Abstract
Purpose
Satisfaction with care is thought to be important for quality of life (QOL) of family caregivers of patients with recurrent or metastasized digestive cancer requiring palliative care. This study aimed to clarify (1) family caregivers’ QOL status and (2) factors related to their QOL, including satisfaction with care.
Methods
Data were collected from 111 family caregivers of patients with recurrent or metastasized digestive cancer. The Short-Form 36 (SF-36) (acute version) was used to measure QOL.
Results
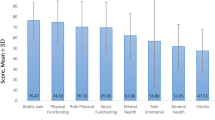
Family caregivers’ QOL was lower than the national average (Cohen’s d = 0.12–0.66). Lower age of patients and family caregivers (standardized regression coefficient (β) = −0.18, β = −0.26) and family caregivers’ perceived health (β = 0.22) were related to better physical health of family caregivers, but satisfaction with care was not related to physical health. However, family caregivers’ mental health was related to their satisfaction with care (Spearman’s rank correlation coefficient (r) = 0.49–0.61, standardized regression coefficient (β) = 0.24–0.42), as well as higher age of family caregivers (β = 0.25), their perceived health (β = 0.30), non-spousal caregiver (β = −0.20), patient lacking a history of surgery aimed at radical treatment (β = −0.22), and patient not hospitalized solely for symptom relief (β = −0.10).
Conclusions
Family caregivers of patients with recurrent or metastasized digestive cancer requiring palliative care had lower QOL, both physically and mentally, than the national average. Improvements in satisfaction with care may contribute to improved QOL.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In 2012, the number of deaths in Japan due to cancer exceeded 360,000, representing approximately 30 % of total deaths [1]. This number is increasing annually as the population ages. In particular, deaths from digestive cancer represent approximately 55 % of total cancer deaths [2]. In terms of curing cancer, the first round of treatment is the most important. When cancer recurs, death often follows within a few years. Therefore, recurrent cancer is recognized as a precursor of death. Furthermore, metastasized cancer is fundamentally incurable [3]. Chemotherapy is not a radical treatment for solid tumors, and chemotherapy for unresectable or recurrent digestive cancer in particular is almost always aimed at life extension and palliative care [4]. Thus, palliative care is important for patients with recurrent or metastasized digestive cancer.
Cancer has a major impact not only on patients but also on family caregivers [5]. In addition to their own lives, family caregivers have long-term responsibilities of providing the patient with physical and mental care as well as coping with associated financial and social problems [6–8]. These and other responsibilities can lead to an increase in chronic sleep disorders [9] and an incidence of depression and mental illness [10–12]. Consequently, family caregivers’ quality of life (QOL), including mental and physical health, often deteriorates [13]. Despite a recent increase in different types of cancer research related to patients’ family caregivers, there is a lack of studies focusing on family caregivers of patients with digestive cancer. Thus, their status remains unclear. Furthermore, in Japan, there are few quantitative studies about family caregivers of cancer patients requiring palliative care. Palliative care aims to improve the QOL of patients facing a life-threatening disease as well as that of the family caregivers enduring it [2]. The importance of continuous support beginning with the early stages of treatment has been recognized as important for family caregivers of cancer patients [14, 15].
In Japan, 90 % of cancer patients die in a general ward [16]. However, patients hospitalized in a general ward have a range of conditions from the acute to terminal stages requiring various forms of care, which may prevent them from receiving adequate and consistent palliative care [15, 17]. Arimori noted the lack of an adequate perception of the need for care for families not directly involved in patient care and stated that family caregivers are left to provide psychological care when the patient is feeling depressed [18]. In terms of QOL, it is important to assess subjective indicators, especially individuals’ satisfaction with care [19–21]. Satisfaction with care is associated with evaluation of care in the medical field [22]. There are ongoing studies regarding patients’ satisfaction with care [23, 24]. However, the relationship between QOL and satisfaction with care among family caregivers of patients with advanced cancer remains unclear, although talking with family caregivers is considered important when evaluating the care of both the family and the patient [25]. Moreover, QOL is related to demographic factors that generally cannot be changed, such as age, sex, familial relationship, and economic status [7, 8, 26–28]. More research is needed regarding whether these factors are also associated with QOL of family caregivers of patients with recurrent or metastasized digestive cancer patients requiring palliative care.
This study aims to clarify (1) family caregivers’ QOL status and (2) factors related to the said QOL, including satisfaction with care.
Methods
Study design and participants
In the present study, “family” is defined as “two or more members who share a bond and emotional intimacy and consider themselves to be family” [29]. A “general ward” is defined as “a medical ward intended for patients who are in various stages of illness, including the acute, chronic, and terminal stages” [30].
A cross-sectional study was conducted from July to November of 2011. Participants were family caregivers of inpatients in a general ward at a university hospital in Tokyo. Patients met the following criteria: (a) diagnosed with digestive cancer, (b) had recurrence or metastasis, (c) older than 20 years, and (d) consented to participate. Eligibility criteria for family caregivers were (a) perceived by the patient to be the primary caregiver (or perceived by the family to be the primary caregiver if poor health of the patient prevented the patient from being asked), (b) older than 20 years, (c) able to fill out the questionnaire and communicate with the researcher, and (d) judged by the head nurse to be physically and mentally capable of participating in the survey. Exclusion criteria for patients were (a) hospitalization for initial cancer surgery and (b) Barthel index score <40 before hospitalization unrelated to cancer. The Barthel index is a standard measure for evaluating activities of daily living (ADL) and has been shown to be reliable and valid. A Barthel index score ≤40 reveals high dependence [31, 32]. We therefore excluded patients with a Barthel index score ≤40 to reduce the effects of care for diseases other than cancer.
Procedure
Patients who were admitted and met the criteria were chosen by the head nurse of the gastroenterology ward. Nurses gave information to admitted patients regarding the objectives of the research. Then the researcher visited patients and family caregivers in the patient’s room and offered a written and verbal explanation of the study. The patient’s written consent was received for both the questionnaire to be distributed to family caregivers and the researcher to be able to view the medical records. Family caregivers were asked to submit the questionnaire either by mail or by placing it in the mailing box in the ward. Patient information was obtained from medical records. For the purposes of this anonymous survey, identical registration numbers were appended so that questionnaires distributed to family caregivers could be consolidated with the notes made by the researcher from medical records. A correspondence table with patient names and numbers was kept for 2 weeks in the ward and then shredded. A coupon book worth 500 yen was given to family caregivers for providing written consent and filling out the questionnaire.
Measurements
Independent variables
Family caregivers’ characteristics measured by the questionnaire included demographic data, perceived health status, chronic disease, familial relationship, whether they lived with the patient before hospitalization, and existence of other caregivers. Economic status was determined by asking, “What do you perceive your economic status to be?” Patients’ characteristics measured included demographic data, physical symptoms, and performance of ADL. Cancer sites, purpose of hospitalization, history of surgery aimed at radical treatment, and performance status (PS) were surveyed from medical records.
Evaluation of care was measured with the care evaluation scale (CES), a well-validated and commonly used instrument in Japan to quantify the family-perceived need for improvements in palliative care [25]. The CES comprises 10 scales, with a six-point Likert-type format from “1: improvement not necessary at all” to “6: improvement highly necessary” regarding physical care provided by the physician, physical care provided by the nurses, psycho-existential care, help with decision-making for the patient, help with decision-making for the family, environment, family burden, costs, availability of facilities, and coordination of care. The reliability and validity of each subscale has been established. In this study, subscale names were not included in the questionnaire. Cronbach’s alphas in this study ranged from 0.84 to 0.95.
Satisfaction with care was measured by 10 subscales of the CES, and one item evaluating degree of total satisfaction with the present treatment patients were receiving because, as stated in the “Introduction”, evaluation of care is related to satisfaction with care [22]. We developed an 11-point Likert scale (0: dissatisfaction–10: satisfaction) for these items. Cronbach’s alpha in this study was 0.97.
Burden of care was measured by the Japanese version of the caregiver reaction assessment (CRA-J) [33, 34]. The CRA contains 24 items divided into five subscales: four subscales regarding burden (disrupted schedule, financial problems, lack of family support, and impact on health) and one subscale regarding positive “self-esteem.” The CRA is a well-validated tool with good psychometric properties and has been validated in other countries. Respondents were asked to rate their care burden on a five-point Likert scale. Cronbach’s alpha in this study ranged from 0.83 to 0.91.
Dependent variables
Family caregivers’ QOL was measured using the Short-Form 36 (SF-36) (acute version), a well-validated, widely used instrument that assesses several aspects of QOL including physical, social, and psychological functioning [35, 36]. It comprises 36 items designed to measure several dimensions of QOL. There is a physical component summary (PCS) score and a mental component summary (MCS) score. Both indexes were used as outcome measures in this study.
Statistical analysis
All analyses were performed using SPSS software, version 12.0J (SPSS, Inc., Chicago, IL), and the level of significance was set at 0.05. Descriptive statistics were calculated for each measure and for family caregivers’ and patients’ characteristics. A national average has not been calculated for QOL measured by the SF-36 (acute version), but the Cohen effect size (d) [37] for comparison against a numerical value calculated in the standard version was calculated as a reference.
The Spearman’s rank correlation coefficient (r) was calculated to examine the relationship between QOL and evaluation of care, satisfaction with care, and burden of care. Because evaluation of care is related to satisfaction with care [22], the Spearman’s coefficient was calculated to investigate the relationship between satisfaction with care and evaluation of care by participants.
Multiple regression analysis was performed. First, the scores for “overall satisfaction with care” and the CRA-J subscales were used as independent variables. Thereafter, additional coefficients were added and selected because previous research suggests that they are important factors related to QOL of family caregivers of cancer patients. The coefficients for family caregivers were age, whether the family caregiver was the spouse, the family caregiver’s perceived health, and existence of other caregivers. The coefficients for patients were age, whether the purpose of admission was palliative care, history of surgery aimed at radical treatment, PS, existence of pain, and whether there was dyspnea. To consider multicollinearity, a variable reduction method was used to build a model for the CRA-J subscales such that the Variance Inflation Factor (VIF) value was at most 2.3 and the other variables were at most 1.4.
To study the impact of satisfaction with care on each of the subscales, “overall satisfaction with care” was switched with other subscales of satisfaction one by one within the constructed model, and for each case, the respective standardized partial regression coefficient (β) and the coefficient of determination (R 2) were calculated.
Ethical considerations
This study was approved by the institutional review board of The University of Tokyo. Requests for participation in the study included verbal and written explanations of the purpose of the study, the voluntary nature of participation, the protection of personal information, and the fact that for up to 2 weeks consent could be withdrawn, until the point when the correspondence table was destroyed. Furthermore, the opening of questionnaires was planned for at least 2 weeks after the correspondence table was shredded, to preserve the anonymity of the patients surveyed.
Results
Compliance status
A total of 198 patients who met the criteria were initially selected on the basis of their medical records. Thirty-eight patients declined to participate. Thus, 160 patients were enrolled, and all gave written consent. Of the 160 consenting patients, we were unable to meet with the families of seven. Ultimately, 153 family caregivers received the questionnaire. Responses were obtained from 129 of the families (84 %). Questionnaires of 18 family caregivers were excluded for either failing to meet the criteria or having less than an 80 % response rate for the overall questionnaire. Thus, we analyzed data from 111 family caregivers.
Family caregivers’ and patients’ characteristics
The mean age of family caregivers was 59.3 ± 12.3 years (range, 29–87 years); 84 (75.7 %) were women. The mean age of patients was 71.3 ± 10.3 years, and 31 (27.9 %) were women. At least 90 patients (81 %) were classified as “unassisted” for all ADL items (Tables 1 and 2).
Ninety-five participants (85.6 %) responded to “changes in health” by reporting no change from the week before on the SF-36 (acute version). Therefore, participants’ QOL was compared with the national average for the standard version of the SF-36. All aspects of QOL were lower than the national average. The effect size of the bodily pain subscale relative to the national average was negligible, at 0.12. The effect size for other items, including the summary score, was small to moderate (Table 2).
Relationship of QOL to evaluation of care, satisfaction with care, and burden of care
Moderate correlations existed for all items regarding the relationship between evaluation of care and the MCS score. This was also true for the relationship between satisfaction with care and the MCS score (Table 3). There was a moderate negative correlation between burden of care and the MCS score for “impact on daily life,” “support from family,” and “impact on health.” The PCS score was not significantly correlated with any item relating to evaluation of care, satisfaction with care, or burden of care.
Relationship between evaluation of care and satisfaction with care
There was a significant correlation between all items (Table 4). We found that evaluation of care and satisfaction with care had a correlation of 0.6 or higher for three items: “help with decision-making for patient,” “help with decision-making for family,” and “psycho-existential care.” Satisfaction with “physical care provided by the physician,” “physical care provided by the nurses,” and “family burden” were highly correlated with “overall satisfaction with care” (0.74–0.82). However, the correlation between care evaluation and satisfaction with care was only 0.3 to 0.4. The lowest correlation was 0.38 for “family burden.” Satisfaction with “family burden” had the strongest correlation with “psycho-existential care” among the items evaluated (0.62; CES). It also had a strong correlation with all satisfaction items.
Relationship with QOL
Results of multiple regression analysis revealed that the PCS score was higher (adjusted R 2 = 0.140) when the family caregivers’ age was lower (β = −0.18), when they perceived their own health as good (β = 0.22), and when the patient’s age was lower (β = −0.26) (Table 5). Furthermore, the MCS score was higher (adjusted R 2 = 0.620) when family caregivers’ age was higher (β = 0.25) and they perceived their own health as good (β = 0.30). This was also true when the family caregiver was not the spouse (β = −0.20), when the patient did not undergo surgery aimed at radical treatment (β = −0.22), and when the purpose of hospitalization was not only relief of symptoms (β = −0.10).
Table 6 shows that when each satisfaction subscale was subjected to multiple regression analysis, the model in which the MCS score was a dependent variable was good (β = 0.24–0.42; adjusted R 2 = 0.526–0.620). In particular, satisfaction with support from physician and nurses had a stronger influence on MCS score than satisfaction with any of the other items. Furthermore, these models indicated that the satisfaction item “help with decision-making for patients” had a larger impact on the MCS score than the “help with decision-making for family” item. In addition, “family burden” and “psycho-existential care” satisfaction had the same degree of influence on MCS score.
Discussion
The present study investigated QOL status and the related factors to QOL including satisfaction with care for family caregivers of patients with recurrent or metastasized digestive cancer patients requiring palliative care in a general ward. The difficulty of recruiting families of patients with advanced-stage cancer means that little qualitative or quantitative research on family caregivers following patient death has been conducted in Japan. This is the first quantitative study investigating QOL of family caregivers of digestive cancer patients requiring palliative care in Japan.
In the present study, participants had lower QOL than the general population. This was also true in a South Korean study of the QOL of family caregivers of terminal cancer patients [38]. Our results suggest that family caregivers of patients hospitalized in a general ward have a greater need for both physical and mental support than does the general population from the initial treatment stage on and not only from terminal stage. The nationwide sample used to determine the national average consisted of data from 2,279 people with a mean age of 50.5 years and can be considered to represent standard scores and distributions of Japanese people 20 to 79 years of age [36]. The marital status of the sample, however, varied, and perceptions of health and economic status were not considered. Although the 59.3-year mean age of study participants was similar to the age of the nationwide sample, we have left consideration of other factors, such as perceptions of health and economic status, for future study.
The present study suggests that evaluation of care had an impact on the MCS score. However, it also shows that satisfaction with care was a more important indicator for the MCS score. The implication is that improving satisfaction with care may improve the mental health aspect of QOL for family caregivers of patients with advanced cancer requiring palliative care.
It is possible that satisfaction with “physical care provided by the physician,” “physical care provided by the nurses,” and “family burden” may be related to support issues other than those measured by the CES.
Satisfaction with “family burden” was correlated with all satisfaction with care for patient’s items and evaluation of patient’s items. In addition, psycho-existential care and help with decision-making for patients were correlated with the MCS score. Previous research has demonstrated that family caregivers want the patient’s suffering to be alleviated [39]. They derive relief from knowing that the patient can live comfortably independently and feeling that they are useful to the patient [18, 39]. Such patient care is thought to indirectly meet the wishes of and provide relief for family caregivers, and our study showed that family caregivers satisfied with patient care are also highly satisfied with their own care. Obtaining quality care for the patient is thus an important way to improve family caregiver satisfaction. Our study quantitatively showed that help with decision-making for patients and psychological care that doctors provide to patients that family caregivers are satisfied with and evaluate well contribute to satisfaction with the level of the family burden and are also relevant to MCS scores. The items in the “help with decision-making for patients” subscale in the CES involve the patient’s condition, current treatment, and outlook. Future research must therefore consider how patients are informed about their condition, outlook, current treatment program, and psychological status.
This research clarified that a connection has been found between family caregivers’ satisfaction with care and QOL-related mental health. Geline and Iconomou et al. showed that communication with patients, caregivers, and healthcare providers was important in promoting family caregivers’ QOL [40, 41]. A general ward is characterized by the ability to provide continuous medical care from diagnosis to caregiving and by the continuity of involvement on the part of the primary care physician and nurses [15]. Optimizing these strengths could increase satisfaction with “physical care provided by the physician” and “physical care provided by the nurses” and lead to an improvement in MCS score. However, the question of what family caregivers need from doctors and nurses is a topic for future study.
In this study, family caregivers’ age and perceived health were associated with both the PCS and MCS scores, supporting previous findings [26, 27, 42, 43]. Participants in this study whose age was equal to or below the mean age were divided into adulthood or middle age. Younger partners may have to care for the patient while dealing with the demands of employment and childcare [26]. Consistent with findings from Kim et al., this result may suggest that the more social roles and responsibilities a caregiver has, the more likely the caregiver will experience stress and negative adjustment [44]. Thus, taking into account the ages of a patient’s family caregivers and recognizing the impact of the patient’s hospitalization on family caregivers may contribute to increased mental health.
In our study, the PCS score showed a small to moderate effect when compared with the national average. In the future, physical support methods must be established. However, we found no relationship between the PCS and family burden of care and satisfaction with care. Thus, future studies might investigate a method for support that differentiates between burden of care and satisfaction with care.
For familial factors, a high MCS score was associated with not being the spouse, as well as age and perceived health, which supports previous research [28]. Regarding patient factors, hospitalization aimed not solely at palliative care and without surgery to provide radical treatment was associated with a high MCS score. When hospitalization becomes solely about palliative care, the patient’s impending death, heretofore ignored because of treatment, must be recognized as a reality. This gives rise to thoughts of death and elicits an anticipatory grief reaction [45]. In addition, patients suffering from various painful symptoms may cause family caregivers to feel helpless or inadequate, so oncology nurses should educate family caregivers and manage their symptoms [40]. It is also important to rapidly alleviate the patient’s pain and to respect the role of family caregivers as patient caregivers [45].
To our knowledge, this is the first report showing that family caregivers of patients who had undergone surgery aimed at radical treatment had a relatively lower MCS score. Recurrence is symbolic, for both the cancer patient and family caregivers. It means that the battle has recommenced and will continue, and this is a source of new suffering [46]. For patients who undergo major invasive surgery believing in a cure, cancer recurrence or metastasis despite this is a shock to patients and family caregivers. As a consequence, the mental QOL presumably decreases.
This study has several limitations. First, because of sample bias, caution should be exercised when generalizing the results. The participating institution was a facility in a university hospital in Tokyo. The average length of stay in the participating ward was 10.1 days, in line with other research showing that 67.6 % of patients who are discharged from a general ward have a length of stay between 0 and 14 days [47]. However, family caregivers we were unable to meet with were not surveyed. A method of measuring QOL of family caregivers who are unable to come to the hospital is needed in future studies. Second, because many of the patients in the present study were in the hospital for therapeutic purposes, they were at similar PS and ADL levels. Future investigations should include patients with a PS > 2 and worse ADL scores.
Family caregivers of patients with recurrent or metastasized digestive cancer requiring palliative care in a general ward had lower QOL, both physically and mentally, than the national average. This suggests that this group requires support. QOL items associated with mental health and satisfaction with care were related, and satisfaction with “family burden” was related to patient care items. It is important to focus on improving both patients and family caregivers’ satisfaction with care. Future research must determine, through interviews, what type of care provides satisfaction to family caregivers of patients with recurrent or metastasized digestive cancer requiring palliative care in a general ward and use the information obtained to identify beneficial interventions. The primary caregivers in our study were selected based on patient perceptions, but patient perceptions of who the primary caregiver was may have differed from family perceptions. A study of family caregivers as perceived by the family should thus also be conducted. The present study considered digestive cancer, which features digestive manifestations also seen in other types of cancer. The results may therefore be applicable to other cancer types.
References
Ministry of Health, Labour and Welfare (2012) Annual estimation of demographic statistics 2012 in Japan. The number of deaths; annual change in number of deaths according to cause of death. http://www.mhlw.go.jp/toukei/saikin/hw/jinkou/geppo/nengai12/dl/h6.pdf. Accessed 5 November 2013
Center for Cancer Control and Information Services, National Cancer Center, Japan (2011) Convalescence of cancer and palliative care, palliative care in cancer medicine. http://ganjoho.jp/public/support/relaxation/palliative_care.html. Accessed 5 November 2013
Nakagawa K (2006) A textbook of cancer. Sanseido, Tokyo
Furuse J (2011) A handbook of chemotherapy of digestive system cancer. Chugai-igakusha, Tokyo
Stenberg U, Ruland CM, Miaskowski C (2010) Review of the literature on the effects of caring for a patient with cancer. Psychooncology 19(10):1013–1025
Bowman KF, Rose JH, Deimling GT (2006) Appraisal of the cancer experience by family members and survivors in long-term survivorship. Psychooncology 15(9):834–845
Yun YH, Rhee YS, Kang IO et al (2005) Economic burdens and quality of life of family caregivers of cancer patients. Oncology 68(2–3):107–114
Baider L, De-Nour AK (1993) Impact of cancer on couples. Cancer Invest 11(6):706–713
Carter PA (2002) Caregivers’ descriptions of sleep changes and depressive symptoms. Oncol Nurs Forum 29(9):1277–1283
Rhee YS, Yun YH, Park S et al (2008) Depression in family caregivers of cancer patients: the feeling of burden as a predictor of depression. J Clin Oncol 26(36):5890–5895
Kaye JM, Gracely EJ (1993) Psychological distress in cancer patients and their spouses. J Cancer Educ 8(1):47–52
Vanderwerker LC, Laff RE, Kadan-Lottick NS et al (2005) Psychiatric disorders and mental health service use among caregivers of advanced cancer patients. J Clin Oncol 23(28):6899–6907
Hodgkinson K, Butow P, Hunt GE et al (2007) Life after cancer: couples’ and partners’ psychological adjustment and supportive care needs. Support Care Cancer 15(4):405–415
Pellegrino R, Formica V, Portarena I et al (2010) Caregiver distress in the early phases of cancer. Anticancer Res 30(11):4657–4664
Ogasawara T (2008) Family care of palliative care. Fam Nurs 6(2):47–52
NPO. Hospice Palliative Care Japan (2010) About hospice palliative care from now on. Present condition and issues. http://www.mhlw.go.jp/shingi/2006/12/dl/s1220-10a16a.pdf. Accessed 5 November 2013
Chou S, Kawamoto R, Nakano M (2009) The development of a method to evaluate general ward nursing care practices targeted at families of cancer patients—identification and selection of items for evaluation. J UOEH 31(1):37–49
Arimori Y (2007) Family care in hospitals: the point of view of a nurse in a general ward. Jpn J Hosp Palliat Care 17:S118–S120
Tazaki M, Nakane Y (2004) Quality of life instrument. Jpn J Clin Psychiatry 33:S83–S87
Oleson M (1990) Subjectively perceived quality of life. Image J Nurs Sch 22(3):187–190
Lohr KN (1988) Outcome measurement: concepts and questions. Inquiry 25(1):37–50
Matsunaga Y (2006) Concept analysis of patient satisfaction. Bull Sch Nurs Fac Med Toho Univ 19:13–24
Gupta D, Lis CG, Grutch JF (2007) Perceived cancer-related financial difficulty: implications for patient satisfaction with quality of life in advance cancer. Support Care Cancer 15:1051–1056
Lis CG, Gupta D, Granick J, Grutch JF (2006) Can patient satisfaction with quality of life predict survival in advanced colorectal cancer? Support Care Cancer 14:1104–1110
Morita T, Hirai K, Sakaguchi Y et al (2004) Measuring the quality of structure and process in end-of-life care from the bereaved family perspective. J Pain Symptom Manag 27(6):492–501
Song L, Northouse LL, Braun TM et al (2011) Assessing longitudinal quality of life in prostate cancer patients and their spouses: a multilevel modeling approach. Qual Life Res 20(3):371–381
Awadalla AW, Ohaeri JU, Gholoum A et al (2007) Factors associated with quality of life of outpatients with breast cancer and gynecologic cancers and their family caregivers: a controlled study. BMC Cancer 7:102–115
Sarna L, Cooley ME, Brown JK et al (2006) Quality of life and health status of dyads of women with lung cancer and family members. Oncol Nurs Forum 33(6):1109–1116
Friedman MM (1992) Family nursing: research, theory & practice, 3rd edn. Appleton & Lange, Stamford
Ogawa M (2006) Palliative care manual for a general ward. Health Shuppan, Tokyo
Collin C, Wade DT, Davies S, Horne V (1988) The Barthel ADL index: a reliability study. Int Disabil Stud 10(2):61–63
Granger CV, Dewis LS, Peters NC et al (1979) Stroke rehabilitation: analysis of repeated Barthel index measures. Arch Phys Med Rehabil 60(1):14–17
Given CW, Given B, Stommel M et al (1992) The caregiver reaction assessment (CRA) for caregivers to persons with chronic physical and mental impairments. Res Nurs Health 15(4):271–283
Misawa T, Miyashita M, Kawa M et al (2009) Validity and reliability of the Japanese version of the caregiver reaction assessment scale (CRA-J) for community-dwelling cancer patients. Am J Hosp Palliat Care 26(5):334–340
Fukuhara S, Ware JE Jr, Kosinski M et al (1998) Psychometric and clinical tests of validity of the Japanese SF-36 Health Survey. J Clin Epidemiol 51:1045–1053
Fukuhara S, Suzukamo Y (2004) Manual of SF-36v2 Japanese version: Institute for Health Outcomes & Process Evaluation research. i Hope International, Kyoto
Cohen J (2009) Statistical power analysis for the behavioral sciences. Psychology Press, New York
Song JI, Shin DW, Choi JY et al (2011) Quality of life and mental health in family caregivers of patients with terminal cancer. Support Care Cancer 19(10):1519–1526
Kirigaya M, Takano M, Hirata Y et al (2005) Nursing to families of dying patients in a general ward: information from interviews with bereaved families. Seijin-kango 36:27–29
Tamayo GJ, Broxson A, Munsll M, Cohen MZ (2010) Caring for the caregiver. Oncol Nurs Forum 37(1):E50–E57
Iconomou G, Vagenakis AG, Kalofonos HP (2001) The informational needs satisfaction with communication, and psychological status of primary caregivers of cancer patients receiving chemotherapy. Support Care Cancer 9:591–596
Lu L, Pan B, Sun W et al (2010) Quality of life and related factors among cancer caregivers in China. Psychiatry Clin Neurosci 64(5):505–513
Tang WR (2009) Hospice family caregivers’ quality of life. J Clin Nurs 18(18):2563–2572
Kim Y, Baker F, Spillers RL et al (2006) Psychological adjustment of cancer caregivers with multiple roles. Psychooncology 15:795–804
Kurihara Y (2007) Family care when the patient’s treatment translates into palliative care (gear change). Jpn J Hosp Palliat Care 17:S95–S99
Vivar CG, Whyte DA, McQueen A (2010) ‘Again’: the impact of recurrence on survivors of cancer and family members. J Clin Nurs 19(13–14):2048–2056
Ministry of Health, Labour and Welfare (2011) Mean hospitalization of discharged patients from 2011 patient survey in Japan. http://www.mhlw.go.jp/toukei/saikin/hw/kanja/11/dl/03.pdf. Accessed 5 November 2013
Acknowledgments
This study was supported by a grant from the Mental Health Okamoto Memorial Foundation. We are sincerely grateful to participants and staff in the hospitals for cooperating with this study.
Conflict of interest
All authors have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Morishita, M., Kamibeppu, K. Quality of life and satisfaction with care among family caregivers of patients with recurrent or metastasized digestive cancer requiring palliative care. Support Care Cancer 22, 2687–2696 (2014). https://doi.org/10.1007/s00520-014-2259-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-014-2259-3