Abstract
Purpose
This study aims to clarify the length of home hospice care, family-perceived timing of referrals, and their effects on the family-perceived quality of care and quality of death and dying of terminally ill cancer patients who died at home and identify the determinants of perceived late referrals.
Methods
A multicenter questionnaire survey was conducted involving 1,052 family members of cancer patients who died at home supported by 15 home-based hospice services throughout Japan.
Results
A total of 693 responses were analyzed (effective response rate, 66 %). Patients received home-based hospice care for a median of 35.0 days, and 8.0 % received home hospice care for less than 1 week. While 1.5 % of the families reported the timing of referrals as early, 42 % reported the timing as late or too late. The families of patients with a length of care of less than 4 weeks were more likely to regard the timing of referrals as late or too late. The patients of family members who regarded the timing of referrals as late or too late had a significantly lower perceived quality of care (effect size, 0.18; P = 0.039) and lower quality of death and dying (effect size, 0.15, P = 0.063). Independent determinants of higher likelihoods of perceived late referrals included: frequent visits to emergency departments, patient being unprepared for worsening condition, and patient having concerns about relationship with new doctor. Discharge nurse availability was independently associated with lower likelihoods of perceived late referrals.
Conclusions
A significant number of bereaved families regarded the timing of referrals to home hospices as late, and the perceived timing was associated with the family-perceived quality of care and quality of death and dying. Systematic strategies to overcome the barriers related to perceived late referrals are necessary.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
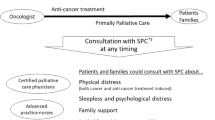
Several studies have revealed that hospice care contributes to increased opportunities to die at home, a reduced frequency of emergency department visits, and improved satisfaction of both patients and their families [1–3]. Multiple surveys from several countries, however, have consistently shown that physicians referred patients to hospice care services at the very latest stage of cancer: the median interval from referral to patient death ranged from 2 to 6 weeks and about 15 to 35 % of the patients died within a week after referral [4–11]. Some studies demonstrated that a shorter length of hospice enrollment was associated with an increased risk of major depressive disorder in family caregivers, less satisfaction with hospice care of family caregivers, and inadequate symptom management [9, 12–16]. Another recent study clarified that patients who received less than a week of hospice care had the same quality of life as patients who did not receive hospice care at all [17].
On the other hand, some studies identified that the family-perceived timing of referrals, not the length of receiving hospice care itself, was significantly correlated with the family-perceived quality of care [4, 6]. Many studies stressed the importance of appropriate referral to a hospice and/or palliative care service to identify unmet needs early, alleviate pain and suffering appropriately, and strengthen emotional connections between patients and their families [18–21]. Recent studies revealed that early hospice and/or palliative care referral improves patients’ understanding of the prognosis over time, which may improve end-of-life decision-making [22, 23].
The factors contributing to late referrals are associated with patients, families, physicians, and health care systems [24–28]. To date, empirical studies on healthcare providers have identified multiple barriers to appropriate referrals: patients’/families’ unwillingness to receive hospice care, patients’/families’ misconceptions about hospices, physicians’ unwillingness to discuss end-of-life care, and a lack of hospice care services available [24–28]. Although these findings provide useful information to understand why physicians do not refer patients to hospice care services at an earlier stage of cancer, only small numbers of systematic studies have still been performed to directly collect the views of terminally ill patients with cancer or their families. A recent qualitative study in the USA clarified that the reasons for family-perceived late referrals were centered on concerns with the healthcare providers’ role in decision-making, with the main concerns being inadequate with communication physicians and not recognizing that the patient is dying [29]. On the other hand, to our best knowledge, no quantitative empirical studies have investigated factors influencing the perceived timing of hospice referral in terms of the actual experiences of families of cancer patients who received home hospice care and died at home.
In Japan, home care is provided by three types of medical facility in collaboration with home-visiting nurses: physicians working at clinics, clinics with a home hospice function (focusing on delivering home care rather than outpatient care), and home care divisions of hospitals [30]. Eligible criteria for home care service are patients who cannot visit outpatient medical facilities and principally terminally ill patients. Typically, if a patient’s condition is relatively stable, a physician visits the patient’s home weekly and home-visiting nurses visit the home one to three times per week. For imminently dying patients or patients with marked symptoms, physicians and nurses visit every day when needed, and 24-h 7-day call-out is available. Common medical procedures, such as subcutaneous infusion and home parenteral nutrition using an implantable central venous access device, are available. When discharged from hospital, a discharge nurse arranges services at home required for the patient. Daily life at home is assisted by home helpers covered by the national long-term care insurance, in addition to family caregivers. Respite care is provided by nursing homes, palliative care units, or hospitals. If patients want to be admitted to hospitals, admission is generally possible. Very recently, the government has been trying to develop more efficient home care services through modifying laws, healthcare systems, and multiple educational or cooperative projects. Nevertheless, investigations of referrals to home hospices with a focus on the length and timing among terminally ill Japanese patients with cancer in a home hospice setting have yet to be performed.
The primary aims of this study were: (1) to clarify the length of home hospice care, family-perceived timing of referrals, and their associations in terminally ill cancer patients who died at home, (2) explore the effects of the length of home hospice care and family-perceived timing of referrals on perceived quality of care and quality of death and dying, and (3) identify the determinants of perceived late referrals. The ultimate aim was to identify ways to promote appropriate referrals to home hospice care for patients with advanced cancer.
Subjects and methods
This is a part of a large nationwide survey of bereaved family members of cancer patients (Japan Hospice and Palliative care Evaluation study: J-HOPEII [31], and a multicenter questionnaire survey was conducted involving bereaved family members of cancer patients who died at home. We mailed questionnaires to bereaved families in June 2007 and again in August 2007 to nonresponding families. The return of the completed questionnaire was regarded as consent to participate in this study. Ethical and scientific validity was confirmed by the institutional review boards of all participating institutions.
Settings and subjects
Participating institutions were recruited from home-based hospice services belonging to the Japan Hospice Association. Among all 37 home-based hospice services belonging to the Association, a total of 15 agreed to participate in this survey.
Primary responsible physicians identified potential participants following the inclusion criteria: (1) bereaved family members of an adult cancer patient (one family member was selected for each patient), (2) aged 20 or older, (3) capable of replying to a self-reported questionnaire, and (4) aware of the diagnosis of malignancy. Exclusion criteria included: (1) inability to complete the questionnaire (dementia, cognitive failure, psychiatric illness, language difficulty, or visual loss), (2) severe emotional distress of the family, as determined by the primary responsible physicians, (3) treatment-associated death or death from comorbidity, (4) death in intensive care units, and (5) no family member unavailable. The second criterion was, as in our previous studies [32–35], adopted on the assumption that primary responsible physicians could identify families who may suffer a serious psychological impact due to the present study, and no formal criteria or psychiatric screening was applied. Families were surveyed 6 to 12 months after the patients’ deaths.
Questionnaire
The questionnaire was developed by the authors on the basis of a literature review [5, 8, 9, 12–21, 24–29], interviews, and focus groups involving healthcare professionals and 28 bereaved family members.
Length of care and family-perceived timing of referrals
The primary end-points were the length of home hospice care and family-perceived appropriateness of the timing of physicians’ referrals of patients to home hospice services. The former data were obtained from each hospice service. The latter were measured using the same methods as in previous studies [5, 8]. The level of the family-perceived appropriateness was rated on a 5-point scale: “should have been referred much later (very early),” “should have been referred a little later (early),” “referred at the appropriate time,” “should have been referred a little earlier (late),” and “should have been referred much earlier (too late).”
Family-perceived quality of care
The family members were asked to rate their perceived quality of palliative care of responsible facilities when the patient died. Family-perceived quality of care was measured using the Care Evaluation Scale, a well-validated and the most commonly used measurement tool to quantify user-perceived quality of palliative care in Japan [36]. This consists of eight subdomains: (1) physical care provided by physicians, (2) physical care provided by nurses, (3) psycho-existential care, (4) help with decision-making, (5) coordination/consistency of care, (6) environment, (7) cost, and (8) availability. Each subscale had two or three items graded with a 6-point Likert-type scale, from “1: improvement is markedly necessary” to “6: improvement is not necessary at all,” and the total score of the Care Evaluation Scale was defined as the mean of all subdomain scores. Higher values indicated a lower perceived necessity of improvement, with a range of 1 to 6.
Quality of death and dying
The family members were asked to rate the quality of death and dying over the last month of the patient’s life. The quality of death and dying was measured using the Good Death Inventory, a measure of the quality of death and dying of patients with advanced cancer [37]. The full version of this scale was used, consisting of ten domains: (1) physical and psychological comfort, (2) living in one’s favorite place, (3) maintaining hope and pleasure, (4) having a good relationship with medical staff, (5) not feeling a burden to others, (6) having a good relationship with the family, (7) having independence, (8) living in a comfortable environment, (9) being respected as an individual, and (10) a feeling of fulfillment at life’s completion. Each item was assessed using a 7-point Likert-type scale, from “1: strongly disagree” to “7: strongly agree,” and the total score was defined as the mean of all subdomain scores. Higher values indicated a higher perceived quality of death and dying, with a range of 1 to 7.
Factors contributing to perceived timing of referrals
Family members were asked to rate the level of agreement with nine statements (yes or no) and six statements (strongly disagree, 1 to strongly agree, 5) as potential factors contributing to their perceived timing of referrals (Table 4). In addition, negative perceptions of home hospices were examined using the mean level of agreement for seven statements: symptoms cannot be sufficiently alleviated at home, home care cannot adequately respond to sudden changes out of hours, home-visit doctors are unavailable, home care causes a heavy family burden, staying at home is expensive, hospital beds are unavailable even if necessary, and patients cannot receive better treatment at home than at hospitals. Each item was rated on a 4-point Likert-type scale, from strongly disagree (1) to strongly agree (4), and the score was calculated as the mean score for each item. A higher score thus indicates a more negative perception of home care, with a range of 1 to 4. Cronbach’ alpha was 0.81, and factor analysis identified one factor.
Analyses
We initially calculated the frequency with 95 % confidence intervals for the length of home hospice care and family-perceived timing of referrals. Then, the percentages of the respondents who reported that referrals were late or too late were calculated with 95 % confidence intervals for five groups with a different length of care (<1 week, 1 week to less than 2 weeks, 2 weeks to less than 4 weeks, 4 weeks to less than 8 weeks, and 8 weeks or longer). Secondly, we compared the scores for the perceived quality of care and quality of death and dying between the patients with a length of care of less than 2 vs. 2 weeks or longer, patients with a length of care of less than 4 vs. 4 weeks or longer, and patients with family-perceived late or too late referrals vs. appropriate; the respondents with early and too early perceived timings of referrals were excluded from further analysis. Comparisons were performed using Student’s t test. We calculated Hedges’ g to estimate the effect size, and effect sizes of 0.2, 0.5, and 0.8 were regarded as small, moderate, and large effects, respectively [38, 39]. Thirdly, we compared demographic data and factors contributing to the perceived timing of referrals using univariate logistic regression analysis to screen, followed by multivariate logistic regression analysis. All variables with P values of 0.10 or less were entered into the model, and a step-forward elimination method was adopted. The P value regarded as significant was 0.050. All analyses were performed using the Statistical Package for the Social Sciences (ver. 11.0).
Results
A total of 1,120 family members met the inclusion criteria, and 68 of them were excluded according to the exclusion criteria. We thus sent our 1,052 questionnaires, and 723 (70 %) were returned, with 24 returned due to the wrong address. Of those, 25 refused to reply. Therefore, we obtained a total of 698 responses. For the present study, as five responses were excluded due to missing data on the length of care, we finally analyzed 693 (66 %) responses. Background characteristics are summarized in Table 1.
Length of care and family-perceived timing of referrals
Patients received home-based hospice care for a median of 35.0 days (range, 3 to 1,307 days). A total of 8.0 % of the patients received home hospice care for less than 1 week, and 21 % received it for less than 2 weeks (Table 2). While the number of family members who reported that the timing of referrals was early or too early was very small, being 1.5 %, 42 % reported that the timing was late or too late, and the remaining 56 % of the family members reported that the timing was appropriate, (Table 2).
Association between length of care and family-perceived timing of referrals
There were significant differences in the rates of those who reported that the timing was late or too late among the patients with different lengths of care (P < 0.0001; Fig. 1). The family members of patients with a length of care of less than 4 weeks were more likely to report that the timing of referrals was late or too late compared to those with care of 4 weeks or more. The rates of family members who reported that the timing of referrals was late or too late were: 60 % (<1 week), 58 % (1 week to less than 2 weeks), 50 % (2 weeks to less than 4 weeks), 34 % (4 weeks to less than 8 weeks), and 36 % (8 weeks or longer).
Effects of length of care and perceived timing of referrals on family-perceived quality of care and quality of death and dying
There were no significant differences in the family-perceived quality of care and quality of death and dying between the patients with different lengths of care (Table 3). The family members who regarded the timing of referrals as late or too late were significantly more likely to report a lower quality of care (P = 0.039), and poorer quality of death and dying with marginal significance (P = 0.063). The effect sizes were 0.18 and 0.15, and the difference was considered as marginal to small.
Determinants of family-perceived timing of referrals
Univariate analyses revealed that the perceived timing of late referrals was significantly correlated with frequent visits to emergency departments, patient being unprepared for worsening condition, and family being unprepared for worsening condition (Table 4). On the other hand, primary tumor sites of the prostate, kidney, and bladder, symptoms adequately relieved, discharge nurse being available, and the patient wanting a hospital doctor was to perform treatment were significantly correlated with lower likelihoods of perceived late referrals (Table 5).
Independent determinants of higher likelihoods of perceived late referrals included frequent visits to emergency departments, patient being unprepared for worsening condition, and patient having concerns about relationship with new doctor. A discharge nurse being available and the patient wanting a hospital doctor to perform treatment were independently associated with lower likelihoods of perceived late referrals. The item of the patient being unprepared for the worsening condition was moderately associated with the item of the family being unprepared (rho = 0.43), and, thus, if the former item was excluded from the model then the latter was included.
Discussion
This is one of large studies investigating the appropriateness of the timing of referrals to home hospice care for terminally ill cancer patients who received palliative care and died at home.
The first important finding of the present study was clarification of the situation regarding the family-perceived timing of referrals to home hospice care. Less than 2 % of families reported that the timing of referrals was early or too early, and 42 % reported that the timing was late or too late. The median length of referral from hospital to death at home was 35 days, and approximately 10 % of the patients died within 1 week. These findings are generally consistent with the existing literature, reporting that patients were referred to home hospice care at a late stage of cancer [4–11]. The fact that over 40 % of family members responded that the timing of referrals was late or too late suggests that the timing of referrals to home hospice care is likely to be delayed, and a strategy needs to be developed to improve this situation.
A novel finding of this study was that, whereas the length of care itself did not significantly influence the family-perceived quality of care or quality of death and dying, the family-perceived timing of a late referral was correlated with family-perceived quality of care, and the quality of death and dying. These findings suggest that it is not the length of receiving hospice care itself but rather the family-perceived timing of referral to home hospice care that should be considered as an indicator of the quality of end-of-life care.
Moreover, this is, to our knowledge, the first study to identify determinants of the family-perceived timing of referrals in terminally ill patients with cancer. Among the five determinants identified for late referral, two of them are within the context of the patient-physician relationship. Especially, concern over the relationship with a new physician was significantly associated with a greater likelihood of perceived late referrals. Because of the lack of a home physician or general practitioner system in Japan, patients generally sever strong ties with hospital physicians over the course of their disease. When patients receive home hospice services, therefore, they have to establish entirely new relationships with home-visiting physicians and nurses. Recently, efforts were made in Japan to increase communication and interactions and nurture relationships among physicians at a regional level, such as through whole-region interdisciplinary conferences [40]. A recent study revealed that a display of social intimacy between a hospital physician and home hospice physician was one of the determinants of a family’s evaluation of physicians’ communication when patients were referred to a home hospice [41]. Improving regional interaction between hospital physicians and home-visiting physicians may be a promising solution to late referrals to home hospices.
We also identified that discharge nurse availability was a key for decreasing likelihoods of perceived late referrals. Multiple studies have indicated that many patients with life-limiting illnesses were discharged without appropriate proactive management in their homes, and they eventually died in acute care hospitals [42, 43]. Many studies have also stressed the importance of discharge planning and the development of transitional care from a hospital to the home, and so the process of discharge planning is often complex and requires early initiation just after a patient's admission [43, 44]. The findings of this study highlights that discharge nurses play an important role in reducing the risk of delaying the timing of referral to a home hospice.
In addition, as the patients and families who reported frequent visits to emergency rooms and were unprepared for the worsening condition, this population should be a target for improving the timing of referrals to home hospices. A feasible screening system followed by appropriate triage for such a selected population may be of value, although frequent emergency visits could be simply the result of a lack of enrollment in a hospice program.
Despite the strength of the present study regarding the success in obtaining a relatively large sample and the use of validated measurements of perceived quality of care and quality of death and dying, the present study has several limitations. Firstly, home services participating in this study were generally well-organized and belonged to a national association. The findings might not be applicable to other smaller services. Secondly, the study subjects were the families of patients, and so the patients’ views might have been different. Thirdly, the questions about factors potentially contributing to the perceived timing of hospice referrals used in this study were ad hoc and did not undergo formal validation testing. Fourthly, the reason why the Care Evaluation Scale and Good Death Inventory did not correlate with the actual timing of hospice referrals may be the ceiling effects of these scales, resulting in limited sensitivity, and/or the exclusion of patients who died in intensive care units. These limitations should be explored in future studies.
In conclusion, more than 40 % of bereaved Japanese families receiving home hospice care regarded the timing of referrals as late or very late, while less than 2 % reported it as early. Independent determinants of higher likelihoods of perceived late referrals included: frequent emergency department visits, patient being unprepared for worsening condition, and patient having concerns about relationship with new doctor. Systematic strategies to overcome these barriers should be explored to promote appropriate referrals to home hospices.
References
Finlay IG, Higginson IJ, Goodwin DM et al (2002) Palliative care in hospital, hospice, at home: results from a systematic review. Ann Oncol 4:257–264
Brumley R, Enguidanos S, Jamison P et al (2007) Increased satisfaction with care and lower costs: results of a randomized trial of in-home palliative care. J Am Geriatr Soc 55:993–1000
Drieskens K, Bilsen J, Van Den Block L et al (2008) Characteristics of referral to a multidisciplinary palliative home care team. J Palliat Care 24:162–166
Poulose JV, Do YK, Neo PS et al (2013) Association between referral-to-death interval and location of death of patients referred to a hospital-based specialist palliative care service. J Pain Symptom Manag 46(2):173–181
Morita T, Akechi T, Ikenaga M et al (2005) Late referrals to specialized palliative care service in Japan. J Clin Oncol 23(12):2637–2644
Teno JM, Shu JE, Casarett D et al (2007) Timing of referral to hospice and quality of care: length of stay and bereaved family members' perceptions of the timing of hospice referral. J Pain Symptom Manag 34(2):120–125
Schockett ER, Teno JM, Miller SC et al (2005) Late referral to hospice and bereaved family member perception of quality of end-of-life care. J Pain Symptom Manag 30(5):400–407
Morita T, Miyashita M, Tsuneto S et al (2009) Late referrals to palliative care units in Japan: nationwide follow-up survey and effects of palliative care team involvement after the Cancer Control Act. J Pain Symptom Manag 38(2):191–196
Stillman MJ, Syrjala KL (1999) Differences in physician access patterns to hospice care. J Pain Symptom Manag 17:157–163
Costantini M, Toscani F, Gallucci M et al (1999) Terminal cancer patients and timing of referral to palliative care: a multicenter prospective cohort study. J Pain Symptom Manag 18:243–252
Morita T, Chihara S, Kashiwagi T (2002) Family satisfaction with inpatient palliative care in Japan. Palliat Med 16:185–193
Kris AE, Cherlin EJ, Prigerson H et al (2006) Length of hospice enrollment and subsequent depression in family caregivers: 13-month follow-up study. Am J Geriatr Psychiatr 14(3):264–269
Bradley EH, Prigerson H, Carlson MD et al (2004) Depression among surviving caregivers: does length of hospice enrollment matter? Am J Psychiatry 161(12):2257–2262
Lamont EB, Christakis NA (2002) Physician factors in the timing of cancer patient referral to hospice palliative care. Cancer 94:2733–2737
Medicare: more beneficiaries use hospice but for fewer days of care. Washington, DC, United States General Accounting Office 2000
Christakis NA, Escarce JJ (1996) Survival of medicare patients after enrollment in hospice programs. N Engl J Med 335:172–178
Wright AA, Zhang B, Ray A et al (2008) Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA 300(14):1665–1673
Ashbury FD, Findlay H, Reynolds B, McKerracher K (1998) A Canadian survey of cancer patients’ experiences: are their needs being met? J Pain Symptom Manag 16:298–306
Casarett D, Abrahm JL (2001) Patients with cancer referred to hospice versus a bridge program: patient characteristics, needs for care, and survival. J Clin Oncol 19:2057–2063
Dudgeon DJ, Raubertas RF, Doerner K et al (1995) When does palliative care begin? A needs assessment of cancer patients with recurrent disease. J Palliat Care 11:5–9
Emanuel LL, Alpert HR, Emanuel EE (2001) Concise screening questions for clinical assessments of terminal care: the needs near the end-of-life care screening tool. J Palliat Med 4:465–474
Temel JS, Greer JA, Muzikansky A et al (2010) Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 363(8):733–742
Temel JS, Greer JA, Admane S et al (2011) Longitudinal perceptions of prognosis and goals of therapy in patients with metastatic non-small-cell lung cancer: results of a randomized study of early palliative care. J Clin Oncol 29(17):2319–2326
Casarett DJ, Marenberg ME, Karlawish JH (2001) Predictors of withdrawal from hospice. J Palliat Med 4:491–497
Friedman BT, Harwood MK, Shields M (2002) Barriers and enablers to hospice referrals: an expert overview. J Palliat Med 5:73–84
Ogle KS, Mavis B, Wyatt GK (2002) Physicians and hospice care: attitudes, knowledge, and referrals. J Palliat Med 5:85–92
Pugh EM (1996) An investigation of general practitioner referrals to palliative care services. Palliat Med 10:251–257
Weggel JM (1999) Barriers to the physician decision to offer hospice as an option for terminal care. WMJ 98:49–53
Teno JM, Casarett D, Spence C et al (2012) It is "too late" or is it? Bereaved family member perceptions of hospice referral when their family member was on hospice for seven days or less. J Pain Symptom Manag 43(4):732–738
Morita T, Kizawa Y (2013) Palliative care in Japan: a review focusing on care delivery system. Curr Opin Support Palliat Care 7(2):207–215
Miyashita M, Morita T, Hirai K et al (2008) Evaluation of end-of-life cancer care from the perspective of bereaved family members: the Japanese experience. J Clin Oncol 26(23):3845–3852
Shinjo T, Morita T, Hirai K et al (2010) Care for imminently dying cancer patients: family members' experiences and recommendations. J Clin Oncol 28(1):142–148
Yamagishi A, Morita T, Miyashita M et al (2010) The care strategy for families of terminally ill cancer patients who become unable to take nourishment orally: recommendations from a nationwide survey of bereaved family members' experiences. J Pain Symptom Manag 40(5):671–683
Morita T, Akechi T, Ikenaga M et al (2004) Communication about the ending of anticancer treatment and transition to palliative care. Ann Oncol 15(10):1551–1557
Yamagishi A, Morita T, Miyashita M et al (2012) Preferred place of care and place of death of the general public and cancer patients in Japan. Support Care Cancer 20(10):2575–2582
Morita T, Hirai K, Sakaguchi Y et al (2004) Measuring the quality of structure and process in end-of-life care from the bereaved family perspective. J Pain Symptom Manag 27:492–501
Miyashita M, Morita T, Sato K et al (2008) Good death inventory: a measure for evaluating good death from the bereaved family member's perspective. J Pain Symptom Manag 35:486–498
Hedges LV, Olkin I (1985) Statistical methods for meta-analysis. Academic Press, Orlando
Cohen J (1992) A power primer. Psychol Bull 112:155–159
Morita T, Miyashita M, Yamagishi A et al (2013) Effects of a programme of interventions on regional comprehensive palliative care for patients with cancer: a mixed-methods study. Lancet Oncol 14(7):638–646
Yamagishi A, Morita T, Kawagoe S et al Communication about home hospice referral for patients and families of terminally ill cancerpatients: recommendations from a nationwide survey of bereaved family members’ experiences. Gan to kagaku ryoho (in press, abstract is available in PUBMED in English)
Wilkinson S (2000) Fulfilling patients’ wishes: palliative care at home. Int J Palliat Nurs 6:212
Bowles KH, McCorkle R, Nuamah IF (2008) Homecare referrals and 12-week outcomes following surgery for cancer. Oncol Nurs Forum 35:377–383
Hirabayashi Y, Miyashita M, Kawa M et al (2007) Factors relating to terminally ill cancer patients’ willingness to continue living at home during the early phase of home care after discharge from clinical cancer centers in Japan. Palliat Support Care 5:19–30
Conflict of interest
This study was funded by the Japan Hospice Palliative Care Foundation in Japan. The authors have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yamagishi, A., Morita, T., Kawagoe, S. et al. Length of home hospice care, family-perceived timing of referrals, perceived quality of care, and quality of death and dying in terminally ill cancer patients who died at home. Support Care Cancer 23, 491–499 (2015). https://doi.org/10.1007/s00520-014-2397-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-014-2397-7