Abstract
Purpose
Dysphagia is a common and debilitating side effect for head and neck cancer (HNC) patients undergoing radiotherapy (RT) with or without chemotherapy ([C]RT) and is associated with nutritional and emotional comorbidities. Emotional sequelae and distress are also known to affect carers of HNC patients. A weekly, joint speech pathology/dietetic (SP/DN) service-delivery model has been employed to manage swallowing/nutritional and associated emotional issues during (C)RT. This study aimed to conduct a service evaluation of the weekly SP/DN clinical model.
Methods
Cross-sectional sampling of core service metrics and perceptions of key stakeholders (70 HNC patients, 30 carers, and 10 clinicians) were collated from the Metro South Radiation Oncology Service in Brisbane, Australia. Data from each source was examined separately and then triangulated.
Results
An average of 28 patients (SD = 5.54) attended SP/DN appointments per week, with 58 % reporting swallowing and/or nutritional issues. Distress was reported by 27 % of patients and 30 % of carers. Clinicians felt able to adequately identify and manage swallowing and nutrition 90 % of the time but only 10 % of the time for distress. Seventy-six percent of scheduled SP/DN sessions were perceived as necessary by either patients, clinicians or both.
Conclusions
Findings demonstrated a third of patients and their carers had a high level of distress during HNC [C]RT, supporting need for the provision of a weekly SP/DN service in a select cohort. However, the routine weekly SP/DN assessment model for all patients undergoing HNC treatment demonstrates the potential for over-servicing. Alternative service-delivery models warrant further evaluation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Patients with head and neck cancer (HNC) undergoing radiotherapy (RT) with or without chemotherapy ([C]RT) often experience severe detrimental impacts to swallowing function both during and long-term post-treatment [1, 2]. Impaired swallowing is associated with not only a multitude of negative health outcomes such as nutritional deficiency, poor physical functioning and fatigue [2–4] but also psychological issues including poor quality of life and distress [5–9]. As such, the presence of dysphagia is recognised as contributory to considerable survivorship burden for patients with HNC [10].
The psychological impacts of dysphagia not only affect HNC patients but can also cause significant psychological burden and distress for their carers. This distress has been shown to be multifaceted [11], typically related to speech and swallowing problems and the presence of feeding tubes, coping styles, reduced vitality and disruptions to daily life resulting from care-giving [9, 12–14]. The growing use of (C)RT for HNC, which is provided on an outpatient basis, has also culminated in a greater burden of care falling on patients and their families to manage side effects and their psychological comorbidities in the home.
In recognition of the severity and complexity of treatment sequelae, international cancer guidelines have highlighted the need for timely speech pathology management of HNC patients during (C)RT to proactively identify and minimise on-treatment complications and side effects and thereby potentially reduce the longevity of survivorship burden [15]. Governing bodies have also begun to advocate for the importance of identifying and specifically managing distress in this population, for both patients and carers, to address the psychological implications of HNC treatment and recovery [16, 17]. Unfortunately, the combined effects of growing patient numbers and insufficient specialist services challenge the translation of such evidence into clinical practice [18, 19].
Thus, it is imperative to scrutinise current “on-treatment” speech pathology service provision in order to help optimise its delivery to HNC patients and carers within current staff and service constraints. International surveys of practice have begun to explore aspects of service delivery and have demonstrated limited consistency of practice. A survey of speech pathologists in the UK demonstrated that the majority of clinicians assessed patients in an on-request manner during treatment, with only 25 % reporting seeing patients in a structured weekly review model [20]. Kriscinuas and colleagues [21] examined USA practices and found that for all institutions except stand-alone cancer centres, clinicians worked with no specific management policies for speech pathology intervention during (C)RT.
Australian research studies have indicated that weekly speech pathology intervention for HNC patients during (C)RT, delivered in a joint clinic with the dietitian (SP/DN), has become commonplace [22, 23]. A 10 % reduction in hospital admissions for treatment-related swallowing and nutritional sequelae was found in early examination of this service delivery approach [24]. Despite these positive early findings, no research to date has systematically examined this clinical model. In particular, there has been limited exploration of the specific nature or characteristics of these SP/DN services, including the extent to which care issues, including patient and carer distress, are managed. There is also an absence of data on whether this level of clinical intensity is required for all patients, whether there is over-servicing or inefficiencies in staff utilisation, and how patients and clinicians perceive this service model.
The objective of the current study was therefore to evaluate the weekly, joint SP/DN service delivery model provided to HNC patients at a tertiary cancer centre in Brisbane, Australia. Specifically, this study aimed to examine the validity and clinical usefulness of this care model through the triangulation of a number of service metrics including the perspectives of key stakeholders (patient, carer and clinician).
Methods
Participants and facility
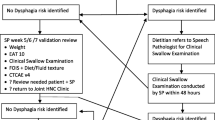
A cross-sectional sample of HNC patients, their carers and clinicians were recruited from the Metro South Radiation Oncology Service (MSROS), a tertiary referral centre hosted across the Princess Alexandra Hospital and Mater Hospital campuses in Brisbane, Australia. MSROS provides a weekly, 30-min joint face-to-face SP/DN service to HNC patients identified as high risk for developing swallowing and/or nutritional difficulties during (C)RT (i.e. any patient receiving a radical course of RT [>60 Gy]), as determined by the treating radiation oncologist.
The study involved the collection and subsequent triangulation of data obtained from four different sources. This included information regarding service characteristics of the SP/DN sessions delivered during the data collection period, as well as responses from the three (3) consumer groups detailed below, who either received or provided SP/DN services during this time.
Inclusion criteria were (1) any patient diagnosed with HNC requiring SP/DN intervention sessions during (C)RT, (2) any carer who attended these appointments with their family member/significant other and (3) any clinician providing speech pathology or dietetic services to HNC patients during the time of the study. Patients and carers were only excluded if they exhibited severe cognitive deficits or non-English reading/writing skills, which would prevent informed consent. Ethical approval was obtained from the Metro South Human Research Ethics Committee in Brisbane, Australia (HREC/13/QPAH/437). Written informed consent was obtained for all eligible patients and carers at time of recruitment. Clinicians’ consent was obtained at the outset of the study before patients and carers were approached.
Procedure
Data were collected prospectively across six, intensive 2-week data collection periods (total of 12 weeks in a 10-month period), with 5–6-week wash-out periods to ensure patients and carers were not recruited more than once. Eligible patients were identified by review of weekly clinic lists and approached sequentially. Service data pertaining to the number of patients scheduled for joint SP/DN appointments, unscheduled/emergency appointments and did-not-attends (DNAs) or rescheduled appointments per week were collected from the electronic patient booking system. Data on the number (in full-time equivalent, [FTE]) of SP and DN clinicians providing services to these patients was also recorded.
Patients and carers were recruited immediately prior to a scheduled SP/DN review session. Participants were not recruited in their initial SP/DN education session as they would not have had the opportunity to form opinions on the SP/DN service. Demographic data regarding patients’ age, gender, TNM stage, treatment type (including concomitant chemotherapy or surgery) and number of completed radiotherapy fractions at the time of recruitment were retrieved from medical records. Immediately prior to their scheduled SP/DN session, patients were asked three questions regarding (1) their perceived need to attend the scheduled SP/DN session to address aspects of swallowing and/or nutrition, (2) if they felt generally distressed or concerned for any reason and (3) whether they wanted to discuss these concerns with a healthcare practitioner. Carers responded to two questions including their perceived level of distress/concern and whether they wanted to discuss these with a healthcare practitioner. All questions were in yes/no format with free text space for participants to elaborate if they desired.
Immediately following the scheduled SP/DN session, the clinicians’ perspectives were obtained (yes/no question) regarding whether they provided any specific speech pathology or dietetic intervention for swallowing and/or nutrition during the session and therefore whether the session was deemed necessary. Clinicians also completed a short survey (seven questions using 5-point Likert scale responses: Never, Rarely, Half the time, Most of the time, Always) at the commencement of the study period regarding current practice patterns of combined SP/DN services, including how frequently aspects of swallowing, nutrition and patient and carer distress were managed in a typical SP/DN session, and how often clinicians felt they had adequate time to manage these aspects of care.
Statistical analysis
Data from each of the four sources (service metrics, patient, carer and clinician perceptions) were analysed separately first, then the information was triangulated to expose the relationships between the four data sources. Descriptive statistics were used to analyse the service metrics and patient-, carer- and clinician-reported information. Clinician questionnaire data obtained from the 5-point Likert scales were collapsed from five levels to three (Most of the time and Always were combined, Half the time remained a category in itself, and Rarely and Never were combined) then analysed descriptively. As part of data triangulation, agreement between the patients’ and clinicians’ perceived need to attend scheduled SP/DN sessions were examined using percentage exact agreement.
Results
Service metrics
During the study period, 1.2 FTE SP and 1.9 FTE DN were involved in providing weekly SP/DN services to HNC patients during (C)RT. These weekly review appointments represented the majority (M = 41 %, SD = 7.94 %) of the clinicians’ caseload per week, with other commitments including SP/DN initial education sessions (10 %), single discipline appointments (i.e. SP only or DN only) (27 %), SP/DN post-treatment sessions (10 %), phone reviews (9 %) and administrative tasks. A mean of 28 patients (SD = 5.54) was scheduled for joint SP/DN services per week, across both campuses of MSROS. An average of 5.5 sessions (SD = 2.58) per week (18 %) were cancelled by clinicians, due to multiple reasons such as inpatient admissions, conflicting scheduling and staff leave; 1.5 sessions per week (SD = 0.54; 5 %) were unscheduled (emergency) appointments, and less than 1 session per week (M = 0.67; SD = 0.82; 2 %) was rescheduled. Patient non-attendance was low with an average of only 2.17 sessions (SD = 2.32) per week recorded as DNAs.
Patient data
Patient (n = 70) demographic data is shown in Table 1. The majority of the patient cohort was male, aged in their mid-60s. The majority of patients had locally advanced oral/oropharyngeal and cutaneous squamous cell carcinomas (SCCs) of the HN, mainly managed with multimodality treatment. Cross-sectional sampling obtained data from most patients in the mid-late stages of RT, as denoted by the number of treatment fractions completed at time of recruitment (Table 1). The overall prevalence of patient-reported swallowing and/or nutritional issues was 58 % (n = 41). General distress or concern was reported by 27 % (n = 19) of sampled patients. Of these, 42 % (n = 8) expressed a desire to discuss these concerns with a healthcare practitioner. Patient responses specifying the nature of their distress cited (1) treatment side effects and recovery, (2) general anxiety or previous anxiety/trauma, (3) issues with communication function and (4) weight loss as areas of particular concern.
Carer data
Recruited carers (n = 40) were typically family members, including spouses, partners and offspring. In carers, the prevalence of reported distress was 30 % (n = 9), with 56 % (n = 5) of these wanting to discuss these concerns with a healthcare practitioner. Distress was commonly reported to relate to treatment side effects and patients’ weight loss and fatigue.
Clinician data
Clinicians (n = 10) exhibited a range of clinical experience (M = 9.58 years, range 0.75–23 years), however the majority (n = 7) had less than 2 years of experience in the radiation oncology caseload (M = 2.95 years, range 0.25–12 years). Clinicians’ perceptions of SP/DN service delivery for HNC patients and their carers are summarised in Table 2. With regard to swallowing and nutrition, identification and management of these aspects of care were reported to frequently feature in typical SP/DN sessions. The majority of clinicians also reported that they mostly or always had adequate time to incorporate management of swallowing and nutrition into their joint service. Conversely, the identification and management of patient and particularly carer distress were reported to rarely feature in typical SP/DN sessions. Most clinicians also reported that they rarely or never had adequate time to incorporate appropriate management practices for patient and carer distress into their routine joint service (Table 2).
Data triangulation
Service statistics (average 28 patients per week) and staffing data identified in the current study indicate that the current SP/DN service is resource intensive, requiring almost half the clinical time of a full-time SP and DN position. Overall, 76 % of scheduled SP/DN sessions were perceived as necessary by either patients, clinicians or both (Table 3). This high rate of perceived service need corresponds to a low rate of patient DNAs. When directly comparing patient and clinician responses, 51 % of the time both parties agreed that there were issues with swallowing and/or nutrition needing to be addressed in the scheduled session. For 24 % of the sessions, both patients and clinicians agreed that there were no issues with swallowing and/or nutrition requiring a face-to-face session (Table 3). Overall, 31 % of the time clinicians felt that sessions were not required, which when viewed in conjunction with the observed 18 % clinician proactive cancellation rate, suggests potential over-servicing in this area.
When comparing patient and carer data, the prevalence of distress across both groups was similar (27 % and 30 %, respectively). Exploring the patient data intrinsically, the majority of patients (68 %, n = 13) who reported a level of distress also reported swallowing and/or nutritional difficulties. Patients and carers showed similarities in what they cited as contributing factors to their distress (e.g. side effects and weight loss), however, only five patient/carer dyads reported distress concurrently. Despite both patient and carer groups reporting levels of distress, clinicians reported that distress management rarely featured in typical SP/DN sessions and there was inadequate time to incorporate appropriate intervention into their service. Clinicians perceived limited potential to address these psychological issues concurs with the service data which demonstrates the already highly demanding nature of this clinical model.
Discussion
The aim of the current study was to evaluate the provision of a weekly SP/DN service model to HNC patients during (C)RT. Collated service metrics have demonstrated that the current model employed by MSROS is a time and resource-intensive service for SP and DN clinicians. This is consistent with the UK HNC service evaluation by Roe et al. [20], which reported that limited resources and staffing was an area of concern for many SP clinicians managing this population. This also echoes the perceptions of clinicians in the current study, who reported that they did not have enough time and resources to manage patient and carer distress as an additional service burden to providing swallowing and nutritional intervention. Such findings suggest that further staffing and resource allocation would be required if the current weekly service model was to holistically address patients’ psychological issues and additional needs of carers.
The current data demonstrate a clear clinical need for the provision of SP/DN services to HNC patients receiving (C)RT. Overall, over three quarters of scheduled sessions were perceived as necessary by patients and/or clinicians to manage issues relating to swallowing and/or nutrition. This is not surprising, given that dysphagia, mucositis, xerostomia and changes in taste and appetite are well-recognised sequelae during (C)RT and often and result in weight loss, requiring SP/DN intervention [25]. The low rate of patient DNAs supports that patients perceive the SP/DN service as valuable throughout their treatment. The low rate of emergency sessions and unplanned admissions also suggests that the regular contact provided through this model of care is ensuring that patients remain closely monitored and well supported throughout (C)RT, avoiding the need for emergency medical management.
Overall, the agreement between patient-report and clinician judgement was high, suggesting that patients were generally aware of changes in their side effects and whether they needed support from the scheduled SP/DN session. Previous research in the field of patient-reported outcome measures have reported that whilst the perceived relative severity of symptoms may vary between patients and clinicians, their overall perspectives on treatment progression are each clinically meaningful and complementary [26]. The current study supports these findings.
Exploratory sub-analysis of discordance between patient-report and clinician judgement revealed that the a proportion of cases where patients felt the session was unnecessary, occurred in the beginning weeks of (C)RT. In these cases, the clinicians likely understood the session was necessary for providing ongoing patient education, however patients were not experiencing any significant side effects impacting swallowing or nutrition. In addition, some sessions may have been needed to provide intervention for issues other than swallowing and nutrition, such as laryngectomy management. Conversely, when analysing the cases where clinicians did not consider the session necessary, half of the patients had reported distress or a desire to discuss concerns with a health worker. In these cases, patients may have desired the session for general support regarding treatment progression, rather than intervention specific to swallowing or nutrition.
Despite the largely positive data supporting the weekly SP/DN service model, the finding that 24 % of scheduled sessions were deemed “not required” by both patients and clinicians suggests the potential for over-servicing. The finding that an additional 18 % of appointments were proactively cancelled suggests that clinicians may have already begun to recognise and respond to potential over-servicing and perhaps warrants review of current clinical prioritisation guidelines. Examination of the identified extraneous sessions revealed that they were not confined to any particular stage in the (C)RT treatment process and did not only occur in the early stages of the radiation course (weeks 2–3), when radiation toxicities are typically less severe. Rather, they appeared to be specific to individual patients’ experiences, with 35 % of “unnecessary” sessions occurring in the later weeks of (C)RT. Indeed, there is growing awareness of the varied nature of patients’ responses to (C)RT and its toxicities [27, 28]. This suggests that a one-fits-all approach to service delivery may not be the most efficient way to provide speech pathology/dietetic intervention to this population.
Whilst the nature of service evaluation research requires the collection of information from multiple sources to inform analysis, a recognised limitation in this study is the relatively limited data from each source. It is acknowledged that more detailed analyses, particularly of patient and clinicians perceptions, could have provided greater insights into various factors such as non-attendance and discrepancies between consumer viewpoints. Further research using qualitative approaches may be beneficial to substantiate and expand the scope of the current findings.
In regard to the prevalence of distress, results from the current study are aligned with previous research, with 27 % of sampled patients reporting a level of distress, consistent with that reported by Verdonck-de Leeuw et al. [9]. In the current study, distress was commonly co-reported with concerns regarding swallowing and/or nutrition. This intrinsic link between eating and psychological well-being has been well established in previous literature [10, 29], with Nguyen et al. [7] reporting a correlation between the severity of (C)RT-induced dysphagia and the degree of morbidity to quality-of-life, anxiety and depression in HNC patients. Carer-reported distress in the current study was slightly higher than the 20 % reported by Verdonck-de Leeuw et al. [9]. Interestingly, only five patient/carer dyads reported distress concurrently. This was also demonstrated by Verdonck-de Leeuw et al [9], in which only 10 % of patients and carers simultaneously recorded clinical levels of distress, using the Hospital Anxiety and Depression Scale (HADS). These findings suggest that whilst there is likely to be a relationship between the quality-of-life of the HNC patient and their carer, distress and burden resulting from care-giving is a separate entity and thus requires separate considerations for its management [11, 30].
Despite the recognition of distress as the “sixth vital sign” [31], clinician perceptions of the current clinical model revealed minimal servicing for psychological aspects of care, with the management of patient and particularly carer distress not routine. Recent research and policy guidelines for distress management advocate for the inclusion and education of multidisciplinary oncology team members, including allied health professionals, in identifying signs of potential patient distress. This distress can then be appropriately managed by licensed mental health professionals, social workers and counselling services [17, 32]. Furthermore, it is considered within the scope of practice for speech pathologists and dietitians to provide psychological support for patients regarding swallowing and nutritional difficulties respectively and identify the need for referral to further services as appropriate [33–35]. The current data suggests that at a minimum, incorporating a means to identify or screen patients/carers and facilitate referral for appropriate distress management needs to be considered.
Overall, although the majority of sessions were deemed necessary, met the needs and concerns of patients, and contributed to a low need for emergency reactive management, the current evidence suggested a degree of over-servicing of swallowing and nutrition. It was also identified that there was a failure to address issues relating to patient and particularly carer distress. A potential solution to address these service shortfalls could be the development of more effective weekly triage techniques to streamline current swallowing/nutritional management practices. Effective triage would allow for enhanced early identification and timely intervention for distress in HNC patients and carers. Routine screening using patient-reported outcome measurements has been proposed as an effective method of monitoring patient functional status over time [36], and use of technology-assisted systems may further enhance feasibility for use in clinical practice [37, 38]. Exploration of these alternate service-delivery models and the use of technology-assisted mediums to provide a clinical adjunct to face-to-face services may assist with triaging HNC patients and carers requiring face-to-face supportive care intervention by the multidisciplinary oncology team. This may ultimately allow for the provision of more holistic and individualised supportive care intervention by relevant professionals whilst improving the efficiency of services during (C)RT treatment. This is an area of future research for the current team.
Conclusion
Findings have confirmed a clear clinical need for the provision of a weekly SP/DN service for HNC patients during (C)RT. However, the service evaluation of this weekly model revealed a degree of over-servicing of swallowing/nutrition and under-servicing of patient and particularly carer distress. Improvements could be made to the current service model or alternative models examined to reduce the numbers of unnecessary sessions and improve the detection of patients and carers requiring psychosocial support. Technology-based triaging systems may be one way to achieve such enhancements.
References
Langendijk JA, Doornaert P, Verdonck-de Leeuw IM, Leemans CR, Aaronson NK, Slotman BJ (2008) Impact of late treatment-related toxicity on quality of life among patients with head and neck cancer treated with radiotherapy. J Clin Oncol 26(22):3770–3776
van der Molen L, van Rossman MA, Burkhead LM, Smeele LE, Hilgers FJ (2009) Functional outcomes and rehabilitation strategies in patients treated with chemoradiotherapy for advanced head and neck cancer: a systematic review. Eur Arch Otolaryngol 266:889–900. doi:10.1007/s00405-008-0817-3
Caudell JJ, Schaner PE, Meredith RF, Locher JL, Nabell LM, Carroll WR, Magnuson JS, Spencer SA, Bonner JA (2009) Factors associated with long-term dysphagia after definitive radiotherapy for locally advanced head-and-neck cancer. Int J Radiat Oncol Biol Phys 73(2):410–415
Isenring E, Zabel R, Bannister M, Brown T, Findlay M, Kiss N, Loeliger J, Johnstone C, Camilleri B, Davidson W, Hill J, Bauer J (2013) Updated evidence-based practice guidelines for the nutritional management of patients receiving radiation therapy and/or chemotherapy. Nutr Diet 70:312–324
Gillespie MB, Brodsky MB, Day TA, Lee FS, Martin‐Harris B (2004) Swallowing-related quality of life after head and neck cancer treatment. Laryngoscope 114(8):1362–1367
McQuestion M, Fitch M, Howell D (2011) The changed meaning of food: physical, social and emotional loss for patients having received radiation treatment for head and neck cancer. Eur J Oncol Nurs 15(2):145–151
Nguyen NP, Frank C, Moltz CC, Vos P, Smith HJ, Karlsson U, Dutta S, Midyett FA, Barloon J, Sallah S (2005) Impact of dysphagia on quality of life after treatment of head-and-neck cancer. Int J Radiat Oncol Biol Phys 61:772–778
Semple CJ, Dunwoody L, George Kernohan W, McCaughan E, Sullivan K (2008) Changes and challenges to patients’ lifestyle patterns following treatment for head and neck cancer. J Adv Nurs 63(1):85–93
Verdonck‐de Leeuw IM, Eerenstein SE, Van der Linden MH, Kuik DJ, de Bree R, Leemans CR (2007) Distress in spouses and patients after treatment for head and neck cancer. Laryngoscope 117(2):238–241
Nund RL, Ward EC, Scarinci NA, Cartmill B, Kuipers P, Porceddu SV (2014) The lived experience of dysphagia following non-surgical treatment for head and neck cancer. Int J Speech Lang Path 16(3):282–289
Nund RL, Ward EC, Scarinci NA, Cartmill B, Kuipers P, Porceddu SV (2014) Carers’ experiences of dysphagia in people treated for head and neck cancer: a qualitative study. Dysphagia 29(4):450–458
Manne S, Badr H, Kashy DA (2012) A longitudinal analysis of intimacy processes and psychological distress among couples coping with head and neck or lung cancers. J Behav Med 35(3):334–346
Precious E, Haran S, Lowe D, Rogers S (2012) Head and neck cancer patients’ perspective of carer burden. Br J Oral Maxillofac Surg 50(3):202–207
Girgis A, Lambert S (2009) Caregivers of cancer survivors: the state of the field. Cancer Forum 33(3):164–167
National Comprehensive Cancer Network (2012) NCCN Clinical practice guidelines in oncology: head and neck cancers version 1.2012. http://www.nccn.org/professionals/physician_gls/pdf/head-and-neck.pdf. Accessed 19 March 2015
Lazenby M (2014) The international endorsement of US distress screening and psychosocial guidelines in oncology: a model for dissemination. J Natl Compr Cancer Netw 12(2):221–227
Borras JM, Albreht T, Audisio R, Briers E, Casali P, Esperou H, Grube B, Hamoir M, Henning G, Kelly J (2014) Policy statement on multidisciplinary cancer care. Eur J Cancer 50(3):475–480
Allied Health Professionals Office of Queensland (2012) Discussion paper: allied health staffing in Queensland Health Cancer Care Services. Queensland Health, Brisbane
Health Workforce Australia (2012) The national cancer workforce strategy. http://www.hwa.gov.au/work-programs/workforce-innovation-and-reform/national-cancer-workforce-strategy. Accessed 19 March 2015
Roe JW, Carding PN, Rhys-Evans PH, Newbold KL, Harrington KJ, Nutting CM (2012) Assessment and management of dysphagia in patients with head and neck cancer who receive radiotherapy in the United Kingdom–a web-based survey. Oral Oncol 48(4):343–348
Krisciunas GP, Sokoloff W, Stepas K, Langmore SE (2012) Survey of usual practice: dysphagia therapy in head and neck cancer patients. Dysphagia 27(4):538–549
Lawson NR, Ward EC (2014) Patient support and multidisciplinary management. In: Head and Neck Cancer: Treatment, Rehabilitation, and Outcomes. 2nd edn. Plural Publishing, San Diego, CA, pp 447-492
Maclean J, Ward E, Findlay M, Rees G (2013) Dysphagia and nutritional management in Australia and New Zealand head and neck cancer centers. Dysphagia 28(4):601–601
Riddle B, Davidson W, Elliott R, Balsillie F, Porceddu SV (2005) Collaborative management of acute side effects for head and neck cancer patients receiving radiotherapy. Asia–Pac. J Clin Oncol 1(Suppl):A18
Platteaux N, Dirix P, Dejaeger E, Nuyts S (2010) Dysphagia in head and neck cancer patients treated with chemoradiotherapy. Dysphagia 25(2):139–152
Basch E, Jia X, Heller G, Barz A, Sit L, Fruscione M, Appawu M, Iasonos A, Atkinson T, Goldfarb S (2009) Adverse symptom event reporting by patients vs clinicians: relationships with clinical outcomes. J Natl Cancer Inst 101(23):1624–1632
Meyer F, Fortin A, Wang CS, Liu G, Bairati I (2012) Predictors of severe acute and late toxicities in patients with localized head-and-neck cancer treated with radiation therapy. Int J Radiat Oncol Biol Phys 82(4):1454–1462
Poulsen MG, Riddle B, Keller J, Porceddu SV, Tripcony L (2008) Predictors of acute grade 4 swallowing toxicity in patients with stages III and IV squamous carcinoma of the head and neck treated with radiotherapy alone. Radiother Oncol 87(2):253–259
Wilson JA, Carding PN, Patterson JM (2011) Dysphagia after nonsurgical head and neck cancer treatment patients’ perspectives. Otolaryngol Head Neck Surg 145(5):767–771
Patterson J, Wilson JA (2011) The clinical value of dysphagia pre-assessment in the management of head and neck cancer patients. Curr Opinion Otolaryngol Head Neck Surg 19(3):177–181
Bultz BD, Carlson LE (2006) Emotional distress: the sixth vital sign-future directions in cancer care. Psychol Oncol 15(2):93–95
National Comprehensive Cancer Network (2014) Distress management NCCN clinical practice guidelines in oncology. https://www.nccn.org/store/login/login.aspx?ReturnURL=http://www.nccn.org/professionals/physician_gls/pdf/distress.pdf. Accessed 19 March 2015
American Speech-Language-Hearing Association (2007) Scope of practice in speech language pathology. www.asha.org/policy. Accessed 19 March 2015
Speech Pathology Australia (2003) Scope of practice in speech pathology. http://www.speechpathologyaustralia.org.au/library/Core_Assoc_Doc/Scope_of_Practice.pdf. Accessed 19 March 2015
Brown T, Findlay M, Dincklage J, Davidson W, Hill J, Isenring E, Talwar B, Bell K, Kiss N, Kurmis R, Loeliger J, Sandison A, Taylor K, Bauer J (2013) Using a wiki platform to promote guidelines internationally and maintain their currency: evidence‐based guidelines for the nutritional management of adult patients with head and neck cancer. J Hum Nutr Diet 26(2):182–190. doi:10.1111/jhn.12036
Velikova G, Booth L, Smith AB, Brown PM, Lynch P, Brown JM, Selby PJ (2004) Measuring quality of life in routine oncology practice improves communication and patient well-being: a randomized controlled trial. J Clin Oncol 22(4):714–724
Wall L, Ward E, Cartmill B, Hill A (2013) Technology-assisted screening of patient-reported functional outcomes in the head and neck cancer population: what’s the evidence? Open Access Cancer 1(2):13–20
Abbott J, Teleni L, McKavanagh D, Watson J, McCarthy A, Isenring E (2014) A novel, automated nutrition screening system as a predictor of nutritional risk in an oncology day treatment unit (ODTU). Support Care Cancer 22(8):2107–2112. doi:10.1007/s00520-014-2210-7
Acknowledgments
The authors would like to acknowledge Cancer Council Queensland for their provision of funding to conduct this research. We also acknowledge Bernadette Dutton and the clinical teams across both MSROS sites for their assistance with data collection.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wall, L.R., Cartmill, B., Ward, E.C. et al. Evaluation of a weekly speech pathology/dietetic service model for providing supportive care intervention to head and neck cancer patients and their carers during (chemo)radiotherapy. Support Care Cancer 24, 1227–1234 (2016). https://doi.org/10.1007/s00520-015-2912-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-015-2912-5