Abstract
Background
Aprepitant, a neurokinin-1 receptor antagonist, in combination with 5 HT-3 antagonist and dexamethasone is recommended in adults receiving moderately and highly emetogenic chemotherapy to reduce chemotherapy-induced vomiting (CIV). Data for use of aprepitant in children is limited and hence aprepitant is not recommended by Pediatric Oncology Group of Ontario guidelines for prevention of CIV in children <12 years.
Methods
A randomized, double-blind, placebo-controlled trial was conducted at a single center in chemotherapy naïve children (5–18 years) receiving highly emetogenic chemotherapy. All patients received intravenous ondansetron (0.15 mg/kg) and dexamethasone (0.15 mg/kg) prior to chemotherapy followed by oral ondansetron and dexamethasone. Patients randomly assigned to aprepitant arm received oral aprepitant (15–40 kg = days 1–3, 80 mg; 41–65 kg = day 1, 125 mg and days 2–3, 80 mg) 1 h before chemotherapy. Control group received placebo as add-on therapy. Primary outcome measure was the incidence of acute moderate to severe vomiting, which was defined as more than two vomiting episodes within 24 h after the administration of the first chemotherapy dose until 24 h after the last chemotherapy dose in the block. Complete response (CR) was defined as absence of vomiting and retching during the specified phase.
Results
Of the 96 randomized patients, three were excluded from analysis; 93 patients were analyzed (50 in aprepitant arm and 43 in placebo arm). Acute moderate and severe vomiting was reported in 72 % patients receiving placebo and 38 % patients receiving aprepitant (p = 0.001). Complete response rates during acute phase were significantly higher in aprepitant arm (48 vs. 12 %, p < 0.001). No major adverse effects were reported by patients/guardians.
Conclusions
This double-blind, randomized, placebo-controlled trial shows that aprepitant significantly decreases the incidence of CIV during acute phase when used as an add-on drug with ondansetron and dexamethasone in children receiving highly emetogenic chemotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chemotherapy-induced vomiting (CIV) remains one of the most distressing toxicities of cancer treatment in pediatric patients. The incidence and severity of CIV depends on many factors, including variability among patients and the type of chemotherapeutic drugs, the dose, schedule, and route of administration used in different chemotherapy regimens [1–3]. CIV can affect the quality of life by reducing the ability to enjoy food and maintain other activities of daily living [4, 5]. Moreover, CIV can lead to poor compliance with further chemotherapy [6]. CIV control in the first chemotherapy cycle is of particular importance, as this is related to the occurrence and severity of CIV in the subsequent cycles [1, 5, 7]. In addition, patients who develop CIV in the acute phase (within 24 h of chemotherapy) are more likely to develop CIV in the delayed phase (more than 24 h after completion of chemotherapy) [8]. Current guidelines by the National Comprehensive Cancer Network, the European Society of Medical Oncology, and the American Society of Clinical Oncology recommend anti-emetic regimen consisting of a type 3 serotonin 5-hydroxytryptamine (5-HT3) receptor antagonist, a corticosteroid, and the selective substance P neurokinin-1 (NK-1) receptor antagonist, aprepitant, in adult patients receiving highly emetogenic chemotherapy [9–11].
The role of aprepitant in reducing CIV in children has not been systematically evaluated. Aprepitant in patients more than 11 years of age has been studied in a randomized controlled trial of 46 patients [12] who showed statistically insignificant increased complete response rates (CR) with aprepitant; it had the same adverse event profile as in adults and increased CR rate in delayed phase. Data in younger patients is further scarce. A single-arm prospective study of 11 patients (12 months to 17 years old) and 20 highly emetogenic chemotherapy cycles showed that aprepitant is well tolerated with 39 % CR rate [13]. No high quality evidence exists to unequivocally support the use of aprepitant in this age group. Hence, aprepitant has been incorporated in the Pediatric Oncology Group of Ontario (POGO) antiemetic guidelines only in children more than 12 years of age and receiving highly emetic chemotherapy, although this is based on a very low quality evidence [14]. In children less than 12 years of age, use of aprepitant is not recommended due to lack of evidence.
This study was designed to assess the efficacy of aprepitant as an add-on agent to anti-emetic backbone (ondansetron and dexamethasone) in reducing the incidence of CIV in pediatric patients (≤18 years of age) receiving highly emetogenic chemotherapy.
Patients and methods
Study design and patients
This was a single-center, randomized, double-blind, placebo-controlled study aimed to evaluate the efficacy of aprepitant in reducing the incidence of CIV in pediatric patients receiving highly emetogenic chemotherapy. The study was conducted in the pediatric oncology division of the cancer center at All India Institute of Medical Sciences, a tertiary care center in New Delhi which is the primary referral center for cancer patients in the northern part of India.
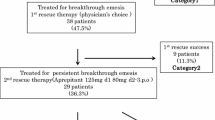
All chemotherapy naïve patients of age 5–18 years and weight 15–65 kg with confirmed diagnosis of malignancy and planned for highly emetogenic chemotherapy (as defined in POGO guidelines for classification of chemotherapeutic drugs [15]) were eligible to participate in this study. The lower limit of age and weight were arbitrary and were set to include the patients who could swallow the capsule. Consecutive patients registered during the enrollment duration were offered to participate in this study (Fig. 1). Exclusion criteria included significant organ dysfunction (aspartate aminotransferase/alanine aminotransferase >2.5 times of upper normal limit, serum bilirubin >1.5 times of upper normal limit, serum creatinine >1.5 times of upper normal limit), active infection, uncontrolled medical condition other than malignancy, pregnancy, need for contraindicated concomitant medication (terfenadine, astemizole, or cisapride), patient on systemic steroids other than use as anti-emetic agent, treatment with another investigational drug within 4 weeks of study start or prior aprepitant use, received or planned for radiotherapy to abdomen or pelvis in the week prior to treatment initiation, and vomiting within 24 h prior to treatment.
Patients who met the eligibility criteria were assigned to one of the two groups using random allocation number generated by computer. One investigator (DD) maintained randomization. The other investigators and the patients were unaware of the actual treatment allocation. Patient’s data collection forms were reviewed and collected by an independent investigator who ensured that the data was complete and accurate.
The institutional ethics committee approved the study. Written consent was obtained from guardians of all the patients. The trial was approved by the drug controller general of India (DCGI). The study was registered at clinicaltrials.gov (ClinicalTrials.gov identifier NCT01402024).
Chemotherapy protocols
Patients receiving any of the four highly emetogenic chemotherapy protocols were enrolled in this study. Of these, ABVD, VAdC, and VAC are single-day protocols. ABVD was given in standard doses (doxorubicin 25 mg/m2, bleomycin 10 mg/m2, vinblastine 6 mg/m2, and dacarbazine 375 mg/m2). VAC included vincristine 2 mg/m2, doxorubicin75 mg/m2, and cyclophosphamide 1200 mg/m2. In VAdC, vincristine 2 mg/m2, actinomycin-D 1 × 35 mg/m2, and cyclophosphamide 2200 mg/m2 were administered. Cisplatin and doxorubicin were administered over 3 days with daily dose of 40 mg/m2 cisplatin and 25 mg/m2 doxorubicin.
Antiemetic treatments
On the day of chemotherapy, all the patients received ondansetron (0.15 mg/kg; maximum 16 mg) as an intravenous bolus followed by dexamethasone (0.15 mg/kg) as 15-min intravenous infusion in 100 ml normal saline 30 min prior to chemotherapy. Patients were randomly assigned to one of the two groups; aprepitant group received aprepitant capsules (Empov; Dr Reddy’s Laboratories, India) 1 h prior to chemotherapy on days 1–3. The dose of aprepitant was based on weight groups; 15–40 kg received 80 mg on days 1–3 and 41–65 kg received 125 mg on day 1 followed by 80 mg on days 2–3. The other group received placebo capsules containing starch (prepared by Dr. Reddy’s Laboratories, India). The patients were required to swallow the whole capsule and opening of capsule was not permitted.
In addition to intravenous ondansetron and dexamethasone, as per our institutional practice, all patients received oral ondansetron (0.3 mg/kg q 8 hourly) and oral dexamethasone (0.15 mg/kg q 8 hourly) starting from the day of chemotherapy till 48 h after completion of chemotherapy. Rescue medications were permitted for vomiting (except additional aprepitant) as “add on” to ondansetron and dexamethasone therapy. The rescue agents included additional ondansetron and/or dexamethasone, or metoclopromide. The maximum total dose allowed for oral ondansetron was 32 mg per day.
To ensure the blinding of patients, the drugs (aprepitant or placebo) were put into identical capsules (one for each day, days 1–3). Patients receiving single-day chemotherapy received day 1 capsule under supervision and compliance on day 2 and day 3 was assessed by counting the remaining pills on day 3. In patients receiving 3-day chemotherapy protocol, all three doses were administered under supervision.
Definitions
Vomiting was defined as a reflexive act of ejecting the contents of the stomach through the mouth. An emetic episode was defined as a single vomiting or retching episode or any number of continuous vomiting episodes. One emetic episode had to be separated from another by the absence of vomiting or retching for at least 1 min. Acute vomiting was defined as any episode occurring after the administration of the first chemotherapy dose until 24 h after the last chemotherapy dose in the block. Delayed vomiting was considered from 24 h up to 6 days after the last dose of chemotherapy. For single-day and 3-day protocols, the acute vomiting was evaluated up to day 2 and day 4, respectively. Overall vomiting included both acute and delayed phase assessment. Complete response (CR) was defined as absence of vomiting and retching during the specified phase. Oral intake for both food and fluid was also separately recorded during this period as normal or decreased as compared to pre-chemotherapy intake, as stated by the guardian or patient.
Clinical assessment
Baseline demographic details of all patients were recorded. Details of vomiting were recorded in a diary by the guardian or patient that contained questions regarding vomiting along with some additional variables like other chemotherapy-related toxicities, food and fluid intake, and requirement of any rescue medication. This tool has previously been used in another randomized controlled trial, conducted in this institute [16].
The guardian and patient were explained in detail in their own language about the filling out of diary. The diary was handed over to the guardian to record all the events at home (incidence and severity of vomiting, other toxicities, and oral intake) till 6 days after last chemotherapy. The adverse events were recorded as reported by the patients and guardians in the diary as per the NCI CTCAEv4.0. Febrile neutropenia records were reviewed from the health records for all patients. Febrile neutropenia was defined as oral temperature >38.5 °C or two consecutive readings of >38.0 °C for 2 h and an absolute neutrophil count <0.5 × 109/l, or expected to fall below 0.5 × 109/l. The patients were monitored till the administration of next chemotherapy cycle.
Outcome measures
The primary end point of this study was acute moderate and severe vomiting. The National Cancer Institute guidelines were used to assess the severity of vomiting based on the data provided by the patient in the diary (Table 1) [17]. Vomiting was grouped as nil to mild and moderate to severe for analysis. The secondary end points included complete control of delayed vomiting, the complete CIV response rate, and normal oral intake (food and fluid). Complete CIV response was defined as absence of vomiting and retching during the respective phase. Oral intake was compared to the pre-chemotherapy intake by the patient and guardian, and recorded as normal or decreased.
Statistical analysis
The following assumptions were made for sample size calculations: the incidence of moderate to severe acute vomiting in control group would be approximately 70 %, as observed previously [14] and adding aprepitant would decrease this to 50 %. With a power of 80 % and significance level of 5 % for a two-sided test able to compare the rates of overall CIV reduction between the two independent samples, 103 patients per arm were necessary to detect a significant difference. Assuming 10 % loss to follow-up, discontinuation of drug, or non-compliance and dropouts, 110 patients in each group were required.
Descriptive statistics were used to analyze the demographic and clinical characteristics of all the patients. A modified intention-to-treat population, i.e., patients who received chemotherapy, took one or more doses of study drug, and had one or more post treatment measurements, was used for efficacy analysis. Comparison between categorical variables was done by chi-square test and continuous variables were compared by Student’s t test. Incidence of CIV and CR rates were compared between patients who received 1-day and 3-day chemotherapy protocols in those who were randomized to the aprepitant arm. All tests were two-sided, and a significance level of 0.05 was used. All statistical analysis were carried out by Stata (version 12).
Role of funding source
The funding source (Dr. Reddy’s Laboratories Ltd., Hyderabad, India) had no role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Results
From September 2011 to February 2013, 107 patients were screened for eligibility in the trial, of which 96 were enrolled in this study. Three patients did not fill out the diary and hence were excluded from the analysis. Therefore, 93 patients were evaluated: 50 in aprepitant arm and 43 in the control arm (Fig. 1). The study was closed before reaching the planned number of patients as per the protocol due to poor accrual, and the results were analyzed.
The baseline characteristics were comparable between the two arms (Table 2).
Acute and delayed moderate to severe vomiting (Table 3)
In the acute phase, there was significant reduction in the incidence of moderate and severe vomiting in the group receiving aprepitant as compared to the placebo group (38 vs. 72 %, p = 0.001). There was no significant difference between the two groups in moderate to severe vomiting in the delayed phase (42 vs. 56 %, p = 0.18). Overall, combining both acute and delayed phase, 84 % patients in the placebo arm had moderate to severe vomiting as compared to 56 % in the aprepitant arm (p = 0.004).
Complete response
CR during acute phase was seen in 48 % of patients receiving aprepitant, compared to 12 % in placebo arm (p < 0.001). The CR rates for aprepitant versus placebo arm during delayed phase and overall phase were 34 vs. 30 % (p = 0.7) and 22 vs. 9 % (p = 0.1), respectively.
One-day versus 3-day chemotherapy
Of the 50 patients in aprepitant arm, 38 patients received 1-day chemotherapy and 12 patients received 3-day chemotherapy. In aprepitant arm, the CR rates (1-day vs. 3-day chemotherapy) during acute phases were 55 vs. 25 % (p = 0.07) and 42 vs. 8 % (p = 0.03), respectively.
In the placebo arm, 26 patients received 1-day chemotherapy and 17 patients received 3-day chemotherapy. In this arm, the CR rates (1-day vs. 3-day chemotherapy) during acute phases were 19 vs. 0 % (p = 0.05) and 42 vs. 12 % (p = 0.03), respectively.
Other outcome measures (Table 4)
Five of 43 patients in the placebo arm and five of 50 patients in the aprepitant arm required rescue medications for vomiting (p = 0.8). One patient in the placebo arm required hospitalization for severe vomiting requiring intravenous fluids and antiemetics.
Oral intake was compared with pre-chemotherapy intake. Fluid intake was significantly decreased in both acute and delayed phases of assessment in the placebo arm as compared to the aprepitant arm (p = 0.03 and p = 0.002, respectively). Likewise, food intake was significantly decreased in the acute phase in the placebo arm (p = 0.04), but this difference was not seen in the delayed phase (p = 0.15).
Adverse events (Table 5)
None of the patients developed any grade 3 or 4 adverse events. Most common adverse events reported in the study were anorexia and headache (grade 1 or 2), which occurred with similar frequency in both the groups (Table 5). Other side effects observed were constipation, diarrhea, and gastritis, which occurred in similar frequency in both the arms.
The adverse events could not be assessed in patients who did not complete the diary; however, a review of their health record did not reveal any grade 3 or 4 adverse event. Specifically, the incidence of febrile neutropenia was similar in both aprepitant and placebo arms (12 vs. 18 %, p = 0.36).
Discussion
The study showed that aprepitant significantly reduced moderate to severe acute phase CIV and increased complete acute CIV response rate in the aprepitant arm. However, there was no difference between the study arms with respect to delayed CIV complete response rates. In a sub-group analysis, significantly higher delayed CIV complete response rates were noted in the aprepitant arm receiving 1-day chemotherapy compared to 3-day chemotherapy regimens.
The role of aprepitant has been clearly elucidated in several randomized controlled trials in adults receiving highly emetogenic chemotherapy [18–20]. As a result, use of aprepitant has been incorporated in most of the antiemetic guidelines for adult patients. The data for use of aprepitant is lacking in the pediatric patients. In a retrospective analysis by Choi et al. [21], use of aprepitant in children (32 months to 18 years) receiving highly or moderately emetogenic chemotherapy was not associated with significant reduction of CIV. A prospective observational study conducted by Bodge et al. showed safety and efficacy of aprepitant in children <40 kg in 11 patients [13]. The study was not randomized and the sample size was too small to conclude firmly on the use of aprepitant. A randomized, double-blind, placebo-controlled trial in 11–19-year-old patients did not reveal significant difference in CR rates; however, the delayed phase vomiting was significantly reduced with the use of aprepitant [12]. A recent retrospective review of 26 patients reported the use of aprepitant and fosaprepitant in children as young as 11 months [22]. However, the dose of aprepitant was highly variable among the patients. Two other retrospective analyses in pediatric population have been published that show improved control of CIV with the use of aprepitant [23, 24].
The results of our study clearly demonstrate the role of aprepitant in 5–18-year-old patients receiving highly emetogenic chemotherapy. The CR rates were significantly higher during the acute phase in the aprepitant arm. It is expected that this will improve the quality of life of these patients, although this was not assessed in our study. This was also supported indirectly by the significantly higher proportion of patients with normal food and fluid intake in the acute phase in the aprepitant arm. However, the CR rates for delayed and overall phases were not different in the two arms. Aprepitant is effective in both acute and delayed phases in adult population [25]. The lack of efficacy of aprepitant in delayed CIV observed in this study may be due to smaller sample size or a heterogeneous population receiving both 1-day and 3-day chemotherapy protocols. None of the patients receiving 3-day chemotherapy achieved an overall CR. Use of aprepitant beyond 3 days in patients receiving multi-day chemotherapy regimens may increase the CR rates and requires further investigation.
Further, aprepitant appears to be safe with no major reported adverse effects by the patients; notably the adverse events in our study were not prospectively monitored and relied on spontaneous reporting by the patients and guardians. An increase in the number of episodes of febrile neutropenia has been reported in earlier trials in both pediatric and adult populations [12, 13, 17]; however, this was not observed in this study.
In our study, we used similar dexamethasone dose in both the arms. In adults, it has been shown that aprepitant decreases the metabolism of dexamethasone and thereby increasing its bioavailability. However, such interaction has not been studied in pediatric population and the recommendation for dose reduction is an extrapolation of observation from adult studies. The exact reduction in dexamethasone dose is not known in pediatric population. In the retrospective analysis by Choi et al. [21], the dose of dexamethasone was same in patients receiving aprepitant and no increased adverse effects were noted. Our study had the same finding, but increased availability of dexamethasone may be a confounder in decreasing the CIV. The CR rates reported in our study (48 %) are somewhat higher than those reported in earlier studies in pediatric age group (36–39 %) [12, 13]. The increased CR rate may be due to the increased dexamethasone dose in the aprepitant arm.
We observed lower CR rates as compared to adult experience with aprepitant (63–68 %) [18, 20]. This has been observed in earlier studies as well, and the reason may be difference in chemotherapy regimen and dose intensity [12, 13]. Difference in pharmacokinetics or differential mechanisms of emesis in children may be contributory; however, this requires further investigation.
The dose of aprepitant used in this study is also different from the POGO recommendations. However, the dose of aprepitant in pediatric population is not standardized and depends on individual institutional practice. The same dose as ours has been used in other published studies as well [13, 22].
The demerit of our study was that the primary outcome measure was taken as acute moderate and severe vomiting and not CR, which has been reported in most of the studies. However, post hoc analysis of CR rates was done that showed significantly increased CR rates during the acute phase. Additionally, the adverse events were not prospectively monitored and relied on spontaneous reporting by patient or guardian. This could have led to under-reporting of adverse events. Also, the assessment of oral intake was subjective and assessed by patient and guardian as compared to the pre-chemotherapy intake.
To conclude, this double-blind, randomized, placebo-controlled trial unequivocally shows that aprepitant significantly decreases the incidence of CIV during acute phase when used as an add-on drug with ondansetron and dexamethasone in children receiving highly emetogenic chemotherapy.
Future directions
Despite the limitations of this study, it has clearly proved the role of aprepitant in decreasing CIV in pediatric patients receiving highly emetogenic chemotherapy; however, its role in children <5 years remains to be assessed. Dose-finding studies should be conducted to determine the optimal pediatric dose and frequency of aprepitant. The role of this drug was studied only in highly emetogenic protocols and may further be assessed in moderately emetogenic chemotherapy since significant reduction has been reported in adults.
References
Hesketh PJ (2008) Chemotherapy-induced nausea and vomiting. N Engl J Med 358(23):2482–2494
Gralla RJ, Osoba D, Kris MG, Kirkbride P, Hesketh PJ, Chinnery LW et al (1999) Recommendations for the use of antiemetics: evidence-based, clinical practice guidelines. American Society of Clinical Oncology. J Clin Oncol Off J Am Soc Clin Oncol 17(9):2971–2994
Bouganim N, Dranitsaris G, Hopkins S, Vandermeer L, Godbout L, Dent S et al (2012) Prospective validation of risk prediction indexes for acute and delayed chemotherapy-induced nausea and vomiting. Curr Oncol 19(6):e414–e421
Grunberg SM, Slusher B, Rugo HS (2003) Emerging treatments in chemotherapy-induced nausea and vomiting. Clin Adv Hematol Oncol 11(2 Suppl 1):1–18, quiz 2 p following 18
Cohen L, de Moor CA, Eisenberg P, Ming EE, Hu H (2007) Chemotherapy-induced nausea and vomiting: incidence and impact on patient quality of life at community oncology settings. Support Care Cancer Off J Multinatl Assoc Support Care Cancer 15(5):497–503
Richardson JL, Marks G, Levine A (1988) The influence of symptoms of disease and side effects of treatment on compliance with cancer therapy. J Clin Oncol Off J Am Soc Clin Oncol 6(11):1746–1752
Morrow GR, Roscoe JA, Hickok JT, Stern RM, Pierce HI, King DB et al (1998) Initial control of chemotherapy-induced nausea and vomiting in patient quality of life. Oncology (Williston Park) 12(3 Suppl 4):32–37
Warr DG, Grunberg SM, Gralla RJ, Hesketh PJ, Roila F, de Wit R et al (2005) The oral NK(1) antagonist aprepitant for the prevention of acute and delayed chemotherapy-induced nausea and vomiting: pooled data from 2 randomised, double-blind, placebo controlled trials. Eur J Cancer Oxf Engl 1990 41(9):1278–1285
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Antiemesis—antiemesis.pdf [Internet]. [cited 2014 Jan 1]. Available from: http://www.nccn.org/professionals/physician_gls/pdf/antiemesis.pdf
Roila F, Herrstedt J, Aapro M, Gralla RJ, Einhorn LH, Ballatori E et al (2010) Guideline update for MASCC and ESMO in the prevention of chemotherapy- and radiotherapy-induced nausea and vomiting: results of the Perugia consensus conference. Ann Oncol Off J Eur Soc Med Oncol ESMO 21(Suppl 5):v232–v243
Basch E, Prestrud AA, Hesketh PJ, Kris MG, Feyer PC, Somerfield MR et al (2011) Antiemetics: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol Off J Am Soc Clin Oncol 29(31):4189–4198
Gore L, Chawla S, Petrilli A, Hemenway M, Schissel D, Chua V et al (2009) Aprepitant in adolescent patients for prevention of chemotherapy-induced nausea and vomiting: a randomized, double-blind, placebo-controlled study of efficacy and tolerability. Pediatr Blood Cancer 52(2):242–247
Bodge M, Shillingburg A, Paul S, Biondo L (2013) Safety and efficacy of aprepitant for chemotherapy-induced nausea and vomiting in pediatric patients: a prospective, observational study. Pediatr Blood Cancer
Dupuis LL, Boodhan S, Holdsworth M, Robinson PD, Hain R, Portwine C et al (2013) Guideline for the prevention of acute nausea and vomiting due to antineoplastic medication in pediatric cancer patients. Pediatr Blood Cancer 60(7):1073–1082
Dupuis LL, Boodhan S, Sung L, Portwine C, Hain R, McCarthy P et al (2011) Guideline for the classification of the acute emetogenic potential of antineoplastic medication in pediatric cancer patients. Pediatr Blood Cancer 57(2):191–198
Pillai AK, Sharma KK, Gupta YK, Bakhshi S (2011) Anti-emetic effect of ginger powder versus placebo as an add-on therapy in children and young adults receiving high emetogenic chemotherapy. Pediatr Blood Cancer 56(2):234–238
Nausea and Vomiting (PDQ®)—National Cancer Institute [Internet]. [cited 2014 Jan 1]. Available from: http://www.cancer.gov/cancertopics/pdq/supportivecare/nausea/HealthProfessional/page1/AllPages
Poli-Bigelli S, Rodrigues-Pereira J, Carides AD, Julie Ma G, Eldridge K, Hipple A et al (2003) Addition of the neurokinin 1 receptor antagonist aprepitant to standard antiemetic therapy improves control of chemotherapy-induced nausea and vomiting. Results from a randomized, double-blind, placebo-controlled trial in Latin America. Cancer 97(12):3090–3098
Hesketh PJ, Grunberg SM, Gralla RJ, Warr DG, Roila F, de Wit R et al (2003) The oral neurokinin-1 antagonist aprepitant for the prevention of chemotherapy-induced nausea and vomiting: a multinational, randomized, double-blind, placebo-controlled trial in patients receiving high-dose cisplatin—the Aprepitant Protocol 052 Study Group. J Clin Oncol Off J Am Soc Clin Oncol 21(22):4112–4119
Gralla RJ, de Wit R, Herrstedt J, Carides AD, Ianus J, Guoguang-Ma J et al (2005) Antiemetic efficacy of the neurokinin-1 antagonist, aprepitant, plus a 5HT3 antagonist and a corticosteroid in patients receiving anthracyclines or cyclophosphamide in addition to high-dose cisplatin: analysis of combined data from two phase III randomized clinical trials. Cancer 104(4):864–868
Choi MR, Jiles C, Seibel NL (2010) Aprepitant use in children, adolescents, and young adults for the control of chemotherapy-induced nausea and vomiting (CINV). J Pediatr Hematol Oncol 32(7):e268–e271
Shillingburg A, Biondo L (2014) Aprepitant and fosaprepitant use in children and adolescents at an academic medical center. J Pediatr Pharmacol Ther JPPT Off J PPAG 19(2):127–131
Duggin K, Tickle K, Norman G, Yang J, Wang C, Cross SJ et al (2014) Aprepitant reduces chemotherapy-induced vomiting in children and young adults with brain tumors. J Pediatr Oncol Nurs Off J Assoc Pediatr Oncol Nurses 31(5):277–283
Bauters TGM, Verlooy J, Robays H, Benoit Y, Laureys G (2013) Emesis control by aprepitant in children and adolescents with chemotherapy. Int J Clin Pharm 35(6):1021–1024
dos Santos LV, Souza FH, Brunetto AT, Sasse AD, da Silveira Nogueira Lima JP (2012) Neurokinin-1 receptor antagonists for chemotherapy-induced nausea and vomiting: a systematic review. J Natl Cancer Inst 104(17):1280–1292
Funding
Drug and placebo were supplied by Dr. Reddy’s Laboratories Ltd., Hyderabad, India. However, they were not involved in study design or analysis.
The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Contribution
Sameer Bakhshi: Literature search, figures, study design, data collection, data analysis, data interpretation, writing.
Atul Batra: Literature search, figures, data analysis, data interpretation, writing.
Bivas Biswas: Literature search and study design.
Deepa Dhawan: Blinding, randomization, figures, data collection, data analysis, data interpretation, writing.
Reeja Paul: Data collection and writing.
Vishnubhatla Sreenivas: Literature search, figures, study design, data analysis, data interpretation, writing.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Additional information
ClinicalTrials.gov Identifier: NCT01402024
Rights and permissions
About this article
Cite this article
Bakhshi, S., Batra, A., Biswas, B. et al. Aprepitant as an add-on therapy in children receiving highly emetogenic chemotherapy: a randomized, double-blind, placebo-controlled trial. Support Care Cancer 23, 3229–3237 (2015). https://doi.org/10.1007/s00520-015-2714-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-015-2714-9