Abstract
Purpose
This study investigated the effectiveness of a structured telephone intervention for caregivers of people diagnosed with poor prognosis gastrointestinal cancer to improve psychosocial outcomes for both caregivers and patients.
Methods
Caregivers of patients starting treatment for upper gastrointestinal or Dukes D colorectal cancer were randomly assigned (1:1) to the Family Connect telephone intervention or usual care. Caregivers in the intervention group received four standardized telephone calls in the 10 weeks following patient hospital discharge. Caregivers’ quality of life (QOL), caregiver burden, unmet supportive care needs and distress were assessed at 3 and 6 months. Patients’ QOL, unmet supportive care needs, distress and health service utilization were also assessed at these time points.
Results
Caregivers (128) were randomized to intervention or usual care groups. At 3 months, caregiver QOL scores and other caregiver-reported outcomes were similar in both groups. Intervention group participants experienced a greater sense of social support (p = .049) and reduced worry about finances (p = .014). Patients whose caregiver was randomized to the intervention also had fewer emergency department presentations and unplanned hospital readmissions at 3 months post-discharge (total 17 vs. 5, p = .01).
Conclusions
This standardized intervention did not demonstrate any significant improvements in caregiver well-being but did result in a decrease in patient emergency department presentations and unplanned hospital readmissions in the immediate post-discharge period. The trend towards improvements in a number of caregiver outcomes and the improvement in health service utilization support further development of telephone-based caregiver-focused supportive care interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With earlier hospital discharges and the shift to more outpatient services, family caregivers are taking more responsibility for cancer patient care [1–3]. Reports suggest that family caregivers provide up to 50 % of patient care needs [4], placing significant additional burden on families. Research confirms high levels of psychological distress and unmet supportive care need in cancer caregivers [5, 6]. The transition from hospital to home is a period of high caregiver need [7–9], particularly if the patient is newly diagnosed [3, 10] and/or has advanced disease [3, 5, 11, 12]. At this time that caregivers are dealing with their own feelings, they need to take on significant patient care and additional family responsibilities. They may also be unfamiliar with the cancer care system [9, 13].
There is growing literature highlighting the positive relationship between caregiver and patient outcomes [3, 14, 15]. The importance of cancer caregiver well-being is well recognized at a policy level [14, 16], but caregivers are largely unsupported by the health system [3].
Caring for patients with poor prognosis gastrointestinal (GI) cancers is particularly challenging. These patients have dismal 5-year survival rates, with rapidly declining health and treatment side effects adversely affecting quality of life (QOL) [17], given the rapid disease trajectory, typically transition to a complex caregiving role in the immediate post-hospital discharge period with many caregivers requiring emotional support during this time [9, 18, 19]. Caregivers report high need for practical and patient care information and assistance with navigating the health system at this time [9].
Caregivers of patients with upper GI cancers are at particular risk of experiencing high levels of psychological distress compared with those caring for people with a longer disease trajectory [11]. Caregiver interventions have been shown to improve both patient and caregiver well-being [16]; however, previous caregiver interventions have primarily focused on patients’ care, with caregiver self-care being a secondary outcome [16]. There is also a paucity of information regarding the specific strategies that will best support caregivers of GI cancer patients to improve their psychosocial outcomes.
The primary aim of this multicenter study was to investigate the effectiveness of a standardized, telephone-based intervention to improve caregivers’ QOL in the first 3 months following a patients’ discharge from hospital. Secondary aims included evaluating the intervention’s effectiveness in reducing caregivers’ unmet supportive care need, caregiver burden and distress. The study also aimed to establish whether a caregiver-focused intervention could also indirectly reduce patient distress, unmet need and unplanned hospital presentations and improve overall patient QOL.
Patients and methods
Trial design, ethics and governance approvals
This study was a parallel randomized trial with a 1:1 group allocation. The study received approval from the Sydney Local Health District Human Ethics Committee (RPAH zone) and was registered with the Australian and New Zealand Clinical Trials Registry (ANZCTR 12609000920291). All patients and caregivers received written and verbal information about the study and gave consent to participate.
Recruitment and random assignment
Between April 2010 and March 2013, caregivers and patients starting treatment at one of four metropolitan hospitals in Sydney, Australia, for a newly diagnosed or recurrent primary upper GI cancer, metastatic liver disease, or stage 4 colorectal cancer were recruited to the study. Patients were eligible for the study if they were aged 18 years or more, aware of their cancer diagnosis, were planning to reside in Australia for the next 6 months, had sufficient English language skills to complete study assessments, were not cognitively impaired and could nominate a caregiver primarily responsible for their care. Caregivers were eligible for participation if the patient consented to their participation, they were aged 18 years or older, they had access to a telephone, they had sufficient English language skills to complete study assessments and they were not cognitively impaired.
Patients were recruited during their hospital admission either post-surgery or immediately prior to starting non-surgical treatment. Eligibility was confirmed by the patient’s surgeon. Primary caregivers of consenting patients were recruited either during the patient’s hospital admission or within 2 weeks of patient discharge. If patients or their caregivers refused to participate, patient socio-demographic information such as their age, gender and tumour site were collected to investigate any potential sampling bias between participants and non-participants. No demographic information was collected from non-participating caregivers.
Consenting caregivers and patients separately completed a baseline self-administered questionnaire prior to randomization. The caregiver baseline questionnaire ascertained demographic characteristics, QOL using the Short Form (SF)-12v2, a 12-item QOL questionnaires with two subscales that assess physical and mental well-being. Estimates of reliability for SF-12 physical component scores (PCS) and mental component scores (MCS) are reported as 0.89 and 0.86, respectively [20]; unmet supportive care needs using an early 26-item version of the Partner and Caregiver Supportive Care Needs Survey (SCNS-P&C) that included the subscales psychological and emotional, work and social and information needs. Reliability for these subscales ranges from .88 to .94. [21]: the five subscales of the 26-item Caregiver Reaction Assessment (CRA)—disrupted schedule, financial problems, lack of family support, health impact and impact on self-esteem. Reliability of the subscales ranges from .62 to .83 [22, 23]. Overall distress was measured using the single-item Distress Thermometer [24]. The patient baseline questionnaire included assessment of QOL, unmet supportive care needs and psychological distress using the Functional Assessment of Cancer Therapy—General (FACT-G), a 33-item measure of QOL across five domains (physical, social/family, emotional, functional well-being and relationship with physician) with good reliability (.89) [25]; the Supportive Care Needs Survey—Patient version (SCNS-34), a 34-item measure across five domains of need (psychological, health system and information, physical and daily living, patient care and sexuality needs) with good reliability (.86–.96) [26] and the Distress Thermometer [24]. Type and stage of cancer, treatment received, current or planned referral to palliative care, co-morbidities and length of hospital stay were extracted from hospital medical records and recorded on a standardized clinical data form. Estimated time to complete study questionnaires for caregivers and patients was 20 min.
On receipt of both caregiver and patient baseline questionnaires, participants were stratified by hospital and randomly allocated to a study group (intervention or usual care) using a computer-generated randomization list. Caregivers were contacted by telephone to advise them of their group allocation, and for those participants allocated to the intervention group, the first intervention call was scheduled.
Intervention
The Family Connect intervention comprised a series of four telephone calls to the caregiver nominated by the patient as primarily responsible for ongoing care in the first 10 weeks after the patient was discharged from hospital, a time highlighted in our pilot work as particularly stressful for caregivers [9]. The first call was scheduled to occur within 14 days post-discharge and subsequent calls were scheduled at 4, 6 and 10 weeks post-discharge. Participants could reschedule calls if required within the 10-week intervention. The intervention involved a manualized, standardized assessment of caregiver need across the domains of patient care, maintaining family relationships and emotional and physical self-care, as well as an assessment of information and practical needs [27]. Within each of these domains, the manual provided a list of resources and strategies that might address identified needs, to guide the health professionals delivering the intervention. The resources provided and the level of discussion related to management strategies were tailored to individual caregiver needs. Therefore, in addition to emotional support and discussion of tangible strategies to assist caregivers deal with the challenges associated with caregiving, individualized information related to local patient and/or caregiver support services and practical and financial resources available for caregivers was also provided. Strategies were based on published evidence and clinical experience. The intervention was delivered by experienced health professionals (clinical psychologists with training in clinical aspects of cancer care) who followed intervention protocols and received training in cancer care specific to gastrointestinal cancers as well as telephone communication skills. All intervention calls were recorded. Recordings were used during regular sessions to provide support and further training to intervention staff and for quality assurance purposes to confirm intervention fidelity. Intervention participants (30 %, n = 18) were also interviewed at 3 months to assess intervention acceptability.
Outcome measures
At 3 and 6 months after hospital discharge, separate self-administered questionnaires comprising all measures from the baseline assessment except demographic questions were mailed to caregivers and patients. Additionally, caregivers were also telephoned at both time points to determine patient health service utilization in the preceding 3 months using a standardized telephone interview format developed for the study. Reasons for each contact with health professionals were elicited, and interactions outside of routine follow up protocols were clinically assessed to identify unscheduled contacts with health services.
Statistical analysis
Caregivers and patients in each arm of the intervention were compared descriptively according to CONSORT guidelines [28]. Analyses were conducted on an intention to treat basis. All questionnaires were scored according to coding manuals, and mean values on all outcome measures for each group were compared at 3 and 6 months using regression modelling with group and baseline score as covariates. The effect of caregiver scores on patient outcomes was assessed by multivariate regression. Linear mixed modelling was used to compare the trajectories of outcome measures over time. The proportion of patient presentations to emergency and unplanned hospital readmissions between groups were compared using Fisher’s exact tests. All analyses were conducted using Stata/SE 12.1 and R 3.01.
Missing data
Multiple imputations were used to impute missing data using R 3.0.1. Fifty imputed datasets were created by predictive mean matching using 25 iterations of the chained equation process. The imputed data were imported into Stata and regression models were fit to the imputed datasets.
Sample size
Sample size calculations were based on a difference of 0.5 SD in mean PCS and MCS on the SF-12v2 at 3 months. To detect a moderate effect size with .05 significance and .80 power, we estimated a sample size of 64 caregivers per group, at 3 months.
Results
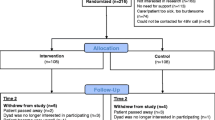
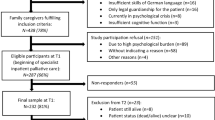
Three hundred eighty five patients were screened for eligibility. Of those found to be eligible, 189 patients and 160 caregivers consented to participate and 128 patient–caregiver pairs completed the baseline questionnaire and were randomized (Fig. 1). Baseline characteristics for caregivers and patients were similar for both groups (Tables 1 and 2). Demographic and clinical characteristics of participating and non-participating patients were similar, although non-participating patients were slightly older (66.6 vs. 62.1 years). The most common reasons for non-participation included caregiver declined/patient or caregiver withdrawal of consent prior to randomization, patient deterioration/death prior to randomization, or inability to contact the nominated caregiver within the study timelines. Higher than anticipated withdrawal rates pre-randomization were due to perceived study burden once the patient was discharged.
Caregiver quality of life
The scores for the mental health (MCS) and physical health (PCS) components of the SF-12v2 QOL scale are presented in Table 3. In both the intervention and usual care groups, mean scores for the mental component of the SF-12v2 QOL scale were considerably lower than standardized population means at all time points and were indicative of poor mental health. At 3 months the mental health score for the intervention group (47.7) was higher than the for usual care group (44.5). This difference was larger than the minimally important difference for the SF-12v2 [20], although did not reach statistical significance (Table 3). Mental health scores in both groups increased by 6 months but remained below general population norms. Overall trajectories are shown in Fig. 2. There were also no significant between-group differences at 3 or 6 months (Table 3) or in overall trajectories (Fig. 2) for the physical health component of the SF-12v2 QOL or between-group differences at 3 or 6 months (Table 3) and trajectories presented in Fig. 2.
Caregiver burden
There were no significant differences between groups at either 3 or 6 months for any of the Caregiver Reaction Assessment subscales (Table 3) in cross-sectional analysis. However, longitudinal assessment of the overall trajectories (Fig. 2) demonstrated significant differences between groups for the subscales of family support (p = .049) and finance (p = .014), with the intervention group reporting greater family support and fewer worries regarding finance compared to the usual care group.
Caregiver distress
At baseline both groups reported distress levels indicative of clinical distress (>4). Distress reduced to below clinical levels at 3 months. Although not statistically significant, by 6 months distress levels in the usual care group had increased to near baseline levels, while intervention group distress remained at 3-month levels (Table 3 and Fig. 2).
Caregiver unmet supportive care needs
Unmet supportive care need was low in both groups at 3 and 6 months, and there were no statistically significant between-group differences. Although not statistically significant, the overall SCNS trajectory for the intervention group indicated reduced unmet need at 3 and 6 months compared to the trajectory for the usual care group (Fig. 2).
Effect of the intervention on patient outcomes
Intervention group caregivers reported fewer patient emergency presentations and unplanned readmissions than usual care group patients in the 3 months after hospital discharge, with 10.2 % (n = 5) of intervention patients reporting a presentation to the emergency department or an unplanned readmission compared to 30.9 % (n = 17) of patients in the usual care group (p = 0.01, Fisher’s exact test). However, this difference was not maintained at 6 months.
QOL scores for patients increased from baseline to 6 months in both groups indicating improvement quality of life (Table 3). However, there were no differences between groups at 3 or 6 months and QOL trajectories were similar. Both groups had similar levels of distress, with no significant between-group differences at 3 or 6 months (Table 3). Levels of unmet need decreased from baseline to 6 months from moderate to low levels of need, although no significant differences between groups were identified (Table 3).
Intervention process evaluation and acceptability
Intervention fidelity was assessed throughout the study and remained high. Mean call length ranged from 32 min at 2 weeks to 17 min at week 10. There were high levels of participation in the intervention calls among caregivers in the intervention group, and participants were able to reschedule calls to maximize the number of participants receiving four calls within the 10-week intervention (Table 4). Qualitative interviews (n = 18) at 3 months confirmed the intervention to be well accepted among caregivers, the timing of calls appropriate to caregiver need and that the telephone-based nature of the intervention was particularly attractive to caregivers with limited time to attend face-to-face sessions. In addition to providing general reassurance, caregivers were able to identify specific areas of need addressed by the intervention.
Discussion
This caregiver-focused supportive care intervention did not demonstrate statistically significant improvements in caregiver mental well-being in the immediate post-hospital discharge period. However, there were fewer concerns about financial issues and greater perceived family support in the intervention group.
Consistent with previous caregiver research [2, 29], caregivers in our study experienced poor mental health and clinical levels of psychological distress compared to population. Differences greater than the minimally important difference for the SF-12v2 measure were observed between the intervention and usual care groups at 3 months; however, this difference failed to reach statistical significance. Previous caregiver intervention studies have also reported only modest changes in anxiety and distress [16], but suggest high levels of caregiver distress and poor mental well-being at diagnosis are negatively associated with longer term caregiver psychological health; thus, even modest improvements may have important long-term consequences [29].
Caregivers in the intervention group reportedly experienced less financial burden and perceived greater family support than those in the usual care group. Previous studies with cancer caregivers have highlighted both finance and managing family relationships to be significant areas of unmet need [30, 31]. Reports also highlight the psychological morbidity associated with financial strain for both patients and caregivers and suggest that caregivers under-report the impact [32]. Our results suggest that provision of information related to financial entitlements available through government and non-government agencies has the potential to reduce the financial burden associated with loss of income and additional expenses that arose during the 6 months after discharge, although in this study, we did not assess whether services were actually taken up by caregivers.
Difficulty communicating and negotiating family roles has been identified as having a detrimental effect on patient and caregiver well-being [33, 34]. The intervention included specific information and strategies to assist caregivers manage family relationships and negotiate support from family and friends. Our results suggest that this discussion empowered intervention participants to articulate their support needs and better manage family relationships. Although we were unable to demonstrate statistically significant differences, our results do suggest that greater support has the potential to improved caregiver well-being.
Despite low levels of unmet need overall, levels of unmet need in the intervention group were lower at both 3 and 6 months compared to the usual care group, although this difference failed to reach statistical significance. This low level of unmet need reported by both caregivers and patients is inconsistent with both the high levels of distress reported and previous research highlighting high unmet need among patients with gastrointestinal cancers and their caregivers [9, 35]. Other studies have also found low unmet need based on the supportive care need survey [27, 36]. The standardized need assessment conducted as part of the intervention highlighted higher levels and a broader range of needs than questionnaire data. Although a formal comparison is beyond the scope of this study, this discrepancy, coupled with the high caregiver distress, suggests that the SCNS does not adequately capture the needs of this caregiver group. Further work to identify more appropriate measures is required.
This study also investigated whether a caregiver-focused intervention could improve patient outcomes. The intervention reduced caregiver-reported patient unplanned readmissions and presentations to emergency departments in the first 3-month post-hospital discharge; however, the support provided to caregivers did not have any measurable impact on patient quality of life, level of unmet supportive care need, or psychological distress. Future interventions focused on educating caregivers to identify and address patient care need have the potential to reduce health system costs. However, our results suggest that there is also a need for interventions that involve both the caregiver and patient if we are to improve patients’ quality of life.
Due to the complexity of the procedures and subsequent impact on patient physical function, unplanned hospital readmission rates after gastrointestinal surgery are higher than for other surgeries [38]. The reduction in unplanned hospital readmissions and presentations to emergency departments in the intervention group at 3 months suggests that the modules of the intervention related to patient care and navigating the health system provided caregivers with sufficient information to identify the need for medical intervention and the appropriate health professional to contact, prior to the need for crisis intervention. Any reduction will therefore have a positive impact for both the patient and the health system more generally.
This study had a number of strengths, including the randomized controlled design, a standardized intervention protocol and ongoing fidelity assessment across the study, high participant retention rates and the inclusion of both caregiver and patient assessments. This study was also one of few that have focused primarily on caregiver rather than patient need. A limitation of the study is that the intervention schedule was designed to minimize further caregiver stress by limiting the number of calls. It is possible that the intervention was not intensive enough to have a significant impact on caregivers at a time when they are experiencing high levels of distress. Recruitment of caregivers is challenging, particularly when patients are diagnosed with poor prognosis tumours [37], and although the study was sufficiently powered to detect a moderate effect on caregiver outcomes, it had insufficient statistical power to assess smaller differences between groups. The sample size also limited our ability to assess the impact of specific demographic variables such as caregiver relationship to the patient. The high level of withdrawal prior to randomization (20 % of caregivers and 32 % of patients) may have resulted from our recruitment methodology and the need for both patients and caregivers to agree to participate in the study. Recruiting patients and their caregivers prior to hospital discharge was a convenient method of recruitment, but those who withdrew did so once they returned home. Reasons for withdrawal were primarily perceived burden of participation and/or the patient being unable to complete study assessments due to their post-surgery frailty. Similar attrition rates are reported in other supportive care studies targeting poor prognosis patient groups and their caregivers [38–40] and highlight the challenging nature of this area of research.
In conclusion, this telephone-based supportive care intervention for caregivers of patients with poor prognosis gastrointestinal cancers did not demonstrate any statistically significant improvements in caregiver mental health, although there were trends toward improvements in caregiver burden domains of social support and reduced worries about finance. The intervention did result in a statistically significant reduction in patient emergency presentations and readmissions in the immediate post-discharge period. These results suggest that further development of this intervention is required if it is to have potential to deliver improvements in care and outcomes.
References
Thomas C, Morris SM, Harman JC (2002) Companions through cancer: the care given by informal carers in cancer contexts. Soc Sci Med 54:529–544
Sharpe L, Butow P, Smith C, McConnell D, Clarke S (2005) The relationship between available support, unmet needs and caregiver burden in patients with advanced cancer and their carers. Psychooncology 14:102–114
Given BA, Given CW, Kozachik S (2001) Family support in advanced cancer. CA Cancer J Clin 51:213–231
Nijboer C, Tempelaar R, Sanderman R et al (1998) Cancer and caregiving: the impact on the caregiver’s health. Psycho Oncol 7:3–13
Soothill K, Morris SM, Harman J et al (2001) Informal carers of cancer patients: what are their unmet psychosocial needs? Health Soc Care Community 9:464–475
Pitceathly C, Maguire P (2003) The psychological impact of cancer on patients’ partners and other key relatives: a review. Eur J Cancer 39:1517–1524
Weaver FM, Perloff L, Waters T (1999) Patients’ and caregivers’ transition from hospital to home: needs and recommendations. Home Health Care Serv Q 17:27–48
Hughes LC, Hodgson NA, Muller P et al (2000) Information needs of elderly postsurgical cancer patients during the transition from hospital to home. J Nurs Sch 32:25–30
Shaw J, Harrison J, Young J et al (2013) Coping with newly diagnosed upper gastrointestinal cancer: a longitudinal qualitative study of family caregivers’ role perception and supportive care needs. Support Care Cancer 21:749–756
Siegel K, Raveis VH, Houts P, Mor V (1991) Caregiver burden and unmet patient needs. Cancer 68:1131–1140
McConigley R, Halkett G, Lobb E, Nowak A (2010) Caring for someone with high-grade glioma: a time of rapid change for caregivers. J Palliat Med 24:473–479
Richardson A, Plant H, Moore S et al (2007) Developing supportive care for family members of people with lung cancer: a feasibility study. Support Care Cancer 15:1259–1269
Driscoll A (2000) Managing post-discharge care at home: an analysis of patients’ and their carers’ perceptions of information received during their stay in hospital. J Adv Nurs 31:1165–1173
Hodges LJ, Humphris GM, Macfarlane G (2005) A meta-analytic investigation of the relationship between the psychological distress of cancer patients and their carers. Soc Sci Med 60:1–12
Goldstein NE, Concato J, Fried TR et al (2004) Factors associated with caregiver burden among caregivers of terminally ill patients with cancer. J Palliat Care 20:38–43
Northouse LL, Katapodi MC, Song L, Zhang L, Mood DW (2010) Interventions with family caregivers of cancer patients: meta-analysis of randomized trials. CA Cancer J Clin 60:317–339
Australian Institute of Health and Welfare & Australasian Association of Cancer Registries Cancer in Australia: an overview, 2012 In Cancer series no. 74. Cat. no. CAN 70.2012, AIHW: Canberra. (accessed 26 April 2014)
Bae J-M, Park J-W, Yang H-K, Kim J-P (1998) Nutritional status of gastric cancer patients after total gastrectomy. World J Surg 22:254–261
Martin L, Lagergren P (2009) Long-term weight change after oesophageal cancer surgery. Br J Surg 96:1308–1314
Maruish ME (ed) (2011) User’s manual for the SF-36v2 health survey, 3rd edn. Quality Metric Incorporated, Lincoln
Girgis A, Lambert S, Lecathelinais C (2011) The supportive care needs survey for partners and caregivers of cancer survivors: development and psychometric evaluation. Psychooncology 20:387–393
Given CW, Given B, Stommel M et al (1992) The caregiver reaction assessment (CRA) for caregivers to persons with chronic physical and mental impairments. Res Nurs Health 15:271–283
McCorkle R, Yost LS, Jepson C et al (1993) A cancer experience: relationship of patient psychosocial response to care-giver burden over time. Psychooncology 2:21–32
Gessler S, Low J, Daniells E et al (2008) Screening for distress in cancer patients: is the distress thermometer a valid measure in the UK and does it measure change over time? A prospective validation study. Psychooncology 17:538–547
Cella D. Functional Assessment of Chronic Illness Therapy (FACIT) Measurement System. Elmhurst Il. http://www.facit.org/
Boyes A, Bonevski B (2004) The supportive care needs survey: a guide to administration, scoring and analysis. Centre for Health Research & Psycho-oncology, Newcastle
Young JM, Butow PN, Walsh J et al (2013) Multicenter randomized trial of centralized nurse-led telephone-based care coordination to improve outcomes after surgical resection for colorectal cancer: the CONNECT intervention. J Clin Oncol 31:3585–3591
Schulz KF, Altman DG, Mohr D et al (2010) CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMC Med 8:18. doi:10.1186/1741-7015-8-18
Northouse L, Templin T, Mood D (2001) Couples’ adjustment to breast disease during the first year following diagnosis. J Behav Med 24:115–136
Lambert S, Jones B, Girgis A, Lecathelinais C (2012) Distressed partners and caregivers do not recover easily: adjustment trajectories among partners and caregivers of cancer survivors. Ann Behav Med 44:225–235
Chen S-C, Tsai M-C, Liu C-L et al (2009) Support needs of patients with oral cancer and burden to their family caregivers. Cancer Nurs 32:473–481
Hanratty B, Holland P, Jacoby A, Whitehead M (2007) Financial stress and strain associated with terminal cancer—a review of the evidence. Palliat Med 21(p):595–607
Maly RC, Umezawa Y, Leake B, Silliman RA (2005) Mental health outcomes in older women with breast cancer: impact of perceived family support and adjustment. Psychooncology 14:535–545. doi:10.1002/pon.869
Dumont S, Turgeon J, Allard P et al (2006) Caring for a loved one with advanced cancer: determinants of psychological distress in family caregivers. J Palliat Med 9:912–921
Viklund P, Wengström Y, Lagergren J (2006) Supportive care for patients with oesophageal and other upper gastrointestinal cancers: the role of a specialist nurse in the team. Eur J Oncol Nurs 10:353–363
Lambert S, Girgis A, Lecathelinais C, Stacey F (2013) Walking a mile in their shoes: anxiety and depression among partners and caregivers of cancer survivors at 6 and 12 months post-diagnosis. Support Care Cancer 21:75–85
Martin RCG, Brown R, Puffer L et al (2011) Readmission rates after abdominal surgery: the role of surgeon, primary caregiver, home health, and subacute rehab. Ann Surg 254:591–597
Schofield P, Ugalde A, Carey M et al (2008) Lung cancer: challenges and solutions for supportive care intervention research. Palliat Support Care 6:281–287
Ostroff J, Ross S, Steinglass P, Ronis-Tobin V, Singh B (2004) Interest in and barriers to participation in multiple family groups among head and neck cancer survivors and their primary family caregivers. Fam Process 43:195–208
Northouse LL, Rosset T, Phillips L, Mood D, Schafenacker A, Kershaw T (2006) Research with families facing cancer: the challenges of accrual and retention. Res Nurs Health 29:199–211
Acknowledgments
The researchers would like to thank the patients and caregivers who participated in this study. We thank Caroline Wildbourne, Jane-Louise Sinclair and Dr Penelope De Lacavalerie for their assistance with recruitment at their respective sites and Maryann Kurien for her research assistance. We also thank Nicholas Marsden and Emma Jane Li Sian Boles for delivering the intervention. Jane Young was supported by a Cancer Institute NSW Academic Leader in Cancer Epidemiology grant. This study was funded by National Health and Medical Research (NHMRC) Project Grant 632645.
Conflict of interest
None to declare
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shaw, J.M., Young, J.M., Butow, P.N. et al. Improving psychosocial outcomes for caregivers of people with poor prognosis gastrointestinal cancers: a randomized controlled trial (Family Connect). Support Care Cancer 24, 585–595 (2016). https://doi.org/10.1007/s00520-015-2817-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-015-2817-3