Abstract
Purpose
Febrile neutropenia (FN) remains a common and dangerous complication of cancer treatment. Guidelines from the Infectious Disease Society of America urge initiating antibiotics within 2 h of presentation. We reviewed our institution’s performance to identify areas of needed improvement and to design performance improvement steps.
Methods
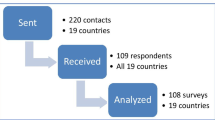
FN management was deconstructed into discrete tasks. Experienced practitioners estimated appropriate time allowance for each task. Cycle time analysis data on a baseline cohort (baseline group) identified causes and loci of delay. Based on these data, new processes to bypass roadblocks for timely therapy were introduced. Performance monitoring continued as these changes were implemented (the transitional group) and for 20 months thereafter (the post-intervention group).
Results
Sixty-nine episodes of FN were identified. Ten distinct improvement steps were implemented. Median time to antibiotics was reduced from 252 min, to 188 min and 118 min for the baseline, transitional, and post-intervention groups, respectively (p = 0.0002 for the baseline vs. the post-intervention group comparison). Variability was reduced with the inter-quartile range falling from 174 min (baseline) to 65 min (post-intervention). Despite improvement, there were persisting episodes of delays, due to competing priorities from other patients or decisions to postpone infusion of antibiotics until patients had been admitted. Standardized order sets eliminated improper antibiotic choices as a source of error.
Conclusions
Improvements in the management of FN can be accomplished and sustained by the focused study of performance of individual tasks, the design of streamlined processes by practitioners, and the ongoing review of performance with feedback to clinical departments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Febrile neutropenia (FN) remains a common and serious complication of many cancer chemotherapies. Data from the 1999 Surveillance and Epidemiology End Result (SEER) program and National Cancer Data Base showed an annual incidence of more than 60,000 cases in the USA with a mortality rate of 6.8 % [1]. A review of more than 41,000 admissions for FN treated between 1995 and 2000 identified a mortality rate ranging from 2.6 % (with no co-morbidities) to 50.6 % (with five co-morbidities) [2]. The same study found mean hospital charges per episode of $19,110 [2]. Outcomes of FN are influenced by individual patient characteristics such as age, co-morbidities, depth and duration of neutropenia, and the presence or absence of positive blood cultures or documented infection [3]. Although guidelines promulgated by the Infectious Disease Society of America (IDSA) recommend initiation of antibiotics within 2 h of patient presentation [4], there is limited published data on the clinical importance of this recommendation. One retrospective study among patients with clinically defined septic shock demonstrated that survival declines with delays of antibiotics. Each hour of hypotension without effective antibiotics was associated with an average decrease in survival of 7.6 % [5]. Even though only 6.8 % of the patients in that study had neutropenia, the 2-h standard has been set empirically as a goal in recognition that rapid deterioration is possible. Organizing hospital services to meet this 2-h standard is a challenge especially where FN is seen infrequently, creating few opportunities to develop and implement best practice paradigms.
We conducted a review of our hospital’s performance in the treatment of FN after anecdotal evidence indicated that our services were failing the IDSA standard with regard to timeliness of antibiotics and choice of appropriate antibiotics. We used cycle time analysis data and interviews with practitioners in the relevant clinical areas most involved to design new processes to bypass impediments to timely therapy. This report describes the frequency and causes of failure in the original and subsequent cohorts, the measures taken to improve outcomes, and the results of those actions over time.
Patients and methods
This project was part of a performance improvement project. The project was approved by the Institutional Review Board. Anne Arundel Medical Center is a 385-bed acute care facility with over 1,900 new cancer patients seen yearly. Approximately, ten full-time equivalent hematologists-oncologists practice on or near the hospital campus seeing approximately 120 patients a day. A campus-based outpatient infusion center treats over 70 cancer patients a day and a nearby private practice treats up to 8 patients daily. The 30-bed inpatient oncology unit has an average census of 18 oncology patients. The emergency department (ED) is staffed by a private practice medical group comprising 18 physicians and a combined total of 7 nurse practitioners and physician assistants. The emergency department sees nearly 100,000 patient visits annually. No students or residents participated in the care of the patients described in this report.
We performed a mixed methodology analysis of the management of FN at our institution. We convened a FN task force composed of representatives from the inpatient oncology unit, ED, outpatient infusion center, oncology practices, hospital laboratory, hospital epidemiology, and pharmacy to analyze results of a retrospective cycle time review of the management of FN over an 18-month period in 2010–2011 (designated the baseline group). As part of this review, the task force characterized the specific processes in which errors or delays occurred. We included in the analysis patients who were admitted either directly from one of the oncology clinics, from the ED, or patients who became febrile once already admitted. Because the IDSA guideline is specific for patients with both fever (defined as temperature ≥38.3 °C or ≥38.0 °C sustained over 1 h) and neutropenia (defined as <500 neutrophils/mm3 or counts expected to decrease to that level over the ensuing 48 h) [4], we did not include patient records where only one of these parameters was present upon presentation. We analyzed how often the care met the IDSA standards for timeliness and appropriateness of antibiotics. We used the time mark detail present in the electronic medical record (EPIC, version 2010, Madison, WI, USA) to determine the actual process steps in which delays occurred, assigning them to one or more categories. To accomplish this, we arbitrarily assigned an acceptable process time of 30 min for the following tasks each of which is composed of several component steps: from presentation in the ED to delivery of the blood specimen to the lab, from receipt in the lab to release of results to the electronic medical record, from release of blood count results to completion of the antibiotic orders, and, finally, from completion of the antibiotic orders to administration of the antibiotics. The neutropenic task force assessed the modes of failure and determined best practices in the context of a busy ED or clinic in order to design education, interventions, and new processes to address each of the deficiencies. We continued to monitor performance on all similar patients while we instituted changes over a 9-month timeframe in 2011 (the transitional group) and then for 20 months in 2012–2013 after the interventions (post-intervention period). The standard process for febrile neutropenia at this hospital involves initial admission of all documented cases of febrile neutropenia even those at low risk.
Statistical methods
Descriptive statistics were computed for the three time intervals (groups) including means and quartiles. The medians for the three groups were compared pair-wise using the Wilcoxon method. The statistical package used was JMP 9.0.2, SAS Institute Inc., Cary, NC, USA.
Results
Ninety-five patients who developed fever with some degree of neutropenia were identified from admission rosters but only 69 of these had simultaneous fever (temperature ≥38.3 °C or ≥38.0 °C sustained over 1 h) and deep neutropenia (absolute neutrophil count <500/mm3) present at the time of presentation and were included in the analysis. Table 1 shows the characteristics of the 69 patients from each of the three cohorts: baseline, transitional, and post-intervention. The vast majority of patients were first evaluated in the ED setting and had clinical characteristics consistent with a low risk Multinational Association of Supportive Care in Cancer (MASCC) score [6]. Only two patients had been on antibiotics either as empiric therapy or as prophylaxis when they became febrile. Three patients in the baseline group had non-recommended, non-standard antibiotic regimens prescribed by three distinct ED providers: two receiving intravenous azithromycin and one patient receiving cefuroxime.
Table 2 describes the specific process steps at which errors or delays contributed to failure to meet the IDSA standards for each of three groups. In many cases, more than one step was delayed. Table 3 lists the specific improvements introduced during the 9-month transitional period based upon review of the causes of failure in the baseline group and a map of best practices. Figure 1 shows the results of the time to antibiotics analyses for each of the three groups demonstrating a reduction in the median time to antibiotics from time of patient arrival from 252 min in the baseline group, 188 min in the transitional group to 117 min in the post-intervention group. The difference between the baseline group and the post-intervention group was statistically significant (p = 0.0002) as was the difference between the medians of the transitional group and the post-intervention group (p = 0.04). The difference between the medians of the baseline and transitional groups was not statistically significant (p = 0.12). In addition to improvements in the median time of antibiotics, there was also a large reduction in the variability of performance as evidenced by a reduction in the inter-quartile range from 174 min in the baseline group to 65 min in the post-intervention group. The longest delays were due to a decision to hold the administration of antibiotics until the patient had been transferred to an inpatient unit. Of the patients whose time to antibiotics was greater than 5 h, the holding of antibiotics until transfer was the main cause of delay in 6/7 in the baseline group, 2/2 in the transitional group, and in the single patient beyond 5 h in the post-intervention group.
Discussion
The optimum management of FN begins with educating patients and caregivers on the importance of self-monitoring of temperatures and immediate reporting of temperature or related symptoms such as chills or rigors. Once a patient presents, it is imperative that the health care team recognize patients at risk, perform prompt clinical and laboratory assessment, and ensure rapid delivery of broad-spectrum antibiotics informed by local sensitivity patterns. Such coordinated action requires a sense of urgency from a diverse medical team: nurses, physicians, medical assistants, laboratory technicians, and pharmacists. Breakdown in any of the steps can results in delays and inferior outcomes. With the exception of the few patients who present to ambulatory clinics or who develop FN while already hospitalized, most of these action steps take place in the emergency department, an environment not under the direct supervision of hematologists-oncologists.
Our data shows that baseline performance at our institution was poor with regard to timeliness, variability in response, and included three patients who received antibiotic combinations more suitable for non-neutropenic infections. These data are similar to baseline performance reported from around the world. A study of multiple UK hospitals found median “door to needle” time that ranged from 0.5 to 4 h and “long delays over 5 hours were not uncommon.” [7]. Other studies have showed median time to antibiotics of 3 h and 36 min [8], 5 h [9], and 3.5 h [10] of which 1.25 h was taken up by waiting for a medical assessment.
Table 2’s catalog of process steps in which errors occurred was made possible by the time stamps available in the electronic medical record. We identified delays at almost every step in the process. This finding is similar to those of Clarke et al. [7], who used both treatment audits and staff feedback to generate a list of problematic categories: lack of staff, lack of understanding, practical problems, and communication issues. We found some of the same errors, but our electronic medical record time stamp methodology did not allow us to distinguish between a delay due to relative staffing shortage or lack of understanding of medical urgency. The longest delays that we experienced were a consequence of the conscious or functional decision to pause the delivery of antibiotics while awaiting transfer to an inpatient unit. These transfers can be delayed for a variety of causes both at the receiving unit and in the ED and can be lengthy, 5.5 h in one study [10]. This pattern of practice is a result of lack of appreciation for the pathophysiology of infection and potential sepsis. It should be a prime target of training efforts for all staff involved in the care of FN patients.
Our improvement steps were informed both by analysis of our own actual performance breakdowns and by mapping of best practices by leaders of the clinical areas. We did not rely upon education alone to improve outcomes, an unreliable method for addressing root cause problems [11]. Rather, we buttressed patient, caregiver, and staff education with new tools. Among the most important of these steps was the ordering of blood counts “stat” and allowing the lab to release preliminary results of white blood cell counts to the treating physicians without awaiting manual confirmation by a laboratory technician. Our experience was that the manual review always confirmed the automated blood count and therefore added no new information to justify this delay. Standardized electronic order sets for FN ensured universal ordering of blood cultures prior to antibiotics and ensured that the antibiotic regimens were consistent with the 2011 IDSA guideline [4] including an option for penicillin-allergic patients. Locating appropriate antibiotic drugs in ready-to-administer form available inside the ED in automated dispensers bypassed the time needed for the antibiotic order to be recognized, prepared in the pharmacy, and then transported from the pharmacy.
Educational efforts did succeed in increasing the awareness of FN as an urgent situation and, for the most part, reduced the execution time of certain tasks such as completing the medical assessment and the drawing of blood. However, such efforts are subject to break down especially at times of heavy volume in the ED. Our improved results were sustained after 18 months of follow-up indicating improved processes at work, though ongoing review of the data by all stakeholders seems essential to maintain improvement.
Our study has limitations related to method and generalizability. We were able to measure each of the basic four processes required for antibiotic administration (Table 2) because of the time stamps available in the electronic medical record. But, in some cases, we could not tell which specific steps in the process that had been delayed. In addition, we were not able to capture data on duration of symptoms prior to first contact with medical staff or from duration of symptoms to presentation in ED. These are potentially as important as any delay encountered once within the health care system. Indeed, in one report of 23 episodes of FN, fevers were present for a mean of 21 h (range 1–72 h) prior to the patient-seeking medical attention [10]. In addition, we did not attempt to analyze adherence to the entire care map or morbidity and mortality results of patients with FN. Rather, we examined only the initial phase of care. As a consequence, the results of our study cannot be used to comment upon the appropriateness of the IDSA guideline to start antibiotics within 2 h of patient presentation [4]. Indeed, retrospective analysis in pursuit of this goal is hazardous because the patient with fewer co-morbidities or less toxic appearance might have received antibiotics in a less urgent fashion, and yet have still have better outcomes. By contrast, Zuckermann et al. described a sequential cohort study in which a critical care pathway reduced all-cause in-hospital mortality for pts with FN, despite only modest adherence to the entire care map [12]. Finally, we did not address differences between day shift and night shift or day of the week. Such differences between clock time and calendar days may just be a surrogate measure for staff: patient ratios. We did learn by review of individual failures that high emergency department volumes result in busy staff who execute the necessary steps less rapidly, regardless of time of day or day of the week.
With regard to generalizability, it should be noted that not all hospitals utilize a comprehensive electronic medical record which affords standardization and reduces delays that can be seen with paper orders. Hospitals without such electronic order systems will need to find different methods of analysis and solutions. Indeed, paper order sets have been found to be effective in reducing treatment time [8, 13]. In addition, our institution did not have physician trainees involved in the care which alter the processes of patient care and can create (or ameliorate) delays depending upon deployment.
FN is a consequence of oncologic treatment that is directed by oncologists. But because most patients will either present to the ED or be directed there, the initial care of FN is not under the direct control of oncologists, the physicians with the most experience in its management. Many of the problems we describe appear to be widespread and the solutions we list are adaptable. But other problems are local in nature, and so too must be the solutions. It therefore behooves oncologists and cancer centers to perform their own analyses of local ED operations with regard to management of FN. Routine and ongoing monitoring of performance is strongly recommended to ensure that the ideal performance becomes the typical performance.
References
Caggiano V, Weiss RV, Rickert TW, Linde-Zwirble WT (2005) Incidence, cost, and mortality of neutropenia hospitalization associated with chemotherapy. Cancer 103:1916–1924
Kuderer NM, Dale DC, Crawford J, Cosler LE, Lyman GH (2006) Mortality, morbidity and cost associated with febrile neutropenia in adult cancer patients. Cancer 106:2258–2266
Talcott JA, Siegel RD, Finberg R, Goldman L (1992) Risk assessment in cancer patients with fever and neutropenia: a prospective, two-center validation of a prediction rule. J Clin Oncol 10:316–322
Freifeld AG, Bow EJ, Sepkowitz KA et al (2011) Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer; 2010 update by the Infectious Disease Society of America. Clin Infect Dis 52(4):e56–e93
Kumar A, Roberts D, Wood KE et al (2006) Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med 34:1589–1596
Klastersky J, Paesmans M, Rubenstein EB et al (2000) The multinational association for supportive care in cancer risk index: a multinational scoring system for indentifying low-risk febrile neutropenic patients. J Clin Oncol 18:3038–3051
Clarke RT, Warnick J, Stretton K, Littlewood TJ (2011) Improving the immediate management of neutropenic sepsis in the UK: lessons form a national audit. Brit J Haematol 153:773–779
Burry E, Punnet A, Mehta A, Thull-Freedman J, Robinson L, Gupta S (2012) Identification of Educational and infrastructural barriers to prompt antibiotic delivery in febrile neutropenia: a quality improvement initiative. Pediatr Blood Cancer 59:431–435
Szwajcer D, Czaykowski P, Turner D (2011) Assessment and management of febrile neutropenia in emergency departments within a regional health authority-a benchmark analysis. Curr Oncol 18:280–284
Nirenberg A, Mulhearn L, Lin S, Larson E (2004) Emergency department waiting times for patients with cancer with febrile neutropenia: a pilot study. Oncol Nurs Forum 31:711–715
Wu AW, Kipshutz AKM, Pronovost PJ (2008) Effectiveness and efficiency of root cause analysis in medicine. JAMA 299:685–687
Zuckermann J, Moreira LB, Stoll P, Moreira LM, Kuchenbecker RS, Polanczyk CA (2008) Compliance with a critical pathway for the management of febrile neutropenia and impact on clinical outcomes. Ann Hematol 87:139–145
Baltic T, Schlosser E, Bedell MK (2002) Neutropenic fever: one institution’s quality improvement project to decease time from patient arrival to initiation of antibiotic therapy. Clin J Oncol Nurs 6:337–340
Acknowledgments
The authors thank Professor Charles Mylander for expert statistical analysis and Jeanne Morris RN for assistance with data acquisition.
Conflict of interest
The authors declare no conflicts of interest. No outside funding was received for this study. The authors retain control of all primary data which is available to review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Meisenberg, B., Clemons, J., Ness, J. et al. Improving hospital performance in the treatment of febrile neutropenia. Support Care Cancer 23, 371–375 (2015). https://doi.org/10.1007/s00520-014-2377-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-014-2377-y