Abstract
Purpose
The aim of this study is to compare the generic and ostomy-specific quality of life (QoL) between cancer and non-cancer ostomy patients using a mixed-method design.
Methods
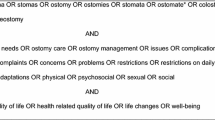
All patients with an ostomy participating in the Stomapanel of the Dutch Ostomy Association were asked to complete a generic (RAND-36) and ostomy-specific (Stoma-QoL) QoL questionnaire. In addition, open-ended questions on symptoms, restrictions or adaptations influencing daily life were included. The generic and ostomy-specific QoL between cancer and non-cancer ostomy patients were compared using linear regression analyses. Qualitative responses were analysed using content analysis.
Results
In total, 668 patients were included: 379 cancer patients (80 % colorectal, 17 % bladder and 3 % other) and 289 non-cancer patients (38 % colitis ulcerosa, 22 % Crohn’s disease and 40 % other) with a colostomy (55 %), ileostomy (31 %) and/or urostomy (16 %). Adjusted for gender, age, type of ostomy and time elapsed since ostomy surgery, cancer ostomy patients scored higher (better) on Stoma-QoL (β = 2.1) and all RAND-36 domains (9.1 < β ≤ 19.5) except on mental health compared to non-cancer ostomy patients. Of the 33 themes coded for in the content analysis, fatigue or sleeplessness, leakages, pain, bladder or bowel complaints, physical functioning or activity, travelling or being away from home, other daily activities (including work), clothing and diet were among the 10 most frequently reported themes, although ranking differed between both patient groups. Besides, cancer ostomy patients frequently reported on the impact on (engaging in a) relationship or sexual intimacy and non-cancer ostomy patients frequently reported to be relieved of symptoms and restrictions in daily life.
Conclusions
Cancer patients reported better generic and ostomy-specific QoL than non-cancer ostomy patients. In both cancer and non-cancer ostomy patients, fatigue or sleeplessness, leakages, pain, bladder or bowel complaints, physical functioning or activity, travelling or being away from home, other daily activities (including work), clothing and diet were among the 10 most common reported themes influencing daily life. However, the ranking of these 10 most common themes was different in both patient groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An ostomy is a surgically created opening between the colon, ileum or bladder and the abdominal wall by which stool, urine or mucus is discharged [1] and may be created when (part of) the colon, ileum, rectum or bladder has to be removed, in case of faecal or urine incontinence, or when it has to recover from an operation or inflammation. Different disorders and diseases may be the cause of ostomy creation, such as colorectal or bladder cancer, inflammatory bowel diseases like colitis ulcerosa or Crohn’s disease and diverticulitis.
Ostomy patients often suffer from symptoms including leakages, skin irritation, parastomal hernia, fluid and electrolyte imbalance, intestinal obstruction or stoma prolapse [2], which may impair their quality of life (QoL) [3]. In addition, ostomy-related challenges in daily life such as clothing restrictions, travelling restrictions, issues regarding sexuality and intimacy and self-care may negatively influence QoL of ostomy patients [4, 5] even a long time after ostomy creation [5].
Since ostomy patients are a heterogeneous group with regard to indications and types of ostomies, there may be substantial differences in QoL among patient groups. A lower QoL was reported in women with an ostomy compared to men [6] and in older ostomy patients [7]. In addition, colostomy patients have experienced less severe skin problems than ileostomy patients [3, 8], while the effluent of colostomy patients was less tolerable and their appetite more often affected compared to ileostomy patients [9]. Colostomy patients were also reported to have a lower disease-specific QoL scale than patients with an ileostomy [10], while no difference in ostomy-specific or generic QoL has been reported [10–12].
Less is known on differences in QoL between ostomy patients with different indications for ostomy creation. Information on potential differences in QoL between ostomy patients with different indications may provide insight into groups of ostomy patients in need for additional supportive care and into opportunities for clinical care enhancement. While Canova et al. [11] found no differences, Krouse et al. [13] found that cancer patients with a colostomy had a better ostomy-specific QoL than patients with a colostomy due to other causes than cancer. Krouse et al. (2007) hypothesized that the difference in QoL may be due to a better overall health in cancer ostomy patients, since most cancer ostomy patients were likely to be cured from their cancer at the time of QoL assessment, while non-cancer ostomy patients may still experience disease-specific symptoms. Ostomy patients with colorectal cancer also reported less severe skin problems than ostomy patients with inflammatory bowel diseases [3]. Severe leakages were less frequently reported in ostomy patients with colorectal cancer or inflammatory bowel diseases compared to ostomy patients with other indications (i.e. diverticulitis, trauma, familial polyposis, inflammatory processes and cancers other than colorectal cancer).
Although some studies have reported differences in QoL between cancer and non-cancer ostomy patients [3, 13], a direct comparison of the generic QoL between cancer and non-cancer ostomy patients including patients with a colostomy, ileostomy and urostomy is lacking. Therefore, the aim of this study was to compare the generic and ostomy-specific QoL of cancer patients with the QoL of non-cancer patients with a colostomy, ileostomy or urostomy. For this study, a mixed-method design was used, since the combination of qualitative and quantitative findings was expected to provide a more complete understanding on this subject [14]. The quantitative findings provided information on the absolute difference in QoL between cancer and non-cancer ostomy patients, while the qualitative data provided information on the relative importance of several symptoms, restrictions and adaptations influencing daily life in cancer and non-cancer ostomy patients.
Methods
Design and study participants
This mixed-method cross-sectional cohort study used data of the online Stomapanel of the Dutch Ostomy Association. In August 2012, all 1442 ostomy patients participating in the Stomapanel were asked to fill in a questionnaire on their QoL of which 721 (50 %) responded. Ostomy patients (n = 668) were included in this study when they were 18 years or older and had a colostomy, ileostomy (continence or incontinence) or urostomy (continence or incontinence) completed both the entry questionnaire of the Stomapanel and QoL questionnaire and reported their indication for ostomy creation.
Measures
All ostomy patients were asked to complete both a generic and ostomy-specific QoL questionnaire. The generic QoL was measured with the RAND 36-item Health Survey and consisted of 35 questions on eight different dimensions of QoL: general health perception (5 items), physical functioning (10 items), social functioning (2 items), role limitations due to a physical problem (4 items), role limitations due to an emotional problem (3 items), mental health (5 items), vitality (4 items) and pain (2 items) and one additional question on health change [15]. Total scores per construct were converted to a standardized 0–100 score ((raw score − minimum score)/(maximum score − minimum score) × 100 %), in which a higher score indicated a better QoL. The RAND-36 has been reported to be a reliable and valid measurement instrument in Dutch general study populations [15, 16]. The ostomy-specific QoL was measured using the Stoma-QoL questionnaire of Prieto et al. [17]. Ostomy patients were asked to report their level of agreement with 20 different propositions, such as “I feel the need to know where the nearest toilet is” on a 4-point Likert scale, namely 1—always, 2—sometimes, 3—rarely and 4—not at all. A total score can be calculated by summing all item scores and converting it to a 0–100 score based on Rasch modeling [17], in which a higher score indicated a better QoL. The questionnaire has been reported to be a valid and reliable measurement instrument in ostomy patients [12, 17].
In addition, ostomy patients were asked to answer two open-ended questions. First, ostomy patients were asked to describe: a) symptoms, other than having an ostomy, related to the disease or treatment of the disease underlying ostomy surgery, b) the cause of these symptoms and c) the influence of these symptoms on QoL. Second, ostomy patients were asked to a) describe the influence of the ostomy on daily life and b) to give an example. The first question was answered by 37 % and the second question by 88 % of the study population. Socio-demographic (gender, year of birth, education level, employment status) and clinical (type of ostomy, indication for ostomy creation and time since ostomy surgery) characteristics of the ostomy patients were self-reported using a study-specific questionnaire.
Data analyses
Quantitative analyses were performed using the IBM Statistical Package for the Social Science (SPSS) version 20 (IBM Corp., Armonk, NY USA). Descriptive statistics (e.g. frequencies and percentages) were used to describe the socio-demographic and clinical characteristics of participants. Chi-squared tests were used to compare socio-demographic and clinical characteristics between cancer and non-cancer ostomy patients. Linear regression analyses were used to compare the generic and ostomy-specific QoL between cancer and non-cancer ostomy patients adjusted for other characteristics that differed statistically between the two groups. Analyses were considered statistically significant when p < 0.05 (two-sided). An absolute difference in QoL ≥10 % (minimal important difference) of the instrument range was considered clinically meaningful [18].
The qualitative data of the open-ended questions were analysed using content analysis [19]. Since the answers to the questions overlapped, the content of both questions were combined in the analyses. A coding scheme was developed consisting of 33 themes. Themes were formulated based on the 37-item Stoma-QoL questionnaire of Prieto et al. [17], and the coding system on ostomy-specific concerns developed by Sun et al. [5]. Some themes were added, since first exploration of a sub-sample of the data revealed that the qualitative data contained information on additional themes. The themes were categorized into four domains: symptoms and inconveniences in daily life, restrictions and adaptations in daily life, influences on social life and positive influences on daily life (Table 1).
One coder coded all qualitative data and a sub-sample of the data was coded by a second independent coder. Each answer to the open-ended questions could receive one or multiple codes based on the content of the answers; however, individual statements were not double coded. The two coders were trained using a sub-sample of the answers from both the cancer and non-cancer ostomy patients under study. Inter-rater reliability, assessed by comparing assigned codes on 10 % of the data using Cohen’s kappa, was good (mean Cohen’s kappa = 0.80) [19].
Results
Study population
In total, 379 cancer ostomy patients and 289 non-cancer ostomy patients were included in the study (Table 2). Compared to non-cancer ostomy patients, cancer ostomy patients were more often male (66 vs. 38 %), 65 years or older (57 vs. 29 %) and within 6 years since ostomy surgery (63 vs. 45 %). In addition, cancer ostomy patients most often had a colostomy (74 %), while non-cancer ostomy patients most often had an ileostomy (63 %).
Quantitative study results: generic and ostomy-specific quality of life
The generic QoL of cancer ostomy patients ranged from 65.0 (SD = 20.7) on the general health perception domain to 82.7 (SD = 22.4) on the pain domain (Table 3). The generic QoL of non-cancer ostomy patients ranged from 52.7 (SD = 44.0) on the domain on role limitations due to a physical problem to 75.8 (SD = 17.0) on the mental health domain. Adjusted for gender, age, type of ostomy and time elapsed since ostomy surgery, cancer ostomy patients had a better generic QoL score on all domains than non-cancer ostomy patients (mean adjusted difference ranged from 9.1 to 19.5) except for mental health. The mean difference of the generic QoL domains regarding general health perception, physical functioning, social functioning, role limitations due to a physical problem, role limitation due to an emotional problem and pain exceeded the minimal important difference.
Mean ostomy-specific QoL score was 61.7 (SD = 10.0) in cancer ostomy patients and 59.7 (SD = 9.6) in non-cancer ostomy patients (Table 3). Adjusted for gender, age, type of ostomy and time elapsed since ostomy surgery, cancer ostomy patients had a better ostomy-specific QoL score than non-cancer ostomy patients (mean adjusted difference was 2.1).
Qualitative study results: symptoms and restrictions or adaptations influencing daily life
In total, 287 cancer and 218 non-cancer ostomy patients provided an answer which we used in the content analysis (Table 1). Of the 33 themes coded for in the content analysis, the 10 most common reported symptoms, restrictions or adaptations influencing daily life were largely comparable between cancer and non-cancer ostomy patients (Table 4). In total, nine themes (fatigue or sleeplessness, leakages, pain, bladder or bowel complaints, physical functioning or activity, travelling or being away from home, other daily activities (including work), clothing and diet) were among the 10 most common reported themes in both groups. However, the ranking (based on the frequency of patients reporting on a symptom, restriction or adaptation in daily life) was divergent between the two groups.
In the group of cancer ostomy patients, the themes “physical functioning or activity”, “travelling or being away from home” and “other daily activities (including work)” all belonging to the domain on restrictions or adaptation in daily life were most commonly mentioned. Several cancer ostomy patients reported that their restrictions or adaptations in daily life were related to the rectum resection, which hampers the ability to sit or cycle.
My rectum did not heal properly due to the radiation treatment. This means it is not always easy to find a good sitting position—especially away from home.
The removal of my rectum has lead to major implications. For instance, cycling long distances is difficult despite having bought a luxury saddle and proper cycling trousers and pants.
Participants from the group of non-cancer ostomy patients most often mentioned the themes “fatigue or sleeplessness” and “leakages” of the domain on symptoms and inconveniences in daily life and the theme “physical functioning or activity” of the domain on restrictions or adaptations in daily life. Problems on sleeplessness and leakages were often reported in relation to their ostomy.
I sleep badly at night because I have to empty my ileostomy bag three or four times a night; and make sure there is no leakage.
While problems related to fatigue and pain were often mentioned to be associated with the indication underlying ostomy surgery.
My Colitis ulcerosa makes me tired. Prednisone does not help.
Colitis ulcerosa as well as other medications, has given me a lot of joint pain.
The fourth most frequent theme mentioned by cancer patients was the “impact on (engaging in a) relationship or sexual intimacy” of the domain on influences on social life, followed by “leakages”, “fatigue or sleeplessness”, “bladder or bowel complaints”, “pain”, “clothing” and “diet”. The impact on (engaging in a) relationship or sexual intimacy was often reported to be related to problems such as erectile dysfunction.
The operation and radiation treatment has caused me erectile problems. I feel “less of a man” and the relationship with my wife has changed.
In non-cancer ostomy patients, this theme was not among the 10 most common reported themes. Non-cancer ostomy patients next most frequently reported on “relieved of symptoms”, “pain”, “travelling or being away from home”, “bladder or bowel complaints”, “clothing”, “other daily activities (including work)”, “diet” and “relieved of restrictions in daily life”. Non-cancer ostomy patients often reported to be relieved of symptoms such as diarrhoea or to be able to go out again due to their ostomy.
I have never seen my ostomy operation as a problem, more as a relief.
Since my ostomy, I can do everything. Having stayed at home for 2 years, I now work a full week. I go for “days out” and do everything I want. With hindsight, I wish I had had the operation earlier.
Themes regarding positive influences on daily life were not among the 10 most common reported themes in the group of cancer ostomy patients.
Discussion
This mixed-method study compared the generic and ostomy-specific QoL of cancer and non-cancer ostomy patients. The quantitative part of this study showed that (adjusted for gender, age, type of ostomy and time elapsed since ostomy surgery) cancer ostomy patients reported a better generic QoL than non-cancer ostomy patients, except for the mental health domain. The mean differences on the generic QoL domains regarding general health perception, physical functioning, social functioning, role limitations due to a physical problem, role limitation due to an emotional problem and pain were clinically meaningful. On the ostomy-specific QoL scale, cancer ostomy patients scored better than non-cancer ostomy patients, although mean difference was small. Our findings were in contrast with Canova et al. [11] who did not found a difference in ostomy-specific QoL between patients with an ostomy due to colorectal cancer, inflammatory bowel diseases, complications or other causes. Krouse et al. [13] did, however, also find that cancer patients with a colostomy had a better ostomy-specific QoL than non-cancer patients with a colostomy.
In contrast to previous literature, we found no difference between cancer and non-cancer patients on the mental health domain. Krouse et al. [13] did find that non-cancer ostomy patients were more frequently anxious or depressed, and Filipovic et al. [20] reported that patients with a first episode of inflammatory bowel disease experience higher levels of depression and anxiety than patients with newly diagnosed colon cancer. In patients with an ostomy due to Crohn’s disease, high levels of anxiety and depression (42–49 %) were also reported [21].
The qualitative data revealed that, although cancer ostomy patients report a better QoL than non-cancer ostomy patients, the type of symptoms, restrictions, and adaptations influencing daily life encountered by both groups are more or less the same. In both cancer and non-cancer ostomy patients, fatigue or sleeplessness, leakages, pain, bladder or bowel complaints, physical functioning or activity, travelling or being away from home, other daily activities (including work), clothing and diet were among the 10 most common reported themes influencing daily life. However, the ranking of these 10 most common themes was different in both patient groups. Furthermore, in cancer ostomy patients the impact on (engaging in a) relationship or sexual intimacy was frequently reported, while in non-cancer ostomy patients being relieved of symptoms and restrictions in daily life was frequently reported.
Fatigue or sleeplessness, leakages and pain were ranked higher in the non-cancer ostomy patient group of this study than in the cancer ostomy patient group. As suggested by Krouse et al. [13], the high ranking of problems related to fatigue and pain in non-cancer ostomy patients may be due to ongoing medical problems related to their disease.
Cancer ostomy patients most frequently reported on restrictions and adaptation regarding physical functioning or activity, travelling or being away from home and other daily activities (including work) in this study. These high ranking of restrictions in daily life may be due to poor wound healing in patients treated with radiotherapy at the site of surgery [21] hampering for example the ability to cycle in patients who have undergone a rectum resection.
In addition, in cancer ostomy patients, an impact on (engaging in a) relationship or sexual intimacy was frequently reported, while this theme was not among the 10 most common reported themes in the non-cancer ostomy patient group. Sexual dysfunction among cancer ostomy patients, such as erectile dysfunction or decreased lubrication, related to adjuvant cancer therapy [20] may account for the high ranking of this theme among cancer ostomy patients.
Finally, non-cancer ostomy patients frequently reported on positive influences of their ostomy, such as being relieved of symptoms or restrictions in daily life. Non-cancer ostomy patients often suffer a long time from their disease before ostomy creation [22] and may experience an increase in QoL after surgery [23, 24]. In contrast to our expectations, in cancer patients, positive influences, such as post-traumatic growth or the recognition that they are still a live due to the ostomy, were not reported among the 10 most frequently reported themes. This is not in line with a previous study in which post-traumatic growth was highly prevalent among colorectal cancer survivors [25].
This study provided us with several opportunities to enhance clinical care, that are expected to be beneficial to both groups, since reported symptoms, restrictions and adaptations in daily life were largely comparable. Patient education has been found to improve self-management [26] and QoL of ostomy patients [27]. However, since several of the ostomy patients included in this study reported restrictions or adaptations regarding travelling or being away from home, providing an education program by means of eHealth may be promising, since it is easily accessible from home and has 24-h accessibility [28]. In addition, such an intervention may provide information on sexual issues encountered by ostomy patients, since especially in cancer ostomy patients, challenges related to (engaging in a) relationship or sexual intimacy were frequently reported. Lo et al. found that a multimedia intervention including information on ostomy creation and ostomy care improves self-care of ostomy patients [29]. Future research can provide more insight into the attitude towards and need for such eHealth interventions by ostomy patients.
Strengths and limitations
We consider the combination of quantitative and qualitative data a strength of this study, since the combination provided us with a more comprehensive overview on the QoL of cancer and non-cancer ostomy patients. A limitation of the present study was the recruitment of patients via an online panel, hampering generalizability to all ostomy patients, since the included patients are likely to be younger and higher educated. In addition, data on disease-specific clinical characteristics (e.g. tumour stage) were not available; therefore, we could not adjust for these characteristics. Finally, although the sample size was large enough to control for variables which were found to differ between the cancer and non-cancer patient group (e.g. type of ostomy), the study was not powered to stratify analyses for type of ostomy. Type of ostomy may potentially influence the difference in QoL between cancer and non-cancer ostomy patients. Future studies should therefore focus on a direct comparison of QoL between cancer and non-cancer patients with a specific type of ostomy.
Conclusion
Cancer ostomy patients reported a better generic and ostomy-specific QoL than non-cancer ostomy patients. Both cancer and non-cancer ostomy patients frequently reported that fatigue or sleeplessness, leakages, pain, bladder or bowel complaints, physical functioning or activity, travelling or being away from home, other daily activities (including work), clothing and diet influenced their daily life. In addition, cancer ostomy patients frequently reported on the impact on relationship or sexual intimacy, while non-cancer ostomy patients frequently reported to be relieved of symptoms and restrictions in daily life.
References
Sands LR, Marchetti F. (2011) Intestinal stomas the ASCRS textbook of colon and rectal surgery. second edition ed. 517–533
Shabbir J, Britton DC (2010) Stoma complications: a literature overview. Color Dis 12:958–964
Pittman J, Rawl SM, Schmidt CM et al (2008) Demographic and clinical factors related to ostomy complications and quality of life in veterans with an ostomy. J Wound Ostomy Continence Nurs 35(5):493–503
Krouse ES, Grant M, Wendel CS et al (2007) A mixed-methods evaluation of health-related quality of life for male veterans with and without intestinal stomas. Dis Colon Rectum 2054–2066:50(12)
Sun V, Grant M, McMullen CK et al (2013) Surviving colorectal cancer long-term, persistent ostomy-specific concerns and adaptations. J Wound Ostomy Continence Nurs 40(1):61–72
Krouse RS, Herrinton LJ, Grant M et al (2009) Health-related quality of life among long-term rectal cancer survivors with an ostomy: manifestations by sex. J Clin Oncol 27:4664–4670
Orsini RG, Thong MSY, van de Poll-Franse LV et al (2013) Quality of life of older rectal cancer patients is not impaired by a permanent stoma. EJSO 39:164–170
Baxter NN, Novotny PJ, Jacobson T, Maidl LJ, Sloan J, Young-Fadok TM (2006) A stoma quality of life scale. Dis Colon Rectum 49:205–212
Anthony Silva M, Ratnayake G, Deen KI (2003) Quality of life of stoma patients: temporary ileostomy versus colostomy. World J Surgery 27:421–424
Colquhoun P, Kaiser R, Weiss EG et al (2006) Correlating the fecal incontinence quality-of-life score and the SF-36 to a proposed ostomy function index in patients with a stoma. Ostomy Wound Manag 52(12):68–74
Canova C, Giorato E, Roveron G, Turrini P, Zanotti R (2013) Validation of a stoma specific quality of life questionnaire in a sample of patients with colostomy or ileostomy. Color Dis 15:e692–e698
Dol L, van Keizerswaard P, Smits S. (2008) Validation of a Dutch version of Stoma-QoL
Krouse R, Grant M, Ferell B, Dean G, Nelson R, Chu D (2007) Quality of life outcomes in 599 cancer and non-cancer patients with colostomies. J Surg Res 138:79–87
van Griensven H, Moore AP, Hall V. (2014) Mixed methods research - The best of both worlds? Manual Therapy
VanderZee KI, Sanderman R, Heyink J (1996) A comparison of two multidimensional measures of health status: the Nottingham health profile and the RAND 36-item health survey 1.0. Qual Life Res 5:165–174
VanderZee KI, Sanderman R, Heyink JW, de Haes H (1996) Psychometric qualities of the RAND 36-item health survey 1.0: a multidimensional measure of general health status. Int J Behav Med 3(2):104–122
Prieto L, Thorsen H, Juul K. (2005) Development and validation of a quality of life questionnaire for patients with colostomy ot ileostomy. Health Quality Life Outcomes 3(62)
Ringash J, O’Sullivan B, Bezjak A, Redelmeier DA (2007) Interpreting clinically significant changes in patient-reported outcomes. Cancer 110(1):196–202
Downe-Wamboldt B (1992) Content analysis: method, applications and issues. Health Care Women Int 13:313–321
Breukink SO, Donovan KA (2013) Physical and psychological effects of treatment on sexual functioning in colorectal cancer survivors. J Sex Med 10(suppl 1):74–83
Dormand E, Banwell PE, Goodacre TEE (2005) Radiotherapy and wound healing. Int Wound J 2(2):112–127
Brown H, Randle J (2005) Living with a stoma: a review of the literature. J Clin Nurs 14:74–81
Umanskiy K, Fichera A (2010) Health related quality of life in inflammatory bowel disease: the impact of surgical therapy. World J Gastroenterol 16(40):5024–5034
Knowles SR, Wilson J, Wilkinson A et al (2013) Psychological well-being and quality of life in Crohn’s disease patients with an ostomy a preliminary investigation. J Wound Ostomy Continence Nurs 40(6):623–629
Jansen L, Hoffmeister M, Chang-Claude J, Brenner H, Arndt V (2011) Benefit finding and post-traumatic growth in long-term colorectal cancer survivors: prevalence, determinants, and associations with quality of life. Br J Cancer 105:1158–1165
Cheng F, Xu Q, Dai XD, Yang LL (2012) Evaluation of the expert patient program in a Chinese population with permanent colostomy. Cancer Nurs 2012(35):27–33
Danielsen AK, Burchart J, Rosenberg J. (2013) Patient education has a positive effect in patients with a stoma: a systematic review. Colorectal Dis 15(e276-e283)
Leykin Y, Thekdi SM, Shumay DM, Munoz RF, Riba M, Dunn LB (2012) Internet interventions for improving psychological well-being in psycho-oncology: review and recommendations. Psychooncology 21:1016–1025
Lo SF, Wang Y, Wu L, Hsu M, Chang S, Hayter M (2010) Multimedia education programme for patients with a stoma: effectiveness evaluation. J Adv Nurs 67(1):68–76
Conflict of interest
This study was financially supported by the Dutch Ostomy Association. The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jansen, F., van Uden-Kraan, C.F., Braakman, J.A. et al. A mixed-method study on the generic and ostomy-specific quality of life of cancer and non-cancer ostomy patients. Support Care Cancer 23, 1689–1697 (2015). https://doi.org/10.1007/s00520-014-2528-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-014-2528-1