Abstract
Purpose
This study investigated the efficacy and safety of cryotherapy, in the form of frozen gel gloves, in relation to docetaxel-induced hand and fingernail toxicities.
Patients and methods
After piloting with 21 patients, a consecutive series sample of patients (n = 53) prescribed docetaxel every 3 weeks, for a minimum of three cycles, was enrolled in this randomised control trial. Participants acted as their own control, with the frozen gel glove worn on one randomised hand for 15 min prior to infusion, for the duration of the infusion, and for 15 min of after completion of treatment. Hand and nail toxicities were evaluated by two blinded assessors according to CTCAE.v4 criteria. To assess the potential for cross-infection of multi-use gloves, microbial culture and sensitivity swabs were taken of each glove at every tenth use.
Results
Of the 53 participants enrolled in the main study, 21 provided evaluable data. There was a 60 % withdrawal rate due to patient discomfort with the intervention. The mean incidence and severity of toxicities in all evaluable cycles in control and intervention hands respectively were erythroderma grade 1 (5/5 %), nail discolouration grade 1 (81/67 %), nail loss grade 1 (19/19 %) and nail ridging grade 1 (57/57 %). No significant differences were determined between hand conditions in terms of time to event, nor in terms of toxicity in gloved and non-gloved hands.
Conclusion
While cryotherapy in the form of frozen gloves for the cutaneous toxicities associated with docetaxel is safe, its limited efficacy, patient discomfort and some logistical issues preclude its use in our clinical setting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Docetaxel is considered one of the most effective agents in the treatment of malignant tumours of the lung, breast, ovary, head and neck, stomach and prostate [1, 2]. In common with many chemotherapy regimens, a wide profile of short- and long-term side effects (or ‘toxicities’) is associated with docetaxel. These toxicities range from life-threatening to those that cause cosmetic changes such as hair loss. Some toxicities of docetaxel, such as myelosuppression and hypersensitivity reactions, are well-managed with supportive therapies. Others, such as cutaneous reactions of the hands and nails, are relatively neglected in the research literature and in clinical practice, despite their recognised potential to impair cancer patients' quality of life and functional status [3, 4]. Between 30 and 88 % [4–8] of patients receiving docetaxel experience cutaneous side effects of the hand ranging from skin and nail disfigurement, blistering, desquamation, pain, infection and impaired treatment-related quality of life and function.
The aetiology of docetaxel-induced cutaneous hand and nail toxicities is uncertain. The hypothesis supported by early evidence indicates that soft tissue perfusion of intravenously circulating docetaxel instigates the side effects, exerting anti-angiogenic effects on the capillaries of the hand and digits, and thence the structures of the skin and nail beds [7–10]. Alternatively, it is proposed that docetaxel toxicities are the result of a neurogenically mediated inflammatory process within these structures [7, 11]. There is also anecdotal evidence suggesting these effects result from the reaction of ultraviolet light with circulating drug in the peripheries [7], although the exact mechanism has not been articulated.
One approach that has had some success in preventing selected complications of chemotherapy such as oral mucositis [12] and alopecia [13–16] is cryotherapy. It is argued that cryotherapy temporarily reduces vascular flow to the target areas, hence reducing their exposure to the harmful agent that causes the toxicities. One n = 45 case-control study [8] based on this hypothesis provided some interesting early data in relation to hand and nail toxicities. Using cryotherapy in the form of frozen gel gloves during infusion, Scotte et al. noted a decrease in the overall incidence of fingernail toxicities from 51 % in the control hand to 11 % in the hand receiving cryotherapy [8]. Additionally, the severity of fingernail toxicities was reduced from 22 % onycholysis in untreated nails to 0 % in nails treated with frozen gloves (p = 0.0001) [8]. Skin toxicity was noted in 24 % of protected hands versus 53 % in unprotected hands [8]. Patients were described as satisfied with the comfort level of the frozen glove intervention in this study. An n = 52 study that replicated Scotte et al.'s approach, and which similarly reported no patient discomfort with the intervention, found that nail and skin toxicity was “significantly decreased” in the protected left hand (p = 0.01) [17]. A larger n = 122 case-control investigation also reported that onycholysis and skin toxicites were significantly lower in hands protected with frozen gloves (p = 0.0001) [18].
However, these studies have several limitations. They appear to have consistently used the left hand as the intervention and the right hand as the case-control; in a context where it can be reasonably argued that right-hand dominance could be a confounding variable. In addition, the assessors do not appear to have been blinded. A more robust design to test the intervention would therefore randomise the hands and blind the assessors. There are also safety and logistical considerations that have not been addressed in the literature. Due to financial, space and other resource implications, in most chemotherapy units, the glove must be reusable, yet issues related to cross-infection between multiple users of the gloves have not been investigated. Chemotherapy patients may be colonised with, or exposed to, clinically significant organisms and many patients treated with docetaxel are immunocompromised [11]. Hence, nosocomial transmission of organisms between the gloves and the multiple, vulnerable users of the gloves might occur in the absence of infection control protocols.
In summary, cryotherapy for docetaxel-induced nail and skin toxicities of the hand is a popular and promising preventative treatment. Yet there is little high level research evidence to support its use and there are some concerns regarding its clinical safety. While frozen glove therapy has the potential to reduce the cutaneous effects of docetaxel treatment, further research incorporating considerations of infection control, blinding of assessors, randomisation and sample size is required to justify the implementation of this intervention. The randomised control study described in this paper aimed to extend previous work to enhance methodological rigour and add new evidence with respect to infection control, prior to its possible implementation in a large ambulatory cancer setting.
Objective
This study investigated the efficacy and safety of cryotherapy, in the form of frozen gel gloves, with respect to the prevention of docetaxel-induced nail and skin toxicities in cancer patients.
Methods
Study design
The study was a single-blinded, randomised control study of taxane-naїve patients prescribed docetaxel for breast, prostate, lung, head and neck, stomach or ovarian cancer. Participant recruitment and data collection occurred between December 2010 and December 2012, after ethical approval was obtained from the Princess Alexandra Hospital, Queensland University of Technology and Griffith University Human Research Ethics Committees. The study was registered as an investigator-initiated clinical device trial with the Therapeutic Goods Administration of Australia (CTN 131/2009) and with ClinicalTrials.gov (NCT 00911352).
Research questions
-
1.
Does cryotherapy reduce the incidence, severity and time-to-onset of docetaxel-induced nail and skin toxicities?
-
2.
Do patients tolerate cryotherapy to prevent docetaxel-induced nail and skin toxicities?
-
3.
What is the microbiological profile of frozen gel gloves used to prevent docetaxel-induced nail and skin toxicities?
-
4.
What effect does the use of a cotton glove as a barrier between the patient's skin and the surface of the frozen glove have on the microbiological carriage of frozen gel gloves used to prevent docetaxel-induced nail and skin toxicities?
Setting, participants and recruitment
Princess Alexandra Hospital is a large, public metropolitan teaching hospital in southeast Queensland, Australia. Between 1,800 and 2,000 individual patients are treated with chemotherapy each year in the service. A prospective, consecutive sample of patients was recruited according to the following inclusion criteria:
-
1.
Prescribed docetaxel as single or multimodal treatment for any cancer diagnosis, for a minimum of three cycles
-
2.
No disorders of the nails or skin of the hand at the start of treatment
-
3.
Able to provide informed consent.
Exclusion criteria:
-
1.
Previous treatment with taxane chemotherapy
-
2.
Medical history of Raynaud's phenomenon, distal metastases, ungual pathology, arteriopathy, cold intolerance, peripheral neuropathy of CTCAE grade 2 or higher
-
3.
Not fit for participation in the opinion of the treating oncologist.
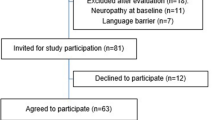
Patients were identified by their oncologist or cancer care coordinator and referred to the project officer, who screened for eligibility, obtained written informed consent and randomised the patients' left or right hand to the frozen glove intervention or control.
Randomisation
Envelopes labelled with numbers 1–80 were created, along with a corresponding number of cards; half marked ‘right’ and half marked ‘left’. These cards were shuffled by a QUT researcher, external to the study, in groups of ten, and placed within the envelopes (thereby the first ten included five left and five right-labelled cards, as did the next ten, and the next). As each participant was recruited into the study, the next envelope was taken from the pile and opened. The hand on this card was the hand that would be gloved in the study.
Cryotherapy intervention
The control treatment comprised usual care, that is, no cryotherapy intervention. The cryotherapy intervention consisted of a frozen glycerine gel-filled glove, covered with a permeable fabric. The gloves covered the hand to the wrist, separating the thumb from the rest of the hand like a mitten. Consistent with the recommendations of the product manufacturer, the gel glove was frozen at −25 to −30 °C for at least 12 h prior to use. Freezer temperature was checked and recorded weekly to ensure standardisation of glove temperature.
At the time of study commencement, patients usually received docetaxel once every 21 days for 63–189 days (i.e. on 3 to 11 separate occasions each). Docetaxel was administered on day 1 of each cycle. Hence, cryotherapy was administered on day 1 of each cycle and occurred every 21 days thereafter, concurrent with docetaxel administration. During each docetaxel infusion, the patient wore the glove for a total of 90 min (15 min before treatment, during the 1 h docetaxel infusion, and for a further 15 min after infusion). Because of the duration of the infusion, more than one frozen gel glove was used to maintain the necessary low temperature of the hand and nails. Gloves were therefore changed every 45 min, but were checked every 20 min and were changed more regularly if they did not feel cool to the touch. This procedure aimed to ensure the patient's periphery was vasoconstricted on commencement of the infusion and for enough time afterwards to ensure the circulating drug did not reach the target area [11].
Infection control intervention
In most facilities, the frozen gloves are routinely re-used by patients, and recirculated amongst them, although the manufacturer recommends that the gloves are not cleaned by wetting the permeable covering. Hence, the gloves cannot be cleaned between patients in accordance with the Spaulding Classification System [19]. To counter the risk of infection this entails, a disposable cotton glove is worn underneath the gel glove. As the disposable cotton glove usually reaches only to the wrist, this nonetheless exposes the area of patient skin above the wrist to the permeable covering, as the gel glove is longer than most disposable cotton gloves.
In this study, to offset the potential infection control risk of this standard practice, a modification to the gloving procedure was tested. This comprised the insertion of a disposable nitrile glove, between the cotton and gel gloves, which exceeded the length of both these gloves. Intervention hands were therefore assigned either a double (disposable cotton plus gel) or triple (disposable cotton plus disposable nitrile plus gel) glove set. The assignment of the glove set depended on the patient's baseline microbiological culture and sensitivity (MC&S) swabs of epidemiologically-significant microorganisms, including multidrug-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Entercoccus (VRE) and carbapenem-resistant Acinetobacter baumannii (CRAB). Triple-gloved patients were assigned into Intervention Arm 2 (multi-disease resistant organism [MDRO] negative) or Intervention Arm 3 (MDRO positive) prior to random assignment of their hands into intervention or control groups (see Fig. 1).
Outcome variables
The primary endpoints were a decrease, over the course of treatment, of nail and skin toxicities of the gloved hand in terms of:
-
1.
Incidence
-
2.
Severity as measured by Common Toxicity Criteria for Adverse Events-Version 4 (CTCAE.v4) scores.
Secondary endpoints included:
-
1.
Delayed time to occurrence of any nail or skin toxicity
-
2.
Patient tolerance of cryotherapy
-
3.
Decrease in microbial type and load of the frozen gloves, including the absence of epidemiologically significant organisms.
Measures
Chart data, including demographics (age, gender), tumour type and stage, and concomitant medications were recorded on the Client Record Form. Disease- and treatment-related data were updated at each time point.
Digital photographs of each patient's intervention and control hands were taken under standardised lighting conditions by a medically trained photographer at baseline and on day 1 of each cycle thereafter. Because the final infusion can also affect the nails beyond treatment cessation, nail assessments were also undertaken 3 weeks after the last infusion during routine follow-up. Hand and nail toxicities were assessed for each patient at every cycle from the digital photographs by two blinded assessors using the Common Toxicity Criteria for Adverse Events Version 4.+0 [20], which are the standard criteria in cancer clinical trials (refer Table 1). Inter-rater reliability ratings were established between assessors at baseline (96.55 % agreement between the two assessors) and re-evaluated 6-monthly thereafter.
Patients' satisfaction with cryotherapy was also assessed during each of the infusions, using a 4-point rating system to determine whether patients were dissatisfied (0), not very satisfied (1), satisfied (2) or very satisfied (3) with the treatment in terms of glove contact, temperature tolerance and immobilisation constraints.
Sites for swabbing of all gloves were standardised to (1) the internal glove surface of the back of the hand, (2) the internal glove surface of the palm of the hand, (3) the internal glove surface at the tip of the second index finger and (4) the internal glove surface at tip of the thumb. These sites are well-established as problematic for cleaning and decontamination in hand hygiene, where carriage of microbial organisms is high [19]. Swabbing of the microbial load of the frozen gel glove occurred on every tenth intervention glove at predetermined time-points, as outlined in Fig. 1.
Bias
As commonly encountered in clinical device trials, it was impossible to blind participants or project officers to such an obvious intervention, which is a potential source of bias. To address this, the toxicities were not graded in the presence of the patient. Photographs of the hands were assessed by two blinded assessors who had no contact with the patient at any stage.
Study size
Using Cohen's method for estimating required sample size, we set the estimated effect size at medium (0.30) and the power required at 0.80, with a significance level of 0.05 [21]. According to Cohen's Indices, n = 87 were required to power the study.
Statistical methods
Statistical analyses of the pooled data were conducted by qualified members of the research team using SPSS version 21.0. Frequencies and summary descriptive statistics were determined for all study variables. Continuous outcome variables are reported as means and standard deviations for normally distributed data; otherwise, the median and inter-quartile range is presented. Proportions are used to summarise categorical variables.
The data for participants who withdrew from the study due to discomfort or logistical issues, but who had been assessed at four or more data collection points, were included in the final analysis. Analyses were not undertaken on an intention-to-treat basis, as a number of participants withdrew from the study after only one data collection point, leaving little opportunity for any toxicities to have occurred. Frozen glove contamination was analysed by determining frequencies and types of micro-organisms.
Kaplan-Meier survival analyses were undertaken of data from participants who had undertaken four or more assessments to determine differences in time-to-event (an event being a score of 1 to 5 toxicity grading for erythroderma) between control and gloved hands. This analysis is a robust way of measuring, from a pre-defined point, the time taken to experience a specified event [22]. The Wilcoxon matched-pairs analysis was used for non-parametric data. Chi square and McNemar Chi square tested categorical and binary variables. Differences between hands were investigated at the fourth assessment, as this is the time that the majority of patients participated in.
Data Management
The study was regularly monitored by an independent clinical trial auditing organisation to ensure compliance with all standard operating procedures, including data management and statistical analysis procedures. It was also subject to periodic intensive audit by this organisation, as well as a close out audit, in compliance with standard good clinical practice procedures. The trial was deemed compliant at all times.
Results
Pilot study
The pilot study tested the feasibility of implementing the intervention and the microbial testing protocol. Twenty-one participants were recruited into the pilot; however, only 15 of these proceeded with the frozen glove. The remaining six either withdrew before treatment commenced, or were unable to participate due to an altered treatment regimen or logistical issues. Those who commenced frozen glove treatment comprised 13 women and two men, with a mean age of 54.8 years. Of note, the pilot study adhered to the manufacturer's guidelines, that is, the gloves were frozen to −25 °C prior to use. Only seven pilot study patients completed three or more cycles for evaluation. The remaining six patients withdrew before cycle 3, citing dissatisfaction with the glove temperature.
Main study
The second phase of the study accounted for the high attrition in the pilot study due to patients' discomfort with the glove temperature and to align the intervention with usual clinical, rather than recommended research, practice. Standard clinical practice is to freeze the gloves in a domestic freezer with a temperature of approximately −4 °C. A recent study found that 100 % of participants similarly complained of discomfort at least once when using gloves frozen to −25 °C or lower [23]; however, less toxicity and less discomfort were observed when Ishiguro et al. increased the temperature by up to 15°. Hence, in the main study, ethical approval was obtained to amend the protocol to freezing of the gel glove for at least 12 h at −4 to −10 °C prior to use. Figure 2 outlines participant flow in the study.
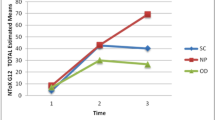
Twenty-one of the 53 participants enrolled in the main study completed evaluable data (i.e. four or more assessments); the remaining 32 withdrew due to dissatisfaction with the glove temperature or immobility constraints. Their demographics and medical variables are presented in Table 2. The mean incidence and mean severity of toxicities are presented in Table 3.
Kaplan-Meier analysis demonstrated no significant difference between hand conditions in terms of time to event. At assessment 4, no participant demonstrated any significant difference in toxicity between gloved and non-gloved hands. Time to onset is presented in Table 4.
All swabs taken throughout the project returned negative results for MRSA, VRE and CRAB.
Discussion
This study investigated the safety and the efficacy of frozen glove therapy for hand and nail toxicities arising from docetaxel therapy. In terms of safety, the double and triple glove techniques trialled here are acceptable. There was no carriage of microbial organisms on the surface on any of the gel gloves at any time point. In terms of efficacy, however, cryotherapy did not appear to reduce the incidence, severity and time-to-onset of docetaxel-induced cutaneous toxicities in this sample. These results are mirrored by another recent study, which investigated predictors and efficacy of frozen glove therapy for taxane-induced hand and nail toxicities in 55 intervention patients and 146 controls [24]. Can et al. reported a comparable demographic to the present study, in that the majority were females with a mean age of 53 years and a diagnosis of breast cancer [24]. Can et al. similarly reported no statistically significant difference for nail toxicity between intervention and control groups [24].
While recognizing that the results of our study do not align with the findings of studies that report benefit from cryotherapy intervention for cutaneous toxicities [8, 11, 17, 18, 23], we have determined that this intervention is of limited value in our clinical context. The reasons are several. As indicated by the high withdrawal rate, individual patients did not tolerate the frozen glove particularly well. Moreover, in the open plan design of our chemotherapy clinic, where patients are closely spaced and can see and interact with each other freely, an obvious intervention like the frozen glove draws a great deal of interest. Study participants tended to collectively discuss their negative experience of the glove with other potential participants. Hence, while the withdrawal rate of 66 % in the pilot study lessened somewhat to 60 % in the main study after adjusting the temperature of the glove, the overall effect of patient interaction in this study, which would probably be replicated in the clinical context if the intervention were formally introduced, was that many patients chose not to be involved or withdrew after discussing the intervention with other patients.
In addition, the majority of nail changes we detected were cosmetic and not likely to interfere with patients' quality of life. Qualitative comments from the patients indicated that the discomfort caused by the glove, and the lack of clinical efficacy they observed themselves, did not offset any potential benefits from the intervention. Furthermore, the logistics of administering the cryotherapy in our high-volume, resource-stretched and very crowded chemotherapy unit does not lend itself easily to this intervention. Clinical staff reported that it was disruptive and that the freezer took up valuable space in the unit. They also found it difficult to juggle the extra load entailed in the intervention within their usual task assignments. Expecting clinical nurses to assume the burden of ensuring the gloves were adequately cooled each day, determining whether the freezer was at the right temperature and documenting this, and remembering to check the glove temperature during the procedure and changing gloves in response, in the context of an already considerable workload, is not realistic.
Finally, the severity of cutaneous side effects is believed to be dependent on the amount of exposure to docetaxel; with a higher incidence of toxicities observed in patients scheduled for three or more cycles [25]. Given the change in length of docetaxel-containing treatment implemented during this study, wherein 3 × 21-day cycles of combination cyclophosphamide, epirubicin, 5-fluorouracil and docetaxel became the norm for breast cancer patients in our facility, frozen glove therapy is largely unnecessary. This observation is supported by Ishiguro et al., who recently evaluated the efficacy and comfort of frozen glove therapy in 16 breast cancer patients prescribed docetaxel [23]. Their investigation evaluated toxicities in patients who received a minimum of 5 months docetaxel treatment [23]. None of these patients developed hand or nail toxicities before this time [23]. Further data from Can et al.'s study of 201 patients also support this decision, indicating the only variable associated with the severity of toxicity is an increased number of taxane cycles [24].
Limitations
This study is limited by its small sample size: it is not adequately powered. While more patients might have been enrolled, the main study was stopped at n = 53 due to the high rate of discomfort with the intervention as reflected in the withdrawal rate. The small sample limits the generalisability of the results. Another limitation is that it was not practical to adhere to the manufacturer's recommendations regarding glove temperature; hence, the temperature was revised upwards to make the glove more acceptable to patients. While one other recent study reported that a more clinically acceptable temperature does not interfere with the efficacy of cryotherapy [23], it could nonetheless have influenced these results. A final limitation is that it is impossible to determine the effect of granulocyte colony stimulating factor (GCSF) in this study. A possible reason for the lack of response to the glove in this study compared to other studies is that during the pilot phase it became facility policy to administer GCSF to all breast cancer patients from the first cycle of any chemotherapy associated with dose-limiting neutropenia. An incidental benefit of this practice could be protection from cutaneous effects.
Conclusion
The results of this study indicate that cryotherapy in the form of frozen gloves for the cutaneous toxicities associated with docetaxel is safe in terms of infection control. However, its efficacy in terms of reducing the incidence, severity and time to onset of toxicities could not be established. In addition, its feasibility in terms of patient satisfaction and logistical obstacles for chemotherapy unit staff is questionable. These limitations preclude its routine use in our clinical setting.
References
MIMS Australia (2008) Docetaxel (Taxotere). MIMS annual. MIMS Australia Pty Ltd, St Leonards, NSW
Gligorov J, Lotz JP (2004) Preclinical pharmacology of the taxanes: implications of the differences. Oncologist 9(Supplement 2):3–8
Nagore E, Insa A, Sanmartin O (2000) Antineoplastic therapy-induced palmar plantar erythrodysesthesia (hand–foot syndrome): incidence, recognition and management. Am J Clin Derm 1:225–234
Winther D, Saunte DM, Knap M, Haahr V, Jensen AB (2007) Nail changes associated with docetaxel chemotherapy: a neglected side effect. 14th European Cancer Conference. Eur Oncol Soc, Barcelona
Zimmerman GC, Keeling JH, Burris HA, Cook G, Irvin R, Kuhn J et al (1995) Acute cutaneous reactions to Docetaxel, a new chemotherapeutic agent. Dermatology 131(2):4
Correia O, Azevedo C, Pinto Ferreira E, Braga Cruz F, Polonia J (1999) Nail changes secondary to Docetaxel (Taxotere). Dermatology 198(3):288–290
Wasner G, Hilpert F, Baron R, Pfisterer J (2001) Clinical picture: nail changes secondary to docetaxel. Lancet 357(9260):910
Scotte F, Tourani JM, Banu E, Peyromaure M, Levy E, Marsan S et al (2005) Multicenter study of a frozen glove to prevent docetaxel-induced onycholysis and cutaneous toxicity of the hand. J Clin Oncol 23:4424–4429
Battegay EJ (1995) Angiogenesis: mechanistic insights, neovascular diseases, and therapeutic prospects. J Mol Med 73(7):333–346
Baker J, Ajani J, Scotte F, Winther D, Martin M, Aapro MS et al (2008) Docetaxel-related side effects and their management. Euro J Oncol Nurs 12:253–268
Scotte FBE, Medioni J, Levy E, Ebenezer C, Marsan S et al (2008) Matched case control phase 2 study to evaluate the use of a frozen sock to prevent docetaxel-induced onycholysis and cutaneous toxicity of the foot. Cancer 112:1625–1631
Peterson D, Öhrn K, Bowen J, Fliedner M, Lees J, Loprinzi C et al (2013) Systematic review of oral cryotherapy for management of oral mucositis caused by cancer therapy. Support Care Canc 21(1):327–332
Katsimbri P, Bamias A, Pavlidis N (2000) Prevention of chemotherapy-induced alopecia using an effective scalp cooling system. Euro J Can 36:766–771
Ridderheim M, Bjurberg M, Gustavsson A (2003) Scalp hypothermia to prevent chemotherapy-induced alopecia is effective and safe: a pilot study of a new digitized scalp-cooling system used in 74 patients. Supp Care Can 11:371–377
Giaccone G, Di Giulio F, Morandini MP, Calciati A (1988) Scalp hypothermia in the prevention of doxorubicin-induced hair loss. Can Nurs 11(3):170–173
Komen MMC, Smorenburg CH, Van der Hurk CJ, Nortier JWR (2013) Factors influencing the effectiveness of scalp cooling in the prevention of chemotherapy-induced alopecia. Oncologist 18(7):885–891
Hayashi T, Fujita T, Mase T, Nakano S, Wada M, Kashizuka T, et al. (2009) Phase II clinical study of protection of nail change and skin toxicity using a frozen glove in Japanese patients with early breast cancer treated by docetaxel and cyclophosphamide. Canc Res 69(24): Supplement 3: Abstract 808.
Sakurai M, Todaka K, Takada N, Kamigaki S, Anami S, Shikata A, et al. (2009) Multicenter phase II study of a frozen glove to prevent docetaxel-induced onycholysis and cutaneous toxicity for breast cancer patients. Canc Res 69(2): Supplement 1: Abstract 4093.
DoHA (2004) Infection control guidelines for the prevention of transmission of infectious diseases in the health care setting. DoHA, Canberra
National Cancer Institute (NCI) (2009). Common toxicity criteria for adverse events. http://evs.nci.nih.gov/ftp1/CTCAE/About.html.
Cohen J (1992) A power primer. Psychol Bull 112(1):4
Goel MK, Khanna P, Kishore J (2010) Understanding survival analysis: Kaplan-Meier estimate. Int J Ayurveda Res 1(4):4
Ishiguro H, Takashima S, Yoshimura K, Yano I, Yamamoto T, Niimi M et al (2012) Degree of freezing does not affect efficacy of frozen gloves for prevention of docetaxel-induced nail toxicity in breast cancer patients. Supp Care Canc 20(9):2017–2024
Can G, Aydiner A, Cavdar I (2012) Taxane-induced nail changes: predictors and efficacy of the use of frozen gloves and socks in the prevention of nail toxicity. Euro J Oncol Nurs 16:270–275
Hong J, Park SH, Choi SJ, Lee SH, Lee KC, Lee J et al (2007) Nail toxicity after treatment with Docetaxel: a prospective analysis in patients with advanced non-small cell lung cancer. Japanese J Clin Oncol 37(6):4
Acknowledgments
The authors gratefully acknowledge the research grant from the Princess Alexandra Hospital Foundation that funded this study. We also thank Sanofi-Aventis for supply of the medical device investigated in this study.
Conflict of interest
The authors have no conflict of interest to declare
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McCarthy, A.L., Shaban, R.Z., Gillespie, K. et al. Cryotherapy for docetaxel-induced hand and nail toxicity: randomised control trial. Support Care Cancer 22, 1375–1383 (2014). https://doi.org/10.1007/s00520-013-2095-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-013-2095-x