Abstract
Purpose
To describe patient- and practice-related factors that physicians report affect their clinical decision to administer prophylactic pegfilgrastim to patients <24 h after completion of a myelosuppressive chemotherapy cycle (i.e., “same-day” pegfilgrastim).
Methods
Oncologists, hematologists, and hematologist-oncologists enrolled in a US national physician panel were invited to participate in a cross-sectional, web-based survey to assess physicians’ reasons for prescribing “same-day” pegfilgrastim. Physicians were screened as eligible if they reported prescribing “same-day” pegfilgrastim within the previous 6 months. The survey assessed physician perspectives and physician-perceived patient/caregiver preferences.
Results
Of 17,478 invited physicians, 386 answered the screening questions; 151 (39.1 %) were eligible, agreed to participate, and completed the survey. Physicians estimated that overall 41.3 % of their patients treated with myelosuppressive chemotherapy received pegfilgrastim and that 31.6 % treated with pegfilgrastim received it on a “same-day” schedule. Approximately 36 % of physicians relied primarily on their clinical judgment when deciding to administer “same-day” pegfilgrastim. The clinical consideration reported most commonly by physicians as moderately or very important when deciding to administer “same-day” pegfilgrastim was previous febrile neutropenia (77.6 %). The most important patient-related consideration in the decision to administer “same-day” pegfilgrastim was patient/caregiver travel distance, and the most important practice-related consideration was the burden to the physician’s practice of “next-day” administration (vs. same-day), reported by 84.7 % and 65.1 % of physicians as moderately or very important, respectively.
Conclusions
While clinical judgment, patients’ risk factors, and practice burden were principal influences favoring “same-day” pegfilgrastim administration, physician-perceived patient preferences and logistical barriers also have important roles in this decision.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
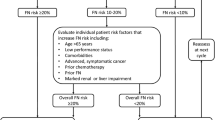
Myelosuppressive cancer chemotherapy can be complicated by the occurrence of febrile neutropenia (FN), characterized by fever associated with a low neutrophil count (absolute neutrophil count either <500 or <1000/μL and predicted decline to ≤500/μL over the next 48 h [1]). Although the myelotoxicity of different chemotherapeutic regimens used in clinical practice is the single most important predisposing factor for overall FN risk, clinical guidelines recognize that both patient characteristics and the type of tumor also affect FN. As such, FN incidence during myelosuppressive chemotherapy (first or all cycles) across tumor types and patient populations has been shown to vary considerably (e.g., 6 % to greater than 50 % [2–4]). FN usually prompts hospitalization and treatment with parenteral broad-spectrum antimicrobials, with significant risk of death and substantial direct and indirect costs [1, 5–7].
Myeloid growth factors are indicated to decrease the incidence of FN in patients with nonmyeloid malignancies who are receiving myelosuppressive anticancer drugs associated with a clinically significant incidence of FN. Neulasta (pegfilgrastim), which was first approved by the US Food and Drug Administration (FDA) in 2002, is a long-acting form of granulocyte colony-stimulating factor (G-CSF) supplied in prefilled syringes and per recommendations, is administered as a single subcutaneous injection of 6 mg once per chemotherapy cycle.
The current FDA-approved prescribing information states that pegfilgrastim should not be administered in the period between 14 days before and 24 h after administration of cytotoxic chemotherapy, and current guidelines recommend that pegfilgrastim be administered either 1-3 (American Society of Clinical Oncology, ASCO) or 1-4 (National Comprehensive Cancer Network, NCCN) days after chemotherapy [1, 8, 9]. Despite these dosing recommendations, a recent US health care claims database analysis of 69,509 patients who received pegfilgrastim prophylaxis with myelosuppressive chemotherapy for selected solid tumors found that pegfilgrastim was administered on the same day as chemotherapy (“same-day” pegfilgrastim) in 13.4 % of the first cycle of chemotherapy [10]. Evidence regarding the efficacy and safety of this practice is inconclusive [11–20]. A study of neutropenia outcomes related to the administration of “same-day” pegfilgrastim found that the duration of severe neutropenia was longer but statistically non-inferior in patients treated with “same-day” pegfilgrastim compared with those treated with “next-day” administration [11]. Current ASCO recommendations, citing these findings, conclude that “clinicians should not be prohibited from using ‘same-day’ pegfilgrastim if it provides the only feasible means of CSF administration for certain patients” [9]. Current NCCN Guidelines (Version 1.2015) for the use of myeloid growth factors also note that “…same-day administration of pegfilgrastim can be considered in certain circumstances…” However, this guideline also notes that “the recent FDA approval of a delivery device that can be applied on the same day as chemotherapy and set to deliver the full dose of pegfilgrastim the following day is an alternative to ‘same-day’ administration for patients who cannot return to the clinic for ‘next-day’ administration of pegfilgrastim” [21].
Little is known about physicians’ underlying reasons for prescribing “same-day” pegfilgrastim [22]. Therefore, a cross-sectional, web-based physician survey was conducted to characterize physicians’ reasons for prescribing “same-day” pegfilgrastim and to explore the key factors associated with prescribing “same-day” pegfilgrastim.
Methods
Questionnaire development
A survey questionnaire was developed using standard survey methodology principles to pose questions eliciting data on the study objectives [23, 24]. The questionnaire, eligibility screener, and informed consent form (ICF) underwent cognitive pretesting to ensure consistent interpretation among respondents and the intended meaning of each question to identify and reduce potential sources of measurement error [24, 25]. The questionnaire was updated following the cognitive pre-test with new and/or revised questions and response options as a result of the interviews. Definitions of “same-day” pegfilgrastim (the prophylactic administration of pegfilgrastim to a patient less than 24 h after completing a cycle of myelosuppressive chemotherapy) versus “next-day” pegfilgrastim (the prophylactic administration of pegfilgrastim to a patient 24–72 h after completing a cycle of myelosuppressive chemotherapy) were developed following this process and provided to the respondents in the survey instrument. Respondents were presented with separate lists of clinical considerations, patient-related factors, and practice-related considerations and asked to indicate the importance of each item as “not at all important,” “a little important,” “moderately important,” or “very important” in their decision to administer “same-day” pegfilgrastim.
Subject selection and data collection
Physicians in the USA who administer “same-day” pegfilgrastim as myelosuppressive chemotherapy were identified and recruited from a pre-existing physician panel. The panel comprises physicians who provide direct patient care in the USA in a wide variety of clinical settings and who have agreed to participate in online research about health care-related issues. Potentially eligible US-based medical oncologists, hematologists, hematologist-oncologists, and other oncologists (n = 17,478) who belong to the panel were sent an e-mail invitation that included a link to the secure web-based screening questions and survey. To be eligible, physicians had to have prescribed the administration of “same-day” pegfilgrastim to any of their patients within the previous 6 months and to provide informed consent to participate in the survey. Respondents who met the eligibility criteria were directed to the beginning of the survey. All study documents, including the initial invitation letter, informed consent form, and honoraria were approved by RTI International’s institutional review board.
The data collected were de-identified (e.g., participating physician’s name and e-mail were not included in the database). The survey targeted recruitment of to up to 150 eligible physicians. As this was an exploratory study, the sample size was based on feasibility assessment and general consideration of the precision of percentage estimates rather than a formal power calculation.
Assessment of outcomes
Specific demographic information on the physician’s practice type, location, and other characteristics were collected anonymously and used to describe the physicians surveyed. Study variables also included the average number of patients by month being treated by each physician or registered under the physician’s care, the average number of patients currently receiving myelosuppressive chemotherapy and pegfilgrastim per month, and an estimate of the percentage of current patients who are administered “same-day” pegfilgrastim. Other variables were related to the setting in which chemotherapy and pegfilgrastim injections are administered. The outcomes of interest were factors that could influence the physician’s decision to prescribe “same-day” pegfilgrastim such as clinical considerations (e.g., risk factors for FN), practice considerations (such as logistical and administrative challenges), and physician-perceived patient or caregiver preferences (e.g., travel distance for patient/caregiver). Physicians were also asked to evaluate the relative importance of guidelines and scientific evidence relating to use of “same-day” pegfilgrastim. Lastly, physicians were asked to consider categories of potentially influencing factors and to rank them by relative importance (with 1 being the most important) in making treatment decisions.
Statistical analysis
The analysis was descriptive in nature, with summary statistics presented for all variables. Continuous variables were summarized with mean, standard deviation, median, and range values. Categorical variables were summarized with frequencies and percentages with exact binominal confidence intervals for selected endpoints. The analysis of the primary objective was initially planned to describe the enrolled set (i.e., physicians who provided an online informed consent); however, to allow for a more consistent set of respondents across variables, the analysis was conducted in the subgroup of respondents who completed the survey (defined as providing a response to the final survey question). The analysis was performed on observed data—no missing values were imputed. Self-evident corrections were used to set null responses to zeros for three questions in the survey (primary cancer of current patients by cancer type, estimated percentage of pegfilgrastim patients by pegfilgrastim administration setting, and estimated percentage of “same-day” pegfilgrastim patients by cycles administered) that met the 100 % summation criteria.
Results
Study sample of physicians
Invitations were e-mailed from May 29, 2015, through June 26, 2015, to 17,478 potentially eligible oncologists, hematologists, and hematologist-oncologists. Three hundred eighty-six physicians responded to the invitation and were screened. Of the 183 physicians enrolled, 151 (82.5 %) completed the questionnaire and were included in the analysis. Table 1 summarizes the characteristics of the participating physicians and their practices.
The majority of physicians (57.7 %) specialized in hematology/oncology and 38.3 % in medical oncology. The average duration in practice was 14.6 years. Most of the physicians practiced in a private group (39.2 %), at a cancer hospital/referral center (25.0 %), or at other types of academic hospitals/clinics (23.0 %). Physicians were relatively evenly distributed across the major geographic regions of the USA, and the majority (53.7 %) practiced in towns with a population of 250,000 or greater.
The physicians reported seeing an average of 225.3 patients per month. Breast cancer (18.8 %), non-small cell lung cancer (15.3 %), and non-Hodgkin lymphoma (12.5 %) were the most common primary cancer diagnoses of their current patients. The primary setting for administration of chemotherapy included both inpatient and outpatient settings (50.0 %), while 43.9 % reported that it occurred in an outpatient setting, and 6.1 % reported that it occurred in an inpatient setting only. The average number of patients treated with myelosuppressive chemotherapy by each responding physician per month was 91.7 (SD = 76.2).
Patients receiving pegfilgrastim
Physicians estimated on average that 41.3 % of their patients treated with myelosuppressive chemotherapy currently receive pegfilgrastim (either “next-day” pegfilgrastim or “same-day” pegfilgrastim) (Table 2). Among patients treated with pegfilgrastim, 31.6 % received “same-day” pegfilgrastim (~13 % of all patients treated with myelosuppressive chemotherapy).
Approximately 43 % of patients estimated to have received “same-day” pegfilgrastim (~6 % of all patients treated with myelosuppressive chemotherapy) were estimated to have received “same-day” pegfilgrastim during all chemotherapy cycles. The specific proportions by cycle are reported in Table 2.
On average, the majority (67.0 %) of pegfilgrastim injections were reported to be administered in an outpatient setting (office, clinic, or infusion center). Other administration settings are detailed in Table 2. Most physicians did not indicate another type of administration; however, of the 4 physicians who did specify another type, 2 noted the use of a delayed injection device or self-injection kit.
Reasons for “same-day” administration
The clinical considerations reported most commonly by physicians as being moderately or very important in influencing the prescribing of “same-day” pegfilgrastim are depicted in Fig. 1. Previous FN (77.6 %) and the presence of infection or open wounds (70.1 %) were the two most commonly reported considerations that were rated as moderately or very important. Similarly, respondents were asked to indicate the importance of select administrative and logistical challenges when deciding to administer “same-day” pegfilgrastim to patients (Fig. 2). The administrative reasons provided to the respondent consisted of practice considerations of staffing, space, and scheduling. The most common administrative considerations reported as moderately or very important when deciding whether to administer “same-day” pegfilgrastim were burden of prophylactic administration of “next-day” pegfilgrastim (65.1 %) and burden of scheduling a next-day appointment (60.4 %). Eleven physicians reported that other administrative considerations were moderately or very important: patient accessibility, reliability to return the next day, and preference (reported by 5 physicians), travel distance (reported by 2), logistics (by 2), insurance coverage or cost of “same-day” administration (by 2).
When asked to spontaneously report any additional issues or considerations that influenced a decision to administer “same-day” pegfilgrastim or “next-day” pegfilgrastim, 11 physicians mentioned reimbursement and insurance issues, and 6 mentioned a delayed injection device or self-injection kit. Additionally, respondents considered the importance of various patient or caregiver preferences (as perceived by the physician) when deciding to administer “same-day” pegfilgrastim; the preferences most frequently reported as moderately or very important are presented in Fig. 2.
On average, physicians ranked “more practical for the patient” as the most important factor influencing their decision to administer “same-day” pegfilgrastim (mean rank [SD] 3.0 [1.7]). This was followed by “patient has limited transportation access and cannot get to the clinic the next day” (mean rank [SD] 3.2 [1.5]) and “patient is disabled or frail, and multiple clinic visits are impractical” (mean rank [SD] 3.3 [1.5]). On average, “more practical for the practice due to patient scheduling burden/load” was ranked as the least important (mean rank [SD] 4.2 [1.7]).
Physician perspective on “same-day” administration
Respondents chose the most influential factor in their decision to administer “same-day”pegfilgrastim from a list of additional high-level categories of considerations. Results are presented in Fig. 3.
When asked how they would describe the efficacy of “same-day” pegfilgrastim administration compared to “next-day” pegfilgrastim administration, 79.1 % of physicians described “same-day” pegfilgrastim administration as being equally effective as “next-day” pegfilgrastim administration. Approximately 16 % of respondents described “same-day” administration as less effective than “next-day” administration, and 5.4 % described “same-day” administration as more effective than “next-day” administration.
Discussion
The FDA- and EMA-approved instructions for administration of pegfilgrastim recommend that treatment start at least 24 h after cytotoxic chemotherapy, but this study and the findings of [22] indicate that “same-day” pegfilgrastim administration occurs in practice [8, 26]. Although the clinical literature provides conflicting evidence regarding the safety and efficacy of “same-day” pegfilgrastim administration, current clinical practice guidelines suggest that it may sometimes be justified [1, 9]. The present study is the first to assess physician-reported patient- and practice-related reasons for prescribing “same-day” pegfilgrastim and to report the frequency of this practice among physicians who have prescribed “same-day” pegfilgrastim.
Physicians in the present study reported administering pegfilgrastim to about 40 % of their patients undergoing myelosuppressive chemotherapy; an estimated 31.6 % of those patients (or approximately 13 % of all patients treated with myelosuppressive chemotherapy) received “same-day” pegfilgrastim. These survey results reflect similar proportions to the Weycker study using a claims database found “same-day” pegfilgrastim in 13.4 % of first cycles and 13.0 % of subsequent cycles of chemotherapy [10]. “Same-day” pegfilgrastim administration was primarily influenced by physicians’ own clinical judgment, followed by individual patient considerations and published guidelines. Product prescribing instructions, clinical trial data, and other research findings were comparatively less influential in the decision process for this sample.
In addition, the perceived administrative burden associated with scheduling a next-day appointment as well as the actual administration of pegfilgrastim on the next day were rated most important to physicians when making the decision to administer “same-day” pegfilgrastim. Physicians reported that patient-specific clinical factors such as febrile neutropenia, the presence of infection or open wounds, and poor ECOG performance status were most important when deciding whether to prescribe “same-day” pegfilgrastim. Among the patient or caregiver preferences reported by physicians, logistical challenges such as travel distance and method or availability of transportation were rated as most important. Other notable factors include patient or caregiver ability to understand and comply with instructions for self-administration and their desire to avoid additional copays or office visits. Patient or caregiver understanding of and/or compliance with instructions for preparation and administration may have contributed to the small proportion of patients reported to receive their injections at home (Table 2). As physicians reported that the majority of patients were administered pegfilgrastim in the office, clinic or infusion center, it is not surprising that these practical challenges would be important factors in the decision process. Only about a quarter of physicians indicated that individual patient considerations were the primary influence on their decision to administer “same-day” pegfilgrastim, suggesting that while physicians recognize these issues to be important to patients and their caregivers, they may factor into but not outweigh clinical judgment in making this treatment decision.
Despite variable evidence as to the safety and efficacy of “same-day” pegfilgrastim administration, current ASCO and NCCN guidelines do acknowledge “same-day” administration but as a less preferable option to administration 1-3 (ASCO) or 1-4 (NCCN) days following chemotherapy [1, 9]. The 2015 NCCN guidelines state that “same-day” administration is an option in specific situations, but that data is inconclusive and “better options” now exist. The guidelines specifically reference the newly available pegfilgrastim delivery device that allows for same-day application and next-day dosage delivery, noting that “this may be an option for patients who cannot return to the clinic for ‘next-day’ administration of pegfilgrastim” [1]. Likewise, ASCO clinical practice guidelines reflect similar recognition of challenges associated with “next-day” administration, specifically patients that are unable to return to the clinic due to distance or immobility, awareness of but hesitancy towards the use of “same-day” pegfilgrastim and acknowledgement of the automated injection device as a potentially useful alternative [9].
Data from the current study were derived from physicians across the USA, with good distribution across all four major geographic regions. The survey instrument was cognitively pretested to ensure that the intended meaning of each question was effectively communicated and that the interpreted meaning was consistent across respondents. The instrument asked physicians directly about their experiences with “same-day” pegfilgrastim administration and the results reflect the current practice among the sampled physicians. By including only physicians who reported prescribing “same-day” within the last 6 months, the study was able to target a specific population of respondents with the most knowledge surrounding this practice.
However, this study is not without limitations. Physicians agreeing to participate voluntarily in the study may not be representative of all physicians prescribing “same-day” pegfilgrastim. For example, the majority of responding physicians practiced in large cities (population ≥ 250,000). Thus, the results may not accurately reflect the prescribing practice and rationale for practices in smaller cities where travel may be even more difficult. A small sample size prohibited the stratification of results by physician characteristic (e.g., years in practice, specialty, population size), which would have allowed us to test the sensitivity of the study results to demographic characteristics of the responding physicians. Similarly, the survey did not collect information on insurance type (e.g., proportion of patients on Medicaid), which, with a larger sample size, could be an interesting topic for further exploration to determine whether rates of “same-day” use differ. Finally, physician perceptions of patient preferences may not accurately reflect patients’ opinions about “same-day” pegfilgrastim administration.
Conclusions
While clinical judgment was the primary factor influencing “same-day” pegfilgrastim administration, the roles of logistical barriers for patients, such as transportation and disability, are additional considerations for providers. Limiting these barriers may reduce patient and caregiver burden while supporting better compliance with approved instructions for administration of pegfilgrastim. Continued education of patients and physicians on the potentially decreased efficacy of “same-day” administration could increase compliance with regulatory agency approved prescribing instructions and possibly improve patient outcomes. In addition, mechanisms overcoming logistic barriers to “next-day” administration, including self- or caregiver-administration at home or use of a delayed delivery device for “next-day” administration, may be warranted in appropriate patients.
References
National Comprehensive Cancer Network (NCCN). Guidelines on myeloid growth factors, version 1. 2015. http://www.nccn.org/professionals/physician_gls/pdf/myeloid_growth.pdf. Accessed 1 September 2015
Culakova E, Thota R, Poniewierski MS, Kuderer NM, Wogu AF, Dale DC, et al. (2014) Patterns of chemotherapy-associated toxicity and supportive care in US oncology practice: a nationwide prospective cohort study. Cancer Med 3:434–444
Crawford J, Dale DC, Kuderer NM, Culakova E, Poniewierski MS, Wolff D, et al. (2008 Feb) Risk and timing of neutropenic events in adult cancer patients receiving chemotherapy: the results of a prospective nationwide study of oncology practice. J Natl Compr Cancer Netw 6(2):109–118
Kosaka Y, Ray Y, Masuda N, Takano T, Saeki T, Nakamura S, et al. (2015) Phase III placebo-controlled, double-blind, randomized trial of pegfilgrastim to reduce the risk of febrile neutropenia in breast cancer patients receiving docetaxel/cyclophosphamide chemotherapy. Support Care Cancer 23(4):1137–1143
de Naurois J, Novitzky-Basso I, Gill MJ, Marti Marti F, Cullen MH, Roila F (2010) Management of febrile neutropenia: ESMO clinical practice guidelines. Ann Oncol 21((Supplement 5)):v252–v256
Weycker D, Li X, Edelsberg J, Barron R, Kartashov A, Xu H, et al. (2015) Risk and consequences of chemotherapy-induced febrile neutropenia in patients with metastatic solid tumors. J Oncol Pract 10:47–54
Bennett CL, Calhoun EA (2007) Evaluating the total costs of chemotherapy-induced febrile neutropenia: results form a pilot study with community oncology cancer patients. Oncologist 12:478–483
Neulasta (pegfilgrastim). http://www.accessdata.fda.gov/drugsatfda_docs/label/2007/125031s082lbl.pdf. Accessed 1 Oct 2015
Smith TJ, Bohlke K, Lyman GH, Carson KR, Crawford J, Cross SJ, et al. (2015) Recommendations for the use of WBC growth factors: American Society of Clinical Oncology Clinical Practice Guideline update. J Clin Oncol 33:1–16
Weycker D, Wu H, Hagiwara M, Li X, Barron RL (2014) Use of chemotherapy and same-day pegfilgrastim prophylaxis in US clinical practice. Blood Journal 124(21):4825
Burris HA, Belani CP, Kaufman PA, Gordon AN, Schwartzberg LS, Paroly WS, et al. (2010) Pegfilgrastim on the same day versus next day of chemotherapy in patients with breast cancer, non-small-cell lung cancer, ovarian cancer, and non-Hodgkin’s lymphoma: results of four multicenter, double-blind, randomized phase II studies. J Oncol Pract 6:133–140
Skarlos DV, Timotheadou E, Galani E, Samantas E, Grimani I, Lianos E, et al. (2009) Pegfilgrastim administered on the same day with dose-dense adjuvant chemotherapy for breast cancer is associated with a higher incidence of febrile neutropenia as compared to conventional growth factor support: matched case-control study of the Hellenic Cooperative Oncology Group. Oncologia 77:107–112
Cheng C, Gallagher EM, Yeh JY, Earl MA (2014 Apr 16) Rates of febrile neutropenia with pegfilgrastim on same day versus next day of CHOP with or without rituximab. Anti-Cancer Drugs 2014[Epub ahead of print]
Saven A, Schwartzberg L, Kaywin P, Bartlett N, Dean L, Shahin S, et al (2006) Randomized, double-blind, phase 2, study evaluating same-day vs next-day administration of pegfilgrastim with R-CHOP in non-Hodgkin’s lymphoma patients. J Clin Oncol 24(suppl). [Abstract 7570]
Kaufman PA, Paroly W, Rinaldi D (2004) Randomized double blind phase 2 study evaluating same-day vs. next-day administration of pegfilgrastim with docetaxel, doxorubicin and cyclophosphamide (TAC) in women with early stage and advanced breast cancer. San Antonio Breast Cancer Symposium. Breast Cancer Res Treat 88[Abstract 1054]
Lokich JJ (2006) Same day pegfilgrastim and CHOP chemotherapy for non-Hodgkin lymphoma. Am J Clin Oncol 29:361–363
Belani CP, Ramalingam S, Al-Janadi A, Eskander E, Ghazal H, Schwartzberg L, et al (2006) A randomized double-blind phase II study to evaluate “same-day” vs next-day administration of pegfilgrastim with carboplatin and docetaxel in patients with NSCLC. J Clin Oncol 24 (suppl):abstract 7110
Schuman SI, Lambrou N, Robson K, Glück S, Myriounis N, Perarson JM, et al. (2009) Pegfilgrastim dosing on same day as myelosuppressive chemotherapy for ovarian or primary peritoneal cancer. J Support Oncol 7:225–228
Whitworth JM, Matthews KS, Shipman KA, Numnum TM, Kendrick JE, Kilgore LC, et al. (2009) The safety and efficacy of day 1 versus day 2 administration of pegfilgrastim in patients receiving myelosuppressive chemotherapy for gynecologic malignancies. Gynecol Oncol 112:601–604
Billingsley CC, Jacobson SN, Crafton SM, Crim AK, Li Q, Hade EM, et al. (2015) Evaluation of the hematologic safety of same day versus standard administration (24- to 72-hour delay) of pegfilgrastim in gynecology oncology patients undergoing cytotoxic chemotherapy. Int J Gynecol Cancer 25:1331–1336
National Comprehensive Cancer Network NCCN. Clinical Practice Guidelines in Oncology (NCCN) Guidelines®: myeloid growth factors, version 1.2015. http://www.nccn.org/professionals/physician_gls/pdf/myeloid_growth.pdf. Accessed 30 September 2015
Weycker D, Wu H, Hagiwara M, Li X, Barron RL (2014) Use of chemotherapy and same-day pegfilgrastim prophylaxis in US clinical practice. Poster presented at the American Society of Hematology Annual Meeting; December 6–9, 2014. San Francisco, CA
Fowler FJ (2014) Survey research methods. Sage, Thousand Oaks, California
Willis GB (2005) Cognitive interviewing: a tool for improving questionnaire design. Sage, Thousand Oaks, California
Patton M (1990) Qualitative evaluation and research methods, second edn. Sage, Thousand Oaks, California
European Medicines Agency. Neulasta 6 mg solution for injection. Summary of product characteristics. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000420/WC500025945.pdf. Accessed 2 Oct 2015
Acknowledgments
The authors take full responsibility for the content of the paper. Ms. Marion was an employee of RTI Health Solutions during the time the study was conducted. The authors thank Kimberly Davis, MS and Kelly Hollis, MBA (RTI Health Solutions) for their assistance. The authors wish to extend a special thanks to Allen Mangel, MD, PhD (RTI Health Solutions), for provision of technical and scientific guidance while developing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Amgen, Inc.
Rights and permissions
About this article
Cite this article
Marion, S., Tzivelekis, S., Darden, C. et al. “Same-Day” administration of pegfilgrastim following myelosuppressive chemotherapy: clinical practice and provider rationale. Support Care Cancer 24, 3889–3896 (2016). https://doi.org/10.1007/s00520-016-3193-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-016-3193-3