Abstract
Purpose
Cancer cachexia and sarcopenia are frequently observed in cancer patients and associated with poor survival. The majority of studies of cancer cachexia and sarcopenia have been done in patients with solid tumors of different origins, and there are currently no good predictors of the benefit of chemotherapy or factors that predict survival in advanced cancer.
The purpose of our prospective study was to evaluate prevalence of cachexia and sarcopenia using international consensus definition and criteria for diagnosis in patients with diagnosed advanced non-small cell lung cancer (NSCLC) stage IIIB and IV and their relation to chemotherapy toxicity and survival prediction. A secondary aim was to compare several biochemical markers (CRP, IL-6, protein, and albumin) with time to tumor progression in order to assess prognostic value or to guide a treatment.
Methods
Between December 2013 and April 2015, the prospective cohort study of 100 Caucasian patients with advanced NSCLC stage IIIB or IV, who were referred consecutively to Department for Respiratory Diseases “Jordanovac,” was evaluated. Anthropometric measurements and biochemical data (CRP, albumin, protein, IL-6, haemoglobin) together with body composition measurements (total muscle cross-sectional area, lumbar skeletal muscle index) were obtained for each patient before starting with platinum-doublet therapy. Skeletal muscle cross-sectional area at the third lumbar vertebra was measured by computerized tomography, and sarcopenia was defined using a previously published cutoff point. Toxicity was assessed after cycle 1 of treatment and time-to-tumor progression was determined prospectively.
Results
One hundred patients with advanced lung cancer were recruited: 67 were male and median age was 64 years. The median time to disease progression was 187 days. The prevalence of cachexia and sarcopenia in study cohort was 69 and 47 %, respectively. CRP, IL-6, and albumin concentration in cachectic compared to non-cachectic patients demonstrated statistically significant difference (p = 0.020, p = 0.040, p = 0.003). Cachexia and sarcopenia were not found to be predictors of chemotoxicity nor was time to tumor progression. On the contrary, albumin concentration with established cutoff point of 37.5 g/L was clearly proved as the predictive factor of both chemotoxicity (OR (95 % CI) = 0.85; p < 0.001) and survival (HR (95 % CI) = 0.55).
Conclusions
Albumin level has been shown to be more important predictive marker of chemotherapy toxicity and survival than cachexia and sarcopenia are. This approach in clinical settings can be used to guide the choice of oncologic treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to international consensus, cancer cachexia is defined as a multifactorial syndrome characterized by an ongoing loss of skeletal muscle mass (with or without functional impairment) that cannot be fully reversed by conventional nutritional support and leads to progressive functional impairment [1].
Patients who have more than 5 % loss of stable body weight over the past 6 months, a body mass index (BMI) less than 20 kg/m2 and ongoing weight loss of more than 2 %, or sarcopenia and ongoing weight loss of more than 2 % are classified as having cachexia [1].
For a long time, cachexia has been recognized as an adverse effect of cancer with reduced physical function and poorer performance status (PS) [2, 3], increased risk of chemotherapy toxicity [4, 5], and reduced survival [6, 7]. Lung cancer is a leading cause of death worldwide with non-small cell lung cancer (NSCLC) being the most common type of lung cancer. Approximately 60 % of lung cancer patients show significant loss of weight at the time of diagnosis, and more than 10 % of patients die with or from cancer cachexia itself [8].
Besides performance status and weight loss, other factors such as systemic inflammation have been shown to independently predict survival in advanced lung cancer.
Over the last 10 years, the term sarcopenia, as a part of cancer cachexia syndrome, has been recognized as clinically important [7]. It is characterized by progressive loss of skeletal muscle mass, muscle strength, and physical performance [9].
Many different techniques have been used to measure muscle mass, but only few have been incorporated into routine practice of cancer patients: computed tomography (CT), magnetic resonance imaging (MRI), dual-energy X-ray absorptiometry (DEXA) scans, and bioelectrical impedance analysis. The current gold standard in body composition research is CT scan which is a part of many cancer patients’ diagnostic and treatment assessment. NSCLC has strong association with loss of muscle mass (defining 47 % of patients to be sarcopenic) [10].
Systemic inflammation is a common feature of chronic disease [11] and plays a pivotal role in the pathogenesis of cachexia [7, 12]. Imbalance between proinflammatory (TNF-α, IL-1, IL-6, IFN-γ) and anti-inflammatory (IL-4, IL-12, IL-15) cytokines [13] is currently believed to contribute to cachexia. High levels of IL-6 correlate with high C-reactive protein (CRP) values and concomitant body weight loss [14, 15].
The aim of the present study was to obtain prevalence of cancer cachexia and sarcopenia in patients with advanced lung cancer using criteria for definition and diagnosis [1]. The second aim was assessing determinants for chemotherapy toxicity and prognostic factors for survival.
Methods
A prospective study was conducted in Department for Respiratory Diseases “Jordanovac,” University Hospital Center Zagreb, Croatia. The patients were recruited from December 2013 to April 2015. The study cohort included 100 eligible patients of 18 years of age or older diagnosed with advanced NSCLC IIIB or IV stage and scheduled to be treated with systemic chemotherapy (ECOG 0–1).
The following data was obtained: age, sex, cancer type, height, weight, body mass index (BMI), body surface area (BSA), weight loss in preceding 6 months (kg, %), CRP, fibrinogen and IL-6 level, protein, albumin, and hemoglobin concentration.
Body composition measurements
Muscle mass was measured and analyzed from electronically stored CT images, which were obtained for diagnostic purposes during routine clinical practice.
Of 100 eligible patients, 55 had CT images that met the criteria for analysis. Patients who did not have evaluable scans either had no scans on record (n = 16) or a scan >30 days from treatment initiation (n = 2) or scans with no L3 region (n = 27).
The third lumbar vertebra (L3) was determined as a standard landmark, and two consecutive CT images extended from L3 to the iliac crest were appointed to measure the cross-sectional area of the skeletal muscle. The L3 is a well-established landmark across research studies as skeletal muscle and adipose tissue area in this region strongly correspond to whole-body tissue quantities in non-malignant [16–19] and malignant population [20–22].
Skeletal muscle was quantified based on Hounsfield unit (HU) thresholds (−29 to +150) [17]. Boundaries of the respective tissue surfaces were manually delineated and cross-sectional area (cm2) was calculated.
The sum of the cross-sectional areas (cm2) of the L3 region muscles (m.psoas, m.erector spinae, m.quadratus lumborum, m.transversus abdominis, m.obliquus internus, m.obliquus externus, m.rectus abdominis) was computed for each image, and the mean value of the two images was calculated for each patient.
Muscle cross-sectional areas are known to be linearly related to whole-body muscle mass and were normalized for stature to obtain the lumbar skeletal muscle index (LSMI, cm2/m2) [22]. Muscle tissue values measured by CT are reported as total muscle cross-sectional area at L3 (cm2) and muscularity—total muscle area divided by patient’s height squared (cm2/m2), a way of normalizing the value by height.
Sarcopenia was defined using the cut off point for lumbar skeletal muscle index of <39 cm2/m2 for women and <55 cm2/m2 for men proposed by international consensus on cancer cachexia [1, 2].
Biochemical analysis
IL-6 was measured using electrochemiluminescent immunoassay (ECLIA) on the Cobas e411 analyzer (Roche Diagnostics, Mannheim, Germany) using original manufactured reagent calibrators and controls.
Albumin levels were measured using the Bromocresol Purple method, ALB2 on the Cobas c311 analyzer (Roche Diagnostics, Mannheim, Germany).
Toxicity assessment
All our patients had received first-line chemotherapy, including platinum-based chemotherapy with gemcitabine, paclitaxel, or etoposide. Toxicity was graded according to the National Cancer Institute Common Toxicity Criteria, version 2.0. For this study, toxicity profiles were obtained after the first cycle, because patients who had toxicity ≥grade 2 had dose reductions for subsequent cycles.
Time to tumor progression
Time to tumor progression was defined as the number of days of tumor remission after cycle 1.
Statistical analysis
Normality of distributions for quantitative variables was tested using the Kolmogorov-Smirnov test. Normally distributed variables were presented as mean ± standard deviation, and those that were not distributed normally with median and interquartile range. Categorical data were demonstrated as counts and percentages.
For determination of significance of difference between the two groups of quantitative data (laboratory and anthropometric parameters), parametric t test or non-parametric Mann-Whitney test was used.
Differences between categorical variables (chemotherapy toxicity and status according to cachexia or sarcopenia) were tested using Fisher’s exact test.
Pearson correlation coefficient and linear regression analysis were calculated for assessment of association between body mass index and lumbar skeletal muscle index.
Logistic regression analysis was done to identify significant predictors of chemotoxicity classified as GRADE = 2 and higher. History and anthropometric data, together with concentrations of laboratory parameters, were first analyzed using univariate logistic regression. Predictors that were identified as significant were then included into multivariate regression model.
To calculate the median time to progression of the disease, Kaplan-Meier survival curves were presented. Disease progression was identified as the endpoint, while all other possible outcomes were classified as censored data (died, lost, or still in the follow-up process). Hazard ratio was calculated to evaluate if there was a difference in time to progression according to cachexia, sarcopenia, or cutoff values of albumin and CRP.
Level of significance was set at 0.05. Statistical analysis was done using MedCalc for Windows, version 12.5 (MedCalc Software, Ostend, Belgium).
Results
Overall characteristics, anthropometric and demographic characteristics, of 100 patients included are detailed in Table 1. All patients had advanced non-small cell lung cancer (stage IIIB—n = 34, 34 % or stage IV, n = 66, 66 %) and were to begin with systemic oncologic treatment–chemotherapy (ECOG 0, 1). The majority of patients were male (n = 67, 67 %) and the median age was 64 years. At the time of cessation of data collection, 11 patients were lost from the study, and 13 patients were still in the process of therapy. Tumors diagnosed were adenocarcinomas (64 %), squamous-cell carcinomas (34 %), and others. Twelve patients (12 %) had brain metastasis.
The mean weight loss in the previous 6 months was 7 kg or 9.4 %. The mean BMI was 24.5 kg/m2. According to Fearon instruments [1], cachexia was present in 69 patients (69 %). According to World Health Organization (WHO) categories of BMI [23], 40 % of patients were overweight or in class I obesity. Despite considerable weight loss in some patients, proportion of severely underweight patients (BMI < 18.5) was relatively low (4 %).
According to the reference value of lumbar skeletal muscle index determined by CT in the study of Prado et al. [2], an overall of 47 % of patients were sarcopenic. Male patients had statistically significant higher lumbar skeletal muscle area and lumbar skeletal muscle index than females do. A very high proportion of men met the criteria for sarcopenia compared to women: 60.5 % (23/38) and 17 % (3/17), respectively.
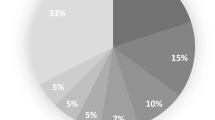
Among male patients who met the criteria as overweight with BMI ≥25.0 [23], N = 26, nine patients (34.6 %) were sarcopenic. Good correlation was observed between BMI and LSMI (r = 0.614) (Fig. 1).
Variation in body composition of the lung cancer population (N = 55). Individual patients are classified by BMI and muscularity. The large variability in muscle index is seen within any given stratum of BMI. Of these patients with BMI classifiable as overweight N = 25, nine patients met the criteria for sarcopenia (33.3 %)
Statistically significant difference was demonstrated between the following parameters in cachectic patients: patients with cachexia had higher CRP (30.1 vs. 6.9 mg/L, p = 0.020) and IL-6 concentration (15.2 vs. 7.5 pg/mL, p = 0.040) but lower albumin (36 ± 5 vs. 40 ± 5 g/L, p = 0.003) and hemoglobin concentration (128 ± 20 vs. 136 ± 17 g/L, p = 0.035) than did non-cachectic patients (Fig. 2). We did not find correlation between IL-6, CRP, and any of the measured anthropometric parameters.
Any adverse event associated with a use of medical treatment that may or may not be considered related to the medical treatment was reported in 43.3 % of patients receiving chemotherapy after the first cycle. There was no statistically significant difference between cachectic and non-cachectic patients in frequency of chemotherapy toxicity. Similarly, there was no difference between sarcopenic and non-sarcopenic patients in the means of chemotherapy toxicity.
Grade ≥2 was observed in 57.2 %, and hematologic toxicity was observed in 33.3 %. We found statistically significant difference between concentrations of measured laboratory parameters and chemotherapy toxicity. Patients with chemotherapy toxicity grade ≥2 compared to patients with no or mild toxicity had significantly lower concentration of protein (60 (59–67) vs. 67 (65–73) g/L; p = 0.001) and albumin (34 (31–37) vs. 39 (35–42) g/L; p = 0.001).
Univariate logistic regression analysis identified significant predictors of chemotherapy toxicity (OR; 95 % CI): weight loss in the preceding 6 months (kg, %) (OR = 1.07, p < 0.049), CRP (OR 1.01, p < 0.028), and concentration of protein (0.89, p < 0.03) and albumin, as the most significant predictor (OR (95 % CI) = 0.85; p < 0.001).
The Kaplan-Meier progression survival curve for 67 patients is presented in Fig. 3. Censored data included patients with lethal end (N = 9), were lost from the study (N = 11), and patients still in the process of management (N = 13). Median time to tumor progression was 187 days. We did not find statistically significant difference between time to tumor progression in cachectic (187 days) and non-cachectic patients (167 days) (Hazard ratio (HR) (95 % CI) = 0.83 (0.48–1.43); p = 0.470). Moreover, there was no statistically significant difference in time to tumor progression in sarcopenic (218 days) and non-sarcopenic patients (209 days).
We did not find any correlation between interlinked parameters: albumin, IL-6, CRP and weight loss, and response to chemotherapy (Cox proportional-hazards regression analysis).
There was no statistically significant difference in survival time between patients with IL-6 concentration in the lower median (IL-6 < 10.9) and those with higher concentration (IL-6 > 10.9); HR = 1.25 (0.76–2.08); p = 0.364. Therefore, we conclude that there was no association between IL-6 and disease progression.
We were not able to identify a reference value for LSMI, as defined by Prado et al. [2], related to cancer-specific outcomes or significant difference to time to tumor progression.
In Fig. 4, we present a comparison of time to tumor progression between groups of patients with albumin concentration lower (<37.5 g/L; N = 46) and higher (>37.5 g/L; N = 47) than median albumin concentration. Time to tumor progression in patients with lower albumin concentration (<37.5 g/L) was 165 days and for patients with higher concentration (>37.5 g/L), it was 255 days. The difference between the times was statistically significant (HR (95 % CI) = 0.55 (0.33–0.90); p = 0.011).
Similarly, analysis of subgroups of patients with CRP level lower or higher than 8 mg/L, evidenced statistically significant difference in survival probability curves. Patients with CRP level lower than 8 mg/L had time to tumor progression of 255 days (128–330), and patients with higher level had 167 days (112–209), the difference being statistically significant (HR (95 % CI) = 0.60 (0.37–0.97); p = 0.040) (Fig. 5).
Kaplan-Meier survival curve of time to tumor progression (days) in patients with higher CRP concentration (≥8 mg/L) and lower (<8 mg/L). Time to tumor progression in patients with lower CRP level (full line) is 255 (128–330) days and 167 days (112–209) in patients with higher CRP level (dotted line)
Discussion
Tumor growth is associated with a vast majority of metabolic changes in humans. They can lead to the onset of anorexia-cachexia syndrome. Cancer anorexia-cachexia syndrome is highly prevalent among cancer patients, especially lung cancer patients. Relevance of cancer cachexia is often overlooked in clinical practice and its better understanding will result in preservation of nutritional status during oncologic treatment.
Cancer cachexia and skeletal muscle wasting (sarcopenia) are frequently observed in NSCLC patients and are associated with poor survival [10, 24]. The incidence rate of cancer cachexia in the study of Kimura et al. [25] was 45.6 %, while in this study, 69 % of patients were cachectic using the same criteria [1]. The same study [25] reported a change in cancer cachexia status (reversal or development) from baseline to 3 months after chemotherapy initiation in 32.4 % of patients, and significantly shorter survival was found in patients with cancer cachexia at baseline.
We did not evidence statistically significant difference in survival curves (time to tumor progression) in patients with and without cachexia or among the group of patients with and without sarcopenia. Possible explanation for that result, we hypothesize, could be high percentage of cachectic and sarcopenic patients in the cohort study.
The classification of BMI does not take into account the composition of weight unit which is clinically important but often misinterpreted. Variations of fat and lean tissue—especially skeletal muscle—are reported in the population [26–28]. Sarcopenia—depletion of skeletal muscle—can occur independently from obesity. Sarcopenia is defined as muscle mass of over two standard deviations below that of healthy adults measured by dual-energy x-ray absorptiometry [29].
Having this quantified, sarcopenia (muscle mass) is another measurable variable in a study of body composition. As a component contributing to cancer cachexia, sarcopenia is incorporated into diagnostic criteria for cancer cachexia. Martin and colleagues [24] reported that low skeletal muscle mass in cancer patients is independently associated with poor survival. The variability of cutoffs in LSMI [2, 24, 25] can be explained due to differences in cancer type, disease stage, ethnicity, cultural background, and BMI. On the contrary, the methods for measuring skeletal muscle mass are similar regardless of the abovementioned inequalities.
The proportion of patients with sarcopenia here outlined was 47 % (26/55), 60.5 % in males and 17 % in females. The difference of lumbar skeletal muscle index between males and females is statistically significant with higher LSMI in males. Using the cutoffs reported in the study of Fearon [1] and Prado [2], we divided our patients into two groups according to sarcopenia status but we did not find statistically significant difference between these two groups in terms of survival curves/time to tumor progression. The reason for that might be in finding the optimal LSMI cutoffs measured by CT based on ethnicity, cancer type, and disease stage, or as we mentioned above, in the high percentage of sarcopenic patients in our report.
Patients with lung cancer constituted the majority (96 %) within the BMI ranges considered normal weight, overweight, and obese. Interestingly, among the patients who have BMI higher than 25.0 (N = 26) (overweight and obese), nine of them were sarcopenic (34.6 %). Sarcopenia was observed in all of the BMI categories shown in Fig. 1 with nearly half of patients (47 %) below the cutoff of muscularity associated with mortality and functional disability [2]. That explained losing muscle tissue while fat tissue is maintained or even gain [2].
A recent study from Kim et al. [30] evaluated prognostic significance of CT-determined sarcopenia in patients with small-cell lung cancer (SCLC). They assessed the prognostic significance of sarcopenia using two different sets of cutoffs in SCLC. When they used the cutoffs proposed by the international consensus of cancer cachexia [1], they found sarcopenia was an independent prognostic factor in SCLC. Patients with sarcopenia had a significantly shorter median overall survival (OS) than did those without. On the contrary, when lower ethnic specific cutoffs were applied [31], the prevalence decreased and its prognostic significance disappeared.
There are no good predictors of the benefit of chemotherapy, although the most established factor for prognosis is performance status. However, performance status is an entirely subjective assessment of a patient’s physical activity and functioning. Along with PS, other factors such as weight loss and systemic inflammation have been reported to independently predict survival in advanced lung carcinoma.
Measures of systemic inflammatory response (CRP) are independent prognostic factors in cancer. A combination of the inflammatory markers CRP and albumin formed the modified Glasgow prognostic score (mGPS). This combination including IL-6 correlates with weight loss. mGPS is the most studied and validated prognostic scoring tool and has clear advantages comparing performance status [32].
Our results, similar to those published by Simmons et al. [32], suggest that the use of weight loss as a prognostic factor in lung carcinoma is less significant than that of performance status and mGPS.
The reason for lacking the impact of cachexia and sarcopenia at baseline on time to tumor progression might be in introduction of nutritional enteral support to the patients with weight loss, thus improving their nutritional status and gaining weight or stopping further loss.
Albumin concentration, CRP, and IL-6 level were discriminatory factors between cachectic and non-cachectic patients. Among the most significant predictors for chemotherapy toxicity that were identified (loss of body weight in 6 months, CRP, protein and albumin level), albumin concentration was the only statistically significant predictor for toxicity. Lower albumin concentration correlated with higher chemotherapy toxicity and poor survival.
One possible limitation of this study was that the prevalence of sarcopenia in the female patients was rather low, when compared to males (17 vs. 60 %). Since females accounted for one third of the participants in the study, it is therefore possible that this might have influenced our results.
Although CT testified as a reliable method for obtaining and calculating muscle area, is easily measurable and reproducible for calculation of muscularity, and usable without expensive software, limitation was demonstrated in defining the cutoffs for LSMI.
Conclusion
Biochemical parameters, CRP, and albumin level were evidenced to be of more important predictive value in chemotherapy toxicity and survival probability than were cachexia and sarcopenia. Further studies are needed to better understand the role of cancer cachexia and sarcopenia in advanced NSCLC and in order to find new nutritional therapeutic approaches and perhaps new concept of cytotoxic drug dosing schedules per kilogram of lean body mass using L3 muscle area measured by CT.
References
Fearon K, Strasser F, Anker DS (2011) Definition and classification of cancer cachexia: an international consensus. Lancet Oncol 12:489–495
Prado CM, Lieffers JR, McCargar LJ, Reinman T, Sawyer MB, Martin L, Baracos VE (2008) Prevalence and clinical implications of sarcopenic obesity in patients with solid tumors of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncol 9:629–635
Moses AWG, Slater C, Preston T, Barber MD, Fearon KCH (2004) Reduced total energy expenditure and physical activity in cachectic patients with pancreatic cancer can be modulated by an energy and protein dense oral supplement enriched with n-3 fatty acids. Br J Cancer 90:996–1002
Prado CM, Baracos VE, McCargar LJ, Reiman T, Mourtzakis M, Tonkin K, Mackey JR, Koski S, Pituskin E, Sawyer MB (2009) Sarcopenia as a determinant of chemotherapy toxicity and time to tumor progression in metastatic breast cancer patients receiving capecitabin treatment. Clin Cancer Res 15:2920–2926
Mir O, Coriat R, Blanchet B et al (2012) Sarcopenia predicts early dose-limiting toxicities pharmacokinetics of sorafenib in patients with hepatocellular carcinoma. PLoS One 7, e37563
Dewys WD, Begg C, Lavin PT et al (1980) Prognostic effect of weight loss prior to chemotherapy in cancer patients. Eastern Cooperative Oncology Group. Am J Med 69:491–497
Fearon KHC, Voss AC, Hustead DS on the bahalf of the Cancer Cachexia Study Group (2006) Definition of cancer cachexia: effect of weight loss, reduced food intake and systemic inflammation on functional status and prognosis. Am J Clin Nutr 83:1345–1350
von Haehling S, Anker SD (2010) Cachexia as a major underestimated and unmet medical need: facts and numbers. J Cachex Sarcopenia Muscle 1:1–5
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, Topinkova E, Vanderwoude M, Zamboni M (2010) Sarcopenia: European concensus on definition and diagnosis: report of the European Working Group on sarcopenia in older people. Age Aging 39:412–423
Baracos VE, Reiman T, Mourtzakis M, Gioulbasanis I, Antoun S (2010) Body composition in patients with non-small cell lung cancer: a contemporary view of cancer cachexia with the use of computed tomography image analysis. Am J Clin Nutr 91:1133S–1137S
Bistrian B (2007) Systemic response to inflammation. Nutr Rev 65(12 Pt 2):S170–S172
Delano MJ, Moldawer LL (2006) The origins of cachexia in acute and chronic inflammatory diseases. Nutr Clin Pract 21(1):68–81
Argiles JM, Lopez-Soriano FJ (1998) Catabolic proinflammatory cytokines. Curr Opin Clin Nutr Metab Care 1:245–251
Walsh D, Mahmoud F, Barna B (2003) Assessment of nutritional status and prognosis in advanced cancer: interleukin-6, C-reactive protein, and the prognostic and inflammatory nutritional index. Support Care Cancer 11(1):60–62
Deans C, Wigmore SJ (2005) Systemic inflammation, cachexia and prognosis in patients with cancer. Curr Opin Clin Nutr Metab Care 8:265–269
Heymsfield SB, Wang Z, Baumgartner RN, Ross R (1997) Human body composition: advances in models and methods. Annu Rev Nutr 17:527–558
Mitsiopoulos N, Baumgartner RN, Heymsfield SB, Lyons W, Gallagher D, Ross R (1998) Cadaver validation of skeletal muscle measurement by magnetic resonance imaging and computerized tomography. J Appl Physiol 85:115–122
Shen W, Punyanitya M, Wang Z et al (2004) Total body skeletal muscle and adipose tissue volumes: estimation from a single abdominal cross sectional image. J Apl Physiol 97:2333–2338
Miller KD, Jones E, Yanovski JA, Shankar R, Feuerstein I, Falloon J (1998) Visceral abdominal-fat accumulation associated with use of indinavir. Lancet 351:871–875
Mourtzakis M, Prado CM, Lieffers JR et al (2008) A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care. Appl Physiol Nutr Metab 33:997–1006
Lieffers JR, Mourtzakis M, Hall KD et al (2009) A viscerally driven cachexia syndrome in patients with advanced colorectal cancer: contributions of organ and tumor mass to whole-body energy demands. Am J Clin Nutr 89:1173–1179
Prado CM, Baracos VE, McCargar LJ, Mourtzakis M, Mulder KE, Reiman T, Butts CA, Scarfe AG, Sawyer MB (2007) Body composition as an independent determinant of 5-fluorouracil-based chemotherapy toxicity. Clin Cancer Res 13:3264–3268
WHO (2000) Obesity: preventing and managing the global epidemic. World Health Organization, Geneva, Switzerland
Martin L, Birdsell L, Macdonald N, Reinman T, Clandinin MT, McCargar LJ, Murphy R, Ghosh S, Sawyer MB, Baracos VE (2013) Cancer cachexia in the age of obesity: skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J Clin Oncol 31:1539–1547
Kimura M, Naito T, Kenmotsu H, Taira T, Wakuda K, Oyakawa T, Hisamatsu Z, Tokito T, Imai H, Akamatsu H, Ono A, Kaira K, Murakami H, Endo M, Mori K, Takahashi T, Yamamoto N (2015) Prognostic impact of cancer cachexia in patients with advanced non-small cell lung cancer. Support Care Cancer 23:1699–1708
Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB (2003) Years of life lost due to obesity. JAMA 289:187–193
Morley JE, Baumgartner RN, Roubenoff R, Mayer J, Nair KS (2001) Sarcopenia. J Lab Clin Med 137:231–243
Cosqueric G, Sebag A, Ducolombier C, Thomas C, Piette F, Weill-Engerer S (2006) Sarcopenia is predictive of nosocomial infection in care of elderly. Br J Nutr 96:895–901
Baumgartner RN, Koehler KM, Gallagher D, Romero L, Hezmsfield SB, Ross RR, Garrz PJ, Lindeman RD (1998) Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol 147:755–763
Kim EY, Ys K, Park I, Ahn HK, Cho EK, Jeong YM (2015) Prognostic significance of CT-determined sarcopenia in patients with small-cell lung cancer. J Thorac Oncol 10:1795–1799
Kim YS, Lee Y, Chung Y et al (2012) Prevalence of sarcopenia and sarcopenic obesity in the Korean population based on the Fourth Korean National Health and Nutritional Examination Surveys. J Gerontol A Biol Sci Med Sci 67:1107–1233
Simmons CP, Koinis F, Fallon MT, Fearon KC, Bowden J, Solheim TS, Gronberg BH, McMillan DC, Gioulbasanis I, Laird BJ (2015) Prognosis in advanced lung cancer—a prospective study examining key clinicopathological factors. Lung Cancer 88:304–309
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the University Hospital Ethics Board.
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Srdic, D., Plestina, S., Sverko-Peternac, A. et al. Cancer cachexia, sarcopenia and biochemical markers in patients with advanced non-small cell lung cancer—chemotherapy toxicity and prognostic value. Support Care Cancer 24, 4495–4502 (2016). https://doi.org/10.1007/s00520-016-3287-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-016-3287-y