Abstract
Purpose
Outpatient palliative care clinics are essential for early symptom management in patients with advanced cancer. Few outpatient programs are available in the Middle East. In this prospective study, we examined the symptom changes among cancer patients seen at a palliative care clinic in Jordan.
Methods
Patients with advanced cancer who had an outpatient palliative care consultation and not delirious were enrolled. The Edmonton Symptom Assessment System (ESAS), Karnofsky Performance Scale (KPS), and Memorial Delirium Assessment Scale (MDAS) were collected at consultation and follow up visit 14–34 days later. We compared symptom changes using paired t test.
Results
Among the 182 enrolled patients, the average age was 53 years, 47 % were females, and 95 % had stage IV cancer. The median duration between the two clinic visits was 21 days (interquartile range 15–28). KPS decreased between visits (mean 68 vs. 66 %, P = 0.004). ESAS pain (5.9 vs. 5.1, P = 0.004) and sleep (4.6 vs. 4.1, P = 0.007) improved significantly over time. The remaining ESAS symptoms decreased in intensity, albeit not statistically significant. Among patients who presented with moderate to severe symptom intensity, pain (7 vs. 6, P < 0.0001), fatigue (7 vs. 6, P = 0.003), nausea (7 vs. 4, P < 0.0001), depression (7 vs. 5, P = 0.0008), anxiety (7 vs. 5, P < 0.0001), drowsiness (6 vs. 5, P < 0.001), appetite (7 vs. 6, P = 0.0007), well-being (7 vs. 6, P < 0.0001), dyspnea (6 vs. 5, P = 0.0006), and sleep (7 vs. 5, P < 0.0001) all improved significantly.
Conclusions
Our outpatient palliative care consultation was associated with improvement in ESAS, particularly for patients who presented with moderate to severe symptoms. Further studies are needed to examine predictors of symptom response, longer term outcomes, and how to improve access to outpatient palliative care in the Middle East.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Assessment and treatment of physical and psychosocial symptoms are essential components of high quality palliative care practice [1]. Despite advances in cancer diagnostics and therapeutics, symptoms remain a major source of distress to patients with cancer and often are not well addressed [2, 3]. Most patients with cancer have multiple symptoms including pain, anorexia, fatigue, shortness of breath, and anxiety. Symptoms can often worsen at the end-of-life, requiring significant attention and proper management [4, 5].
In Jordan, more than 6000 patients are diagnosed with cancer every year. In 2012, more than 2000 patients died of cancer. Palliative care provision and access remain limited [6, 7]. The palliative care program at King Hussein Cancer Center (KHCC) consists of an outpatient clinic, an inpatient consultation service, a palliative care unit, and home palliative care program. The symptomatology associated with cancer and the effect of palliative care on symptom control have not been reported in Jordan. A better understanding of the impact of palliative care on symptom burden may help us to improve the delivery of care for our patients.
In our study, we examined the symptom changes among cancer patients seen in a palliative care clinic in Jordan and identified the possible factors for such a change. We hypothesize that the palliative care team has a positive impact on patients with advanced cancer who presents to our outpatient palliative care clinic with distressing symptoms.
Methods
Study design/eligibility/setting
This is a secondary analysis of a prospective international longitudinal study to examine the minimal clinically important difference for the Edmonton Symptom Assessment Scale (ESAS) [8]. We included patients who were 18 years and older, had advanced cancer, and seen in outpatient palliative care clinic for consultation. We excluded patients who were delirious (13 or more points on the Memorial Delirium Assessment Scale, MDAS) or refused to participate. Consecutive patients who come to the clinic for the first time and met the eligibility criteria were approached. All enrolled patients were re-evaluated in the follow-up visit scheduled 2 to 4 weeks later. The study was approved by the Institutional Review Board. A written informed consent was obtained from all enrolled patients.
Palliative care clinic at King Hussein cancer center
King Hussein Cancer Center is the largest tertiary cancer center in Jordan. The center treats more than 3500 new cancer patients every year. The palliative care clinic at King Hussein Cancer Center receives consultations from all medical and surgical specialty services. The clinic operates 5 days a week and sees between 10 and 15 patients per day. The average waiting time for an appointment is 3–7 days. Urgent requests are accommodated the same or next day. The clinic is staffed by an interdisciplinary team consisting of palliative care physicians, who are American Board Certified in Hospice and Palliative Medicine, registered nurses trained in palliative care and wound management, and a clinical pharmacist. The team is also supported by a social worker and a spiritual advisor who is called to participate in care plan based on patients’ needs [4, 8]. All patients complete the ESAS on every clinic encounter. All cases are evaluated and discussed with the palliative care physician, who works among the clinic interdisciplinary team to formulate a care plan. Care delivery is guided by the institutional approved clinical practice guidelines. At our clinic, discussions generally focused on symptoms with intensity ≥ 4/10.
Data collection and study instruments
In the first study visit, we assessed patients’ demographics, including age, gender, race, cancer type, and stage. ESAS, MDAS, and Karnofsky performance status (KPS) were documented at both the first and second visits. Patients who were delirious in the second visit did not proceed to completing the study assessments. The study instruments were conducted with the help of a trained research residents, who read the questionnaire to patients and clarified as needed. The research residents received training and continuous monitoring.
ESAS is a simple, valid, and reliable tool [9–12] used to assess the severity of symptoms burden in patients with cancer. ESAS assesses the intensity of 10 common symptoms including pain, shortness of breath, fatigue, nausea, drowsiness, anxiety, depression, feeling of well-being, anorexia, and sleep. Each symptom intensity was recorded in the last 24 h, using an 11-point numeric rating scale of 0 to 10, where zero is no symptom and ten is the worst possible symptom [9, 13, 14].
MDAS is a reliable and valid tool for delirium screening and assessment in cancer patients [15]. It consists of 10-items, including awareness, orientation, short-term memory, attention span, attention, thinking, perception, behavior/delusion, psychomotor activity, and sleep disturbance, each ranging between 0 to 2 points, and a higher score indicating worse delirium. A total score of 13 and more indicates delirium [15, 16].
KPS ranges between 0 % (dead) and 100 % (normal) and is widely used to assess functional status in cancer patients [17, 18].
Statistical analyses
We used descriptive statistics to summarize our data, including mean, median, and standard deviation. Symptom changes were compared using paired t test or parametric test as appropriate. The intensity of symptoms were classified in to four categories: absent (0 score), mild (1–3), moderate (4–6), and severe (7–10). We used the paired t test to examine the differences in ESAS scores, MDAS and KPS between the first and second visit.
To examine symptom change between study visits, we decided to focus on patients who reported moderate to severe symptoms (i.e., intensity ≥ 4) because these patients were more likely to require palliative care interventions. We also examined the degree of change by symptom severity for all patients.
A significance criterion of P ≤ 0.05 was used in the analysis. All analysis was performed using SAS version 9.1 (SAS Institute Inc., Cary, NC).
Results
Patients characteristics
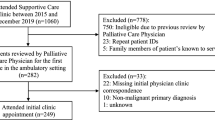
Of the 337 patient screened, 298 (88 %) patients met the eligibility criteria and completed the first visit. Of the 298 patients enrolled, only 182 (61 %) patients completed visit two and were included in the study analysis.
Table 1 summarizes patients’ and disease demographics. The average age was 53 (18–80). Eighty-six (47 %) were females. More than 95 % of patients had a stage 4 cancer. The most common cancers were breast (n = 40, 22 %), lung (n = 37, 20 %), gastrointestinal (n = 31, 17 %), and genitourinary (n = 14, 8 %). The median time between the two visits was 21 days (interquartile range 15–28 days). KPS worsened between visit 1 and 2 (67.8 vs. 65.6 %, P = 0.004). In addition, Table 1 shows the baseline ESAS scores. Vast majority of patients (>80 %) reported pain, fatigue, anorexia, poor wellbeing, and insomnia.
Base line symptoms scores
Table 2 shows the proportion of patients with symptom intensity ≥ 4/10. More than 70 % of patients reported moderate to severe pain, fatigue, and poor well-being.
Symptom changes
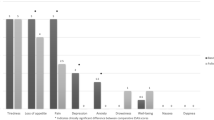
There was a significant reduction in symptom intensity between the first and second visits (Table 2). Among patients who presented with moderate to severe symptom intensity, pain (7 vs. 6, P < 0.0001), fatigue (7 vs. 6, P = 0.003), nausea (7 vs. 4, P < 0.0001), depression (7 vs. 5, P = 0.0008), anxiety (7 vs. 5, P < 0.0001), drowsiness (6 vs. 5, P < 0.001), appetite (7 vs. 6, P = 0.0007), well-being (7 vs. 6, P < 0.0001), dyspnea (6 vs. 5, P = 0.0006), and sleep (7 vs. 5, P < 0.0001) all improved significantly.
Table 3 shows the distribution of symptoms intensity categorized by baseline symptom intensity: absent, mild, moderate, and severe. Patients who had absent and mild symptoms at baseline generally had worsening or exacerbation of symptoms. In contrast, patients who had moderate to severe symptoms had significant improvement (P < 0.0001).
Figure 1 shows that the decrease in symptom intensity in visit 2 as compared to visit 1.
Discussion
This prospective study examined the prevalence of symptoms and impact of a palliative care clinic on symptom change for cancer patients in Jordan. We found that moderate to severe pain, fatigue, feeling of wellbeing, anorexia, insomnia, and drowsiness to be highly prevalent in our patient population. We also found that patients seen at our palliative care clinic had significant improvement in their symptom burden, highlighting the need for effective symptom management programs in the ambulatory setting.
Outpatient palliative care clinics are becoming increasingly common in cancer centers because they facilitate early access to supportive care. In the USA, outpatient palliative care clinics were available in approximately 50 % of National Cancer Institute Designated Cancer Centers and 25 % of non-NCI designated Cancer Centers [19]. In the Middle East, only a few centers have published their experience on palliative care. For example, tertiary care hospital in Saudi Arabia reported that 85.5 % of patients seen at an outpatient palliative care clinic reported pain, with 51 % of them experiencing moderate to severe pain [20]. There are only few specialized palliative care programs in Jordan [6].
To our knowledge, this is the first study to examine the symptom burden and impact of palliative care clinic in Jordan. Compared to other international studies documenting the symptom burden [2, 3, 9, 21–23], our patients had relatively high symptom intensity at baseline with a greater proportion of patients reporting symptom intensity of 4 or greater. This may be related to differences in referral pattern, timing, patient characteristics, culture, scale interpretation, and symptom expression. Future research should examine these issues further.
Our study adds to the growing body of literature to support the role of specialty palliative care clinics in improving patient outcome [24–26]. Because patients with advanced cancer often have significant symptom burden from the time of diagnosis, outpatient clinics allow timely interventions and longitudinal monitoring, thus improving patients quality of life and quality of end-of-life care [25, 27, 28]. Our study is consistent with others demonstrating a benefit in multiple symptom domains in a before-and-after comparison [8]. A retrospective study by Kang and his colleagues conducted at M.D. Anderson Cancer Center evaluating 1612 patients found that moderate to severe symptoms improved while mild symptoms worsened [9]. In another study, Yennurajalingam et al. evaluated 406 patients at an outpatient clinic and reported significant improvement on symptom scores from baseline [22]. Temel et al. also found that patients with metastatic lung cancer who received early palliative care had better quality of life (98.0 vs. 91.5; P = 0.03), fewer depressive symptoms (61 vs. 38 %, P = 0.01) compared to those who only received standard oncologic care [25]. Furthermore, Hui et al. demonstrated that patients seen at outpatient palliative care had improved quality of end-of-life care outcomes compared to those who first had an inpatient palliative care [28].
Routine screening with a validated symptom battery represents one of the cornerstones of symptom management [8, 29, 30]. In this study, the Arabic version of ESAS was used to assess baseline symptom burden and symptom change at our center. Symptoms which were absent or mild at baseline generally worsened. This could be explained by clinical deterioration reflected by declining physical function, the fact that mild symptoms are generally not addressed during the clinical encounter, or floor effect. In contrast, patients who presented with moderate to severe symptoms tend to receive treatment which may explain the level of improvement on the subsequent visit.
One limitation of our study is that we only analyzed patients who completed both visits. Patients who did not return for a second visit due to sickness, death, or refusal were excluded from the analysis. Future studies might include evaluation of those patients who were sick and were followed by home hospice program.
In summary, patients who attended our outpatient palliative care clinic had high symptom burden, and those with moderate and high symptom intensity reported a significant decrease in symptom intensity after the initial consultation. Our study contributes to the accumulating literature demonstrating that outpatient palliative care improves outcome for patients with advanced cancer. Future studies should examine longer term outcomes and how to improve access to outpatient palliative care in the Middle East.
References
Schenck A, Rokoske F, Durham D, Cagle J, Hanson L (2014) Quality measures for hospice and palliative care piloting the PEACE measures. J Palliat Med 17(7):769–775. doi:10.1089/jpm.2013.0652
Walsh D, Donnelly S, Rybicki L (2000) The symptoms of advanced cancer: relationship to age, gender, and performance status in 1,000 patients. Support Care Cancer 8:175–179
Manitta V, Zordan R, Cole-Sinclair M, Nandurkar H, Philip J (2011) The symptom burden of patients with hematological malignancy: a cross-sectional observational study. J Pain Symptom Manag 42:432–442
Seow H, Barbera L, Sutradhar R, et al. Trajectory of performance status and symptom scores for patients with cancer during the last six months of life. J Clin Oncol 29:1151–1158
Hui D, Dos Santos R, Chisholm GB, Bruera E (2015) Symptom expression in the last seven days of life among cancer patients admitted to acute palliative care units. J Pain Symptom Manag 50(4):488–494. doi:10.1016/j.jpainsymman.2014.09.003
Shamieh O, Hui DA (2015) Comprehensive palliative care program at a tertiary cancer Center in Jordan. Am J Hosp Palliat Care 32(2):238–242
Steedman M, Hughes-Hallet T, Knaul F, Knuth A, Shamieh O, Darzi A (2014) Innovation can improve and expand aspects of end-of-life care in low-and middle-income countries. Health Aff 33(9):1612–1619
Hui D, Shamieh O, Paiva C, Perez-Cruz P, Kwon J, Muckaden M, Minjeong P, Yennu S, Kang J, Bruera E (2015) Minimal clinically important differences in the Edmonton symptom assessment scale in cancer patients: a prospective multicenter study. Cancer 121:3027–3035. doi:10.1002/cncr.29437
Kang J, Kwon J, Hui D, Yennurajalingam S, Bruera E (2013) Changes in symptom intensity among cancer patients receiving outpatients palliative care. J Pain Symptom Manag 46:652–660
Moro C, Brunelli C, Miccinesi G, et al. (2006) Edmonton symptom assessment scale: Italian validation in two palliative care settings. Support Care Cancer 14:30–37
Carvajal A, Centeno C, Watson R, Bruera EA (2011) Comprehensive study of psychometric properties of the Edmonton symptom assessment system (ESAS) in Spanish advanced cancer patients. Eur J Cancer 47:1863–1872
Chang VT, Hwang SS, Feuerman M (2000) Validation of the Edmonton symptom assessment scale. Cancer 88:2164–2171
Bruera E, Kuehn N, Miller MJ, Selmser P, Macmillan K (1991) The Edmonton symptom assessment system (ESAS): a simple method for the assessment of palliative care patients. J Palliat Care 7:6–9
Watanabe S, Nekolaichuk C, Beaumont C, Mawani A (2009) The Edmonton symptom assessment system-what do patients think? Support Care Cancer 17:675–683
Breitbart W et al. (1997) The memorial delirium assessment scale. J Pain Symptom Manag 13(3):128–137
Bruera E, Bush SH, Willey J, et al. (2009) Impact of delirium and recall on the level of distress in patients with advanced cancer and their family caregivers. Cancer 115:2004–2012
Schag CC, Heinrich RL, Ganz PA (1984) Karnofsky performance status revisited: reliability, validity, and guidelines. J Clin Oncol 2(3):187–193
Mor V, Laliberte L, Morris J, Weimann M (1984) The Karnofsky performance status scale, an examination of its reliability and validity in a research setting. Cancer 53:2002–2007
Hui D, Elsayem A, Cruz M, Berger A, Zhukovsky D, Palla S, Evans A, Fadul N, Palmer L, Bruera E (2010) Availability and integration of palliative care at US cancer centers. JAMA 303(11):1054–1061
Al-Zahrani O, Eldali A, Zafir Al-Shahri M (2014) Prevalence and severity of pain in cancer patients in an outpatient palliative care setting in Saudi Arabia. Qatar Med J 1:38–45
Strasser F, Sweeney C, Willey J, Benisch-Tolley B, Palmer L, Bruera E (2004) Impact of a half-day multidisciplinary symptom control and palliative care outpatient Clinic in a Comprehensive Cancer Center on recommendations, symptom intensity, and patient satisfaction: a retrospective descriptive study. Pain Symptom Manage 27:481–491
Yennurajalingam SL, Urbauer D, Casper K, Reyes-Gibby C, Chacko R, Poulter V, Bruera E (2011) Impact of a palliative care consultation team on cancer-related symptoms in advanced cancer patients referred to an outpatient supportive care clinic. J Pain Symptom Manag 41:49–56
Yennurajalingam S, Kang J, Hui D, Kang D, Kim S, Bruera E (2012) Clinical response to an outpatient palliative care consultation in patients with advanced cancer and cancer pain. J Pain Symptom Manag 44:340–350
Hearn J, Higginson I (1997) Outcome measures in palliative care for advanced cancer patients: a review. J Public Health 19(2):193–199
Temel J, Greer J, Muzikansky A, Gallagher E, Admane S, Jackson V, Dahlin C, Blinderman C, Jacobsen J, Pirl W, Billings A, Lynch T (2010) Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 363:733–742
Dalal S, Bruera S, Hui D, Yennu S, Dev R, Williams J, Masoni C, Ihenacho I, Obasi E, Bruera E (2016) Use of palliative care services in a tertiary cancer center. Oncologist 21:1–9
Stromgren A, Groenvold M, Pedersen L, Olsen A, Sjogren P (2002) Symptomatology of cancer patients in palliative care: content validation of self-assessment questionnaires against medical records. Eur J Cancer 38:788–794
Hui D, Kim S, Roquemore J, Dev R, Chisholm G, Bruera E (2014) Impact of timing and setting of palliative care referral on quality of end-of-life care in cancer patients. Cancer 120:1743–1749
Cleeland CS, Mendoza TR, Wang XS, et al. (2000) Assessing symptom distress in cancer patients: the M. D. Anderson symptom inventory. Cancer 89:1634–1646
Basch E, Abernethy AP, Mullins CD, et al. (2012) Recommendations for incorporating patient-reported outcomes into clinical comparative effectiveness research in adult oncology. J Clin Oncol 30:4249–4255
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
This research was supported by intermural grant from King Hussein Cancer Center.
Rights and permissions
About this article
Cite this article
Shamieh, O., Khamash, O., Khraisat, M. et al. Impact of outpatient palliative care (PC) on symptom burden in patients with advanced cancer at a tertiary cancer center in Jordan. Support Care Cancer 25, 177–183 (2017). https://doi.org/10.1007/s00520-016-3395-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-016-3395-8