Abstract
Background
This is a single-center, prospective, observational study aiming to determine the effects of unidentified renal insufficiency (URI) on the safety and efficacy of chemotherapy for metastatic colorectal cancer (mCRC) patients.
Patients and methods
mCRC patients with normal serum creatinine and who were treated with CapeOx as the first-line therapy were included. Creatinine clearance (CrCL) was estimated using the Cockcroft–Gault formula. URI was characterized by a CrCL of less than 60 ml/min. Logistic regression was used to assess the effects of URI on toxicities and response rates. Kaplan–Meier curve was used to evaluate the effect of URI on survival.
Results
A total of 143 patients were enrolled, of whom 34.9 % had URI. Compared with the control group, the URI group had longer toxicity durations and developed significantly more grade 1 to 2 toxicities after adjusting for age, gender, and body mass index. The toxicities include cytopenia (76 vs. 61 %, OR = 1.86, 95 % CI = 0.39–2.53, P < 0.001), diarrhea (34 vs. 29 %, OR = 3.76, 95 % CI = 0.95–6.53, P = 0.007), stomatitis (10 vs. 6 %, OR = 2.81, 95 % CI = 1.10–4.28, P = 0.002), and hand–foot syndrome (18 vs. 11 %, OR = 2.56, 95 % CI = 0.86–5.41, P = 0.045). The response rate and time to progression were significantly lower in the URI group than in the control group (4.5 vs. 5.5 months, HR = 1.57, 95 % CI = 1.09–2.25, P = 0.015), whereas the overall survival rates of the two groups were similar.
Conclusion
In conclusion, URI can increase the toxicity and decrease the TTP of CapeOx-treated mCRC patients. Renal function screening via CrCL estimation is required for all mCRC patients before initial chemotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Renal insufficiency (RI), which is defined as glomerular filtration rate (GFR) <90 ml/min, is common in cancer patients. Several studies have shown that approximately 50 to 60 % of cancer patients have a glomerular filtration rate of <90 ml/min per 1.73 m2, which can be attributed to immunoreaction or tumor invasion [1, 2]. Although serum creatinine (SCr) is commonly used to screen for renal function, its sensitivity is insufficient for cancer patients because it is affected by several factors, such as state of nutrition, tumor consumption, and performance status. Several studies have reported that a substantial number of cancer patients with normal SCr have significantly reduced creatinine clearance (CrCL) [3–5] and thus have unidentified renal insufficiency (URI). The Cockcroft–Gault formula or the abbreviated modification of diet in renal disease (aMDRD) formula is more accurate and sensitive in detecting even mild renal function impairments [6].
A regimen of capecitabine plus oxaliplatin (CapeOx) has been recommended as one of the first-line therapy for metastatic colorectal cancer (mCRC) [7]. Capecitabine is first metabolized to 5′-deoxy-5-fluorocytidine (5′-DFCR) in the liver; 5′-DFCR is then converted to 5′-deoxy-5′-fluorouridine (5′-DFUR) in the liver and tumors. Further catalytic activation of 5′-DFUR to 5-FU then occurs in tumor tissues. Subsequently, 5-FU is further metabolized to dihydrofluorouracil and then to fluoro-beta-alanine (FBAL). Approximately 99.5 % of capecitabine and its metabolites are renally excreted. Therefore, the blood concentrations of capecitabine and its metabolites are significantly affected by renal function. Research has shown that renal insufficiency increases systemic exposure to 5′-DFCR and FBAL, leading to a 50 % reduction in creatinine clearance (CrCL) [8]. Therefore, RI probably affects the efficacy and toxicity of capecitabine. Although oxaliplatin also triggers approximately 50 % renal excretion in 48 h. for RI, only the filterable platinum removal decreases, and the toxicity does not increase [9, 10]. According to the International Society of Geriatric Oncology (SIGO), oxaliplatin dosage for cancer patients with RI needs no adjustments even in geriatric patients [11].
Despite the large percentage of mCRC patients with URI [1, 2], most oncologists still rely on SCr when assessing whether chemotherapy dosage adjustment is required, which may lead to drug-associated adverse effects. Thus, we collected medical records of mCRC patients who were treated with CapeOx and underwent normal SCr to assess the effects of URI on the safety and efficacy of chemotherapy.
Patients and methods
We conducted a single-center, prospective, observational study at The First Affiliated Hospital, College of Medicine, Zhejiang University. Patients diagnosed with mCRC were enrolled between August 2008 and January 2012. The inclusion criteria of this study are listed as follows: (1) SCr was normal before treatment. In the standardized test at our center, an SCr of 1.4 mg/dl was the upper limit of normal; (2) the CapeOx protocol was used as the first-line treatment: capecitabine 1000 mg/m2, twice per day, d1–14, every 3 weeks, until disease progression or unacceptable toxicity occurs; oxaliplatin 130 mg/m2, d1, every 3 weeks, for four cycles; and (3) the interval to the last treatment after surgery should be not more than 3 months. CrCL were calculated by using the Cockcroft–Gault formula: CrCL (ml/min) = [(140–age × weight)]/[72 × SCr] × (×0.85 if female) [12], and CrCL less than 60 ml/min (stage 2, 3, 4, or 5) was deemed as URI according to Kidney Disease Outcome Quality Initiative guidelines [13]. Data on the safety, efficacy, and dosing of CapeOx were recorded throughout the therapy and analyzed with respect to renal function. The study protocol was approved by the Ethics Committee of Zhejiang University.
Baseline characteristics, such as sex, age, height, and weight, were collected upon enrollment. Toxicities were graded per the National Cancer Institute Common Terminology Criteria for Adverse Events, version 3.0. Drug-associated adverse events, including dose delay, dose modification, or interruption, were noted throughout the therapy. The overall response rate was evaluated at the fourth cycle according to the Response Evaluation Criteria in Solid Tumors (version 1.1). Time to progression (TTP) was measured from the day CapeOx therapy was started until disease progression. TTP was censored as of the date of last tumor assessment for patients still free of progression. Overall survival (OS) was determined from the day CapeOx therapy was started until death from any cause. OS was censored as of the date of last follow-up for patients still alive or as of the last date of contact for vital status determination. Follow-up data were completed for disease progression through June 3, 2012. Survival data were updated as of May 3, 2013.
Patients were categorized according to their calculated CrCL. Baseline characteristics, toxicities, and response rates were described with summary statistics. Non-normally distributed data, such as SCr, CrCL, TTP, and OS, are presented as median. Meanwhile, normally distributed data, such as weight, are presented as mean ± SD. Univariate binary logistic regression was used to determine the effect of CrCL on adverse drug events, toxicity-associated adverse, and overall response rate (ORR). Then, adjustments were made for age, gender, and body mass index (BMI) and Karnofsky performance score (KPS) by multivariate binary logistic regression. Kaplan–Meier curves and log-rank testing were used to analyze the univariate distributions of TTP and OS, and then Cox-regression model was used to calculate the hazard ratio (HR) [14]. All P values were two sided, and P < 0.05 was considered to indicate statistical significance. Analyses were performed using SPSS version 13.0.
Results
Baseline characteristics
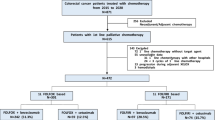
A total of 143 potential patients were enrolled in the study. The distribution of RI in mCRC patients with normal SCr is shown in Fig. 1. Forty-two (29.3 %) patients had a CrCL of more than 90 ml/min, 51 (35.7 %) had a CrCL between 60 and 90 ml/min, 42 (29.3 %) had a CrCL between 30 and 60 ml/min, and 8 (5.6 %) had a CrCL of less than 30 ml/min.
The demographic characteristics of the two groups are summarized in Table 1. In this study, 50 patients (34.9 %) with a median age of 69 years, a mean weight of 60.4 ± 10.8 kg, a median SCr of 0.96 mg/dl, and a median CrCL of 41.8 ml/min were assigned into URI group (CrCL < 60 ml/min). Meanwhile, 93 patients (65.1 %) with a median age of 56 years, a mean weight of 73 ± 15.7 kg, a median SCr of 0.81 mg/dl, and a median CrCL of 91.7 ml/min were classified into the control group (CrCL > 60 ml/min).
By the end of the follow-up, 6 patients (12.0 %) in the URI group were progression free, 8 (16.0 %) were still alive, and 2 (4.0 %) withdrew, and 18 (36.0 %) developed hypercreatininemia (median interval: 4.5 months). In the control group, 9 patients (9.6 %) were progression free, 15 (16.1 %) were still alive, and 4 (4.3 %) withdrew, and 20 (21.5 %) developed hypercreatininemia (median interval: 6 months).
Toxicities and adverse events
In general, for the URI group, the toxicity durations were longer, and the patients developed significantly more grade 1 to 2 toxicities than the control group after adjusting for gender, age, and BMI. These toxicities include cytopenia (76 vs. 61 %, adjusted OR = 1.86, 95 % CI = 0.39–2.53, P < 0.001), diarrhea (34 vs. 29 %, adjusted OR = 3.76, 95 % CI = 0.95–6.53, P = 0.007), stomatitis (10 vs. 6 %, adjusted OR = 2.81, 95 % CI = 1.10–4.28, P = 0.002), and hand–foot syndrome (18 vs. 11 %, adjusted OR = 2.56, 95 % CI = 0.86–5.41, P = 0.045). Moreover, the URI group exhibited higher grade 3 to 4 toxicities. However, the difference between the two groups was not significant except diarrhea (20 vs. 11 %, adjusted OR = 1.53, 95 % CI = 0.45–4.89, P = 0.004) and stomatitis (6 vs. 3 %, adjusted OR = 2.14, 95 % CI = 0.89–3.26, P = 0.022) (Table 2). These higher toxicities resulted in more frequent dose modifications (52 vs. 26 %, adjusted OR = 1.72, 95 % CI = 1.21–2.05, P < 0.001) and prolonged dose interruptions (34 vs. 14 %, adjusted OR = 1.98, 95 % CI = 1.14–2.23, P < 0.001) in the URI group. Dose was interrupted in 52.0 and 28.0 % of the patients in the URI and control groups, respectively. Dose was modified in 34.0 and 13.9 % of the patients in the URI and control groups, respectively. In the URI group, four patients had more than two dosage reductions and one patient had three dose reductions. Approximately 14 % of the patients in the URI group were hospitalized because of insufferable toxicities, whereas only 5.3 % of the patients in the control group were hospitalized. The statistics of dose modifications, dose interruptions, and hospitalization of the renal function subgroup are summarized in Table 3.
Response and survival
The response rate was significantly lower in the URI group than in the control group (28 vs. 41 %, adjusted OR = 0.86, 95 % CI = 0.47–0.97, P = 0.004, Table 4). In addition, the patients in the URI exhibited significantly smaller median TTP (4.5 vs. 5.5 months, log-rank 7.259, P = 0.007, adjusted HR = 1.57, 95 % CI = 1.09–2.25, P = 0.015) and lower OS than those in the control group. However, the difference in OS between the two groups was not statistically significant (18.0 vs. 19.0 months, log-rank 1.534, P = 0.419, adjusted HR = 1.15, 95 % CI = 0.80–1.66, P = 0.442) (Fig. 2). Additional response and survival statistics are given in Table 4.
Discussion
A sizeable proportion of patients with cancer have renal dysfunction. Vincent [1] and Janus [2] indicated in their large-sample studies that the incidence of RI (CrCL < 90 ml/min) in cancer patients is approximately 50 to 60 %, 45 % of which is URI. Meanwhile, approximately 60 and 40 % of mCRC patients developed RI and URI, respectively. In certain medical disciplines, such as nephrology, the renal function is usually assessed based on the estimated CrCL. However, most oncologists still assess the renal function according to the SCr when starting chemotherapy [15], which may predispose an individual to increased systemic toxicity, particularly for the drugs mainly excreted through renal or with nephrotoxicity. The CapeOx regimen is commonly used as one of the first-line treatment in mCRC patients. Thus, we conducted this study to determine the effects of URI on the safety and efficacy of chemotherapy for CapeOx-treated mCRC patients.
A total of 143 patients with normal SCr were enrolled, of whom 34.9 % had URI defined as a CrCL of less than 60 ml/min. To the best of our knowledge, our case series is the largest among all studies that reported on the safety and efficacy of chemotherapy in URI patients. Significant differences were observed between the URI and control groups in the development of grade 1 to 2 toxicities, including cytopenia, diarrhea, stomatitis, and hand–foot syndrome. By contrast, grade 3 to 4 toxicities in the two groups were not statistically different. However, the duration of toxicities in URI group was longer. This result may be attributed to either the accumulation of capecitabine and its metabolites or the longer half-life of excretion in patients with URI. A higher proportion of patients with URI experienced dose interruptions and reductions, which probably resulted in decreased TTP. No statistically significant difference in OS was found between the two groups because of the relatively small sample size. However, we observed that patients with URI exhibited low survival rates based on the Kaplan–Meier curve (Fig. 2).
The Cockcroft–Gault and aMDRD equations are the most frequently used formulas to evaluate renal function [16, 17]. The aMDRD formula is suitable for patients >65 years of age, whereas the Cockcroft–Gault formula is suitable and more practical for patients younger than 65 years and who have normal SCr [18]. For cachexia, neither of the formulas is sufficiently precise [19]. We chose the Cockcroft–Gault formula for renal function evaluation by considering the age and estimated CrCL of the included patients.
Renal insufficiency has a major effect on capecitabine and its metabolites but has negligible effects on oxaliplatin excretion. Reigner et al. [20] investigated the pharmacokinetic characteristics of capecitabine and showed that RI can decrease the concentrations of the metabolites 5′-DFUR and FBAL. However, no evidence of an effect of RI on systemic exposure to 5-FU was observed. Pooled et al. [8] also confirmed that RI increases systemic exposure to 5′-DFUR and FBAL and observed an association between 5′-DFUR area under the curve and safety. However, clinical parameters, such as dose modifications, and the efficacy, including response and survival, were not evaluated in these studies. Only increased short-term toxicities were reported, but long-term toxicity data was still in lack.
The study demonstrated that URI was associated with high incidence of chemotherapy-related toxicities in mCRC and even decreased the efficacy of chemotherapy. That is, URI decreased response rate and TTP. The results emphasize the necessity for renal function monitoring of cancer patients using the estimated CrCL rather than SCr. Initial dosage adjustments may also be necessary. Thus, another issue was raised: whether dose reduction according to CrCL can limit drug-related adverse effects without any decrease in survival. The conclusions were not clear. SIGO recommends dosage adjustments of chemotherapy drugs in RI patients. However, most of the cited references were pharmacokinetic studies with small sample sizes because of the currently lacking evidence on the association between dosage adjustment and clinical treatment outcomes [11].
Our study has several limitations. First, the study represents the data of a single center and included only CapeOx-treated mCRC patients. Second, the study was designed in observational setting. We could not determine whether the dose reduction has an effect on safety and efficacy.
Despite of the limitations, our study still showed higher incidence of chemotherapy-related adverse effects and decreased TTP in mCRC patients with URI. Therefore, renal function monitoring via CrCL estimation is required for all mCRC patients prior to initial chemotherapy. Further prospective trials with large sample are required to verify the conclusion and determine the effects of dose reduction on the adverse effects and survival in cancer patients.
References
Launay-Vacher V, Oudard S, Janus N, Gligorov J, Pourrat X, Rixe O et al (2007) Prevalence of renal insufficiency in cancer patients and implications for anticancer drug management: the renal insufficiency and anticancer medications (IRMA) study. Cancer 110(6):1376–1384
Janus N, Launay-Vacher V, Byloos E, Machiels JP, Duck L, Kerger J et al (2010) Cancer and renal insufficiency results of the BIRMA study. Br J Cancer 103(12):1815–1821
Trobec K, Knez L, Mesko Brguljan P, Cufer T, Lainscak M (2012) Estimation of renal function in lung cancer patients. Lung Cancer 76(3):397–402
Launay-Vacher V, Gligorov J, Le Tourneau C, Janus N, Spano JP, Ray-Coquard I et al (2010) Prevalence of renal insufficiency in breast cancer patients and related pharmacological issues. Breast Cancer Res Treat 124(3):745–753
Launay-Vacher V, Ayllon J, Janus N, Spano JP, Ray-Coquard I, Gligorov J et al (2009) Drug management of prostate cancer: prevalence and consequences of renal insufficiency. Clin Genitourin Cancer 7(3):E83–E89
Launay-Vacher V, Chatelut E, Lichtman SM, Wildiers H, Steer C, Aapro M (2007) Renal insufficiency in elderly cancer patients: International Society of Geriatric Oncology clinical practice recommendations. Ann Oncol 18(8):1314–1321
Cassidy J, Clarke S, Diaz-Rubio E, Scheithauer W, Figer A, Wong R et al (2011) XELOX vs FOLFOX-4 as first-line therapy for metastatic colorectal cancer: NO16966 updated results. Br J Cancer 105(1):58–64
Poole C, Gardiner J, Twelves C, Johnston P, Harper P, Cassidy J et al (2002) Effect of renal impairment on the pharmacokinetics and tolerability of capecitabine (Xeloda) in cancer patients. Cancer Chemother Pharmacol 49(3):225–234
Massari C, Brienza S, Rotarski M, Gastiaburu J, Misset JL, Cupissol D et al (2000) Pharmacokinetics of oxaliplatin in patients with normal versus impaired renal function. Cancer Chemother Pharmacol 45(2):157–164
Takimoto CH, Remick SC, Sharma S, Mani S, Ramanathan RK, Doroshow JH et al (2003) Administration of oxaliplatin to patients with renal dysfunction: a preliminary report of the national cancer institute organ dysfunction working group. Semin Oncol 30(4 Suppl 15):20–25
Lichtman SM, Wildiers H, Launay-Vacher V, Steer C, Chatelut E, Aapro M (2007) International Society of Geriatric Oncology (SIOG) recommendations for the adjustment of dosing in elderly cancer patients with renal insufficiency. Eur J Cancer 43(1):14–34
Cockcroft DW, Gault MH (1976) Prediction of creatinine clearance from serum creatinine. Nephron 16(1):31–41
Levey AS, Eckardt KU, Tsukamoto Y, Levin A, Coresh J, Rossert J et al (2005) Definition and classification of chronic kidney disease: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int 67(6):2089–2100
Black RJ, Swaminathan R (1998) Statistical methods for the analysis of cancer survival data. IARC Sci Publ 145:3–7
Duncan L, Heathcote J, Djurdjev O, Levin A (2001) Screening for renal disease using serum creatinine: who are we missing? Nephrol Dial Transplant 16(5):1042–1046
National Kidney Foundation (2002) K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 39(2 Suppl 1):S1–S266
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of diet in renal disease study group. Ann Intern Med 130(6):461–470
Verhave JC, Fesler P, Ribstein J, du Cailar G, Mimran A (2005) Estimation of renal function in subjects with normal serum creatinine levels: influence of age and body mass index. Am J Kidney Dis 46(2):233–241
Bostom AG, Kronenberg F, Ritz E (2002) Predictive performance of renal function equations for patients with chronic kidney disease and normal serum creatinine levels. J Am Soc Nephrol 13(8):2140–2144
Reigner B, Blesch K, Weidekamm E (2001) Clinical pharmacokinetics of capecitabine. Clin Pharmacokinet 40(2):85–104
Acknowledgments
We appreciate the financial support of the Natural Science Foundation of China for Youth (Grant number: 81301892).
Conflict of interest
The authors declare that they have no other conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, J., Wang, Xt., Luo, Ph. et al. Effects of unidentified renal insufficiency on the safety and efficacy of chemotherapy for metastatic colorectal cancer patients: a prospective, observational study. Support Care Cancer 23, 1043–1048 (2015). https://doi.org/10.1007/s00520-014-2461-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-014-2461-3