Abstract
Purpose
Disease symptom management in patients with advanced non-small cell lung cancer (NSCLC) is a critical aspect of therapy. The main objective of our study was to assess patient-reported outcomes and the degree of concordance between physician and patient perceptions of symptom severity in advanced NSCLC in the USA.
Methods
Patients with advanced (stage IIIB/IV) NSCLC (N = 450) were recruited in a nationwide (USA) lung cancer study. Patients and their oncologists completed patient and physician versions of the Lung Cancer Symptom Scale (LCSS). Patient-reported lung cancer-specific quality of life was assessed with the Functional Assessment of Cancer Therapy—Lung (FACT-L). Concordance was assessed using the kappa-statistic. Regression analysis was performed with FACT-L total score as the dependent variable and patient-reported LCSS symptom scores as predictors.
Results
A high proportion of patients experienced lung cancer symptoms: fatigue (100 %), loss of appetite (97 %), shortness of breath (95 %), cough (93 %), pain (92 %), and blood in sputum (63 %). Concordance between physician and patients was lowest for loss of appetite (kappa 0.1701) and greatest for hemoptysis (kappa 0.4586). Loss of appetite (β = −0.204; p < 0.001), cough (β = −0.145; p < 0.01), pain (β = −0.265; p < 0.001), and shortness of breath (β = −0.145; p < 0.01) were found to be significant predictors of the quality of life.
Conclusions
Symptom burden in patients with advanced NSCLC is high and has a negative impact on the quality of life. Patient-reported outcomes data could help optimize disease outcomes and therapy management in NSCLC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer is the leading cause of cancer-related death in the USA. In 2011 alone, 221,000 new cases of the disease were diagnosed and an estimated 156,900 individuals died as a result of the disease [1]. The prognosis for patients with lung cancer is poor, with only approximately 15 % of patients still alive 5 years after their initial diagnosis [2]. Non-small cell lung cancer (NSCLC) accounts for more than 85 % of all lung cancer cases [1]. Only approximately 15 % of patients are diagnosed while the cancer is still confined to the primary site, and 56 % of patients are not diagnosed until their cancer has reached an advanced stage with the development of metastases [2]. This latter group has the poorest prognosis, with an estimated 5-year survival rate of just 3.6 % [2].
The most common symptoms associated with lung cancer include cough, shortness of breath, and chest pain. Studies in small cohorts of lung cancer patients have highlighted the detrimental impact of lung cancer symptoms on the quality of life (QoL) [3, 4]. However, few studies have systematically evaluated the relationship between lung cancer symptoms and QoL. Moreover, there is also an apparent lack of understanding of the agreement between patient and physician perception of symptom burden in NSCLC. A number of studies have highlighted a lack of concordance between patient and clinician reporting of cancer-related symptoms in patients with a variety of cancer diagnoses [5–7]. Such discrepancies may impair the ability of clinicians to identify areas of need for individual patients and thereby to meet the holistic needs of patients with and undergoing treatment for lung cancer.
The current real-world study was conducted to understand and evaluate the current burden of lung cancer-related symptoms and its impact on patient-reported QoL in patients with advanced NSCLC in the USA. In addition, the study assessed the degree of concordance between physician- and patient-reported lung cancer symptoms.
Patients and methods
Study design
The Adelphi NSCLC Disease Specific Program is a real-world, patient record-based study of oncologists in the USA. The study was undertaken in 2011 and is based on completion of detailed record forms by physicians (Physician Record Form—PRF) and self-completion questionnaires by eligible patients (Patient Self-completion Form—PSC). The study was conducted as per the Pharmaceutical Business Intelligence and Research Group code of conduct, and the physicians did receive reimbursement for participation in the survey in line with these guidelines.
Physician recruitment and eligibility
Eligible physicians were those actively involved in the management of patients with NSCLC who reported seeing at least five patients with advanced (stage IIIB/IV) NSCLC each week. In addition, physicians must have gained their medical qualification between 1978 and 2009.
Patient recruitment and eligibility
Participating physicians were asked to invite patients for whom they completed a PRF to complete a PSC. Eligible patients were those with advanced (stage IIIB/IV) disease receiving drug treatment. Each participating patient provided consent for anonymous and aggregated reporting of research findings. Patients who were participating in a clinical trial at the time of this study were excluded from participation.
Data collection
Physician Record Forms (physician completed)
Each participating physician completed a detailed PRF for their next five patients consulted with NSCLC who were receiving first-line treatment, five patients who were receiving second-line treatment, and two patients who were receiving third-line treatment for their NSCLC (12 patients in total) during the study period. Data collected via the PRF included patient demographics, medical and disease history (including hospitalizations), current and previous treatments for NSCLC, and co-morbidities. Physicians also completed the Observer version of the Lung Cancer Symptom Scale (LCSS) [8]. The Observer LCSS consists of six items which address the intensity of major lung cancer symptoms (loss of appetite, fatigue, cough, dyspnea, hemoptysis, and pain). Each item was given a numerical score from 100 (none) to 0 (severe). Specific descriptors of 0 (severe), 25 (marked), 50 (moderate), 75 (mild), and 100 (none) were provided with each question.
Patient Self-completion Forms
Patients completed the patient version of the LCSS as part of the PSC, as well as the Functional Assessment of Cancer Therapy—Lung (FACT-L) [9].
The patient version of the LCSS consists of nine items including six symptoms (appetite, fatigue, cough, shortness of breath [presented as dyspnea in the physician version of this tool], blood in sputum [presented as hemoptysis in the physician version], pain), total symptomatic distress, activity status, and global QoL with a recall period of ‘the past day.’ Each item is measured on a 100-mm visual analog scale extending from ‘as good as it could be’ to ‘as bad as it could be,’ and the patient is asked to place a mark along the line where it best described their symptoms. The three summation questions include total symptomatic distress, activity status, and global QoL. The mean of the six major lung cancer symptom scores can be combined to give an ‘average symptoms burden score,’ with a higher score indicating a higher severity of symptom burden [8].
The FACT-L contains four generic cancer-specific domains and one lung cancer-specific subscale. The general subscales include physical well-being (PWB), social/family well-being, emotional well-being, and functional well-being (FWB). The seven-item Lung Cancer Subscale (LCS) assesses the impact of symptoms commonly reported by lung cancer patients, including shortness of breath, loss of weight, and chest tightness. All of the questions are rated on a five-point Likert-type scale ranging from 0 (not at all) to 4 (very much). A Trial Outcome Index can be derived by adding scores on the PWB and FWB subscales to the LCS, with a maximum possible score of 84 (the PWB, FWB, and LCS subscales had seven questions each); the total FACT-L score had a maximum of 136. Higher scores represented better functioning and better QoL [9].
Patients completed the forms independently, and physicians were blinded to the responses of the patients (and vice versa).
Statistical analyses
Descriptive statistics were calculated (mean, standard deviation [SD]) as appropriate. The statistical significance of differences in the variables of interest was determined using appropriate statistical tests, including t tests. Categorical data were evaluated using chi-square tests or Fisher's exact test; ordinal data were evaluated using Mann–Whitney or Kruskal–Wallis tests.
A concordance analysis was conducted to evaluate agreement between patient- and physician-reported lung cancer symptoms using the kappa-statistic. To achieve this, LCSS observer and patient scores were grouped into five categories (0, 25, 50, 75, and 100) with scores rounded to the nearest 25. The observer scale categories were then reversed so that severity categories were comparable with the patient scale groupings (i.e. 0 = none, 100 = severe for both scales). The level of concordance was categorized according to Landis and Koch [10] with a kappa- statistic of <0 indicating ‘no agreement,’ 0–0.20 indicating ‘slight,’ 0.21–0.40 indicating ‘fair,’ 0.41–0.60 indicating ‘moderate,’ 0.61–0.80 indicating ‘substantial,’ and 0.81–1.0 indicating ‘almost perfect agreement.’
Finally, regression analyses were conducted to determine predictors of lung cancer-specific QoL. The FACT-L total score was the dependent variable in the regression model. Independent variables were the individual symptom scores reported by the patients on the LCSS. Age, gender, stage of disease, and performance status (Karnofsky score) were also used as independent variables.
Results
Demographics
A total of 101 physicians took part in the study and provided a total of 1,200 PRFs for individual patients. In all, 450 patients completed a PSC (38 % of those for whom a corresponding PRF was available). The demographics and disease history of the study population are presented in Table 1.
The majority of patients (70.2 %) receiving first-line treatment were prescribed combination therapy (most commonly carboplatin + paclitaxel, carboplatin + pemetrexed, and carboplatin + gemcitabine). Monotherapy was the most common treatment regimen among patients receiving second-line therapy (71.6 % of patients; the most common agents were erlotinib, pemetrexed, or gemcitabine).
Lung cancer symptom burden
At the time of the study, the majority of patients had lung cancer symptoms as reported by their physicians (769/886 patients; 86.8 %). The most common symptoms were persistent cough (520/803; 64.8 %), fatigue (608/807; 75.3 %), and dyspnea (436/738; 59.1 %).
Patients reported a mean overall LCSS total score of 400.7 (SD 195.7) and a mean symptom score of 42.3 (SD 21.5; Table 2). Mean scores for individual symptoms ranged from 18.4 for blood in sputum (hemoptysis) to 53.2 for fatigue. Patients with stage IV disease generally reported a greater symptom burden than did patients with stage IIIB disease. This was most marked (greater than ten point differences) for loss of appetite, fatigue, and pain. Patients with stage IV disease also reported a greater impact of disease-related symptoms on their ability to carry out normal daily activities (50.4 versus 38.9 points) and QoL (55.8 versus 45.1 points) compared with patients with stage IIIB disease.
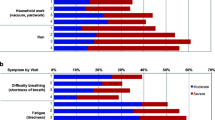
Physicians reported a mean overall LCSS total score of 449.8 (SD 90.2). Patients regarded the majority of their symptoms as moderate or marked in intensity, while physicians evaluated the majority of symptoms as being mild to moderate in intensity (Fig. 1). Overall, concordance between physician- and patient-reported lung cancer symptom burden was considered to be ‘slight’ based on the Landis and Koch [10] criteria (38 % agreement, kappa 0.1561; Table 3). Agreement was greatest for hemoptysis (agreement 70 %, kappa 0.4586) and lowest for loss of appetite (agreement 36 %, kappa 0.1701) and fatigue (agreement 40 %, kappa 0.2033).
FACT-L
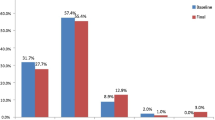
Patients reported a mean FACT-L score of 71.7; mean subscale scores ranged from 11.0 for the functional well-being subscale to 16.8 for the physical well-being subscale (Fig. 2).
The regression model found a significant negative impact on patient-reported lung cancer-specific QoL for loss of appetite (β = −0.204; p < 0.0001), cough (β = −0.145; p = 0.001), shortness of breath score (β = −0.145; p = 0.003), and pain (β = −0.265; p < 0.0001). Among the control variables, age (β = 0.217; p = 0.004) and performance status (β = 0.283; p < 0.0001) were found to be significant predictors of patient-reported lung cancer-specific QoL (Table 4).
Discussion
The current study is, to our knowledge, the first specific and comprehensive evaluation of the burden of lung cancer-related symptoms among patients with advanced NSCLC in the USA. The results of the current study have shown that the burden of lung cancer-specific symptoms in patients with advanced disease is high, even among patients receiving treatment within current guidelines. The perceived burden of cancer-related symptoms was found to be higher among patients with stage IV disease than those with stage IIIB disease, particularly for loss of appetite, fatigue, and pain. Patients with stage IV disease also reported a greater impact on their ability to carry out normal activities and on their QoL as a result of their cancer-related symptoms than those with stage IIIB disease. Consistent with previous studies, the current study has also highlighted some degree of discordance between the assessment of symptom intensity from the perspective of both patients and physicians [5, 6, 11]. The lowest level of agreement was observed for the purely patient-perceived/subjective symptoms of loss of appetite and fatigue, while the greatest level of agreement was observed for the objective symptoms of hemoptysis. Finally, this study also showed that the presence of a variety of patient-reported disease-specific symptoms (including cough, dyspnea, and pain) were predictive for poor QoL as indicated by low FACT-L scores.
A small number of studies have previously reported discordance between patient- and physician-reporting of cancer-related symptom burden. Oi-Ling et al. [5] evaluated the distress caused by a panel of 13 symptoms among 82 patients with advanced cancer in the last week of life as assessed by the patient, their caregiver, and their physician. Data for 30 patients were available, and the most common tumor was cancer of the lung. Caregiver ratings agreed well with those of patients for five of the 13 symptoms, including common lung cancer-related symptoms (dyspnea and cough); physician ratings agreed with patient ratings for just three of the 13 symptoms and physicians tended to underrate the distress. In an analysis of data from 2,279 patients with cancer taking part in 1 of 14 clinical trials supported by the European Organisation for Research and Treatment of Cancer, Quinten et al. [11] noted that patient- and physician-reported symptom scores differed. Most recently, Sikorskii et al. [6] examined the concordance between patient-reported cancer symptoms and physician reports as captured in the medical record. Using a checklist of 12 symptoms, they examined symptom reports among a cohort of 384 women with breast cancer who completed telephone interviews at baseline and after 5 and 11 weeks. They then compared patient-reported symptoms with those recorded in the medical record for each patient and found only poor to slight agreement between physician- and patient-reporting of the 12 symptoms. Finally, Vogelzang et al. [7] identified considerable disagreement between patients with a variety of cancers and their physicians in terms of the most distressing symptom and the level of impact of cancer-related symptoms on their daily lives. A lack of concordance between patient- and physician-assessed symptom burden has been identified in other clinical settings, including rheumatoid arthritis for the presence of tender and painful joints [12] and overall disease severity [13], respiratory illness [14], and anxiety and depression [15]. Such studies and the results of our analyses have shown the least level of agreement for symptoms such as shortness of breath or loss of appetite that have a subjective component compared to symptoms like hemoptysis that are more objective in nature. Our results thus highlight the importance of assessing symptoms both from an objective physician's perspective and from the subjective perspective of patients in order to capture a more comprehensive clinical picture that could help optimize therapy management outcomes.
The results reported here in a large cohort of patients with advanced disease are consistent with previous smaller studies that have shown that severity of symptom burden could impact general response to therapy [16] and that the presence of a number of lung cancer symptoms adversely impacts patients' QoL. Mohan et al. [3] reported that the cumulative symptom burden and all dyspnea measures adversely impacted on QoL in 101 patients with lung cancer. Xara et al. [4] reported that a number of lung cancer-related symptoms such as loss of appetite were associated with worse QoL among 56 patients with NSCLC. Taken together, the observations in these studies highlight the importance of symptom control in improving or at least maintaining the QoL in patients with advanced NSCLC. As such, novel therapies that can demonstrate a positive impact on these symptoms could help improve QoL in patients with advanced lung cancer.
Recent studies have suggested that, among patients with NSCLC, a higher burden of lung cancer-related symptoms may adversely affect both response to treatment [16] and overall survival [17]. In a small, survey-based pilot study among 30 patients with advanced NSCLC, the majority of patients (90 %) regarded symptom control as a crucial part of any maintenance chemotherapy regimen [18]. A separate study in 89 patients with advanced NSCLC found that improvements in progression-free survival (PFS) were regarded as important by patients only if disease symptoms were mild. In patients with severe disease symptoms, improvements in PFS were in fact regarded as detrimental [19]. Such studies highlight the need to understand the perceived burden of disease symptoms in patients with advanced NSCLC in order to meet the needs of such patients when developing care plans.
When considering the results presented here, it is important to acknowledge some limitations of our study. Data collected in our study were focused on the presence of perceived burden of symptoms in patients with advanced NSCLC at a single timepoint, which was at the time of the survey completion. Such an approach allows data to be captured for a large cohort of patients for a single point in time. Further studies will be required to evaluate the impact of change in symptoms or patient status over time. In addition, the current study focused only on patients with advanced disease (stage IIIB or IV) receiving drug treatment; perceptions of symptom burden may be different for those with earlier-stage disease. Further studies are also needed to address issues such as the acceptability of intensive treatment to achieve symptom palliation.
In conclusion, the results of the study presented here highlight the considerable burden of lung cancer-related symptoms among patients with advanced NSCLC in the USA. They also highlight the need to consider the patient's perception of the burden of lung cancer-specific symptoms when managing patients with advanced NSCLC and selecting treatments. Future therapies showing an improvement in lung cancer symptoms could lead to significant improvements in QoL and could provide incremental clinical value over current therapies.
References
National Comprehensive Cancer Network (NCCN). Non-small cell lung cancer. NCCN Guidelines, version 3.2012. Available at: http://www.nccn.org. Accessed July 2012
Surveillance Epidemiology and End Results (SEER). SEER Stat Fact Sheets: lung and bronchus. Available at: http://seer.cancer.gov/statfacts/html/lungb.html. Accessed July 2012
Mohan A, Singh P, Singh S, Goyal A, Pathak A, Mohan C, Guleria R (2011) Quality of life in lung cancer patients: impact of baseline clinical profile and respiratory status. Eur J Cancer Care 16:268–276
Xara S, Amaral TF, Parente B (2011) Undernutrition and quality of life in non-small cell lung cancer patients. Rev Port Pneumol 17:153–158
Oi-Ling K, Man-Wah DT, Kam-Hung DN (2005) Symptom distress as rated by advanced cancer patients, caregivers and physicians in the last week of life. Palliat Med 19:228–233
Sikorskii A, Wyatt G, Tamkus D, Victorson D, Rahbar MH, Ahn S (2012) Concordance between patient reports of cancer-related symptoms and medical records documentation. J Pain Symptom Manage 44:362–372
Vogelzang NJ, Breitbart W, Cella D, Curt GA, Groopman JE, Horning SJ, Itri LM, Johnson DH, Scherr SL, Portenoy RK (1997) Patient, caregiver, and oncologist perceptions of cancer-related fatigue: results of a tripart assessment survey. Semin Hematol 34(3 suppl 2):4–12
Hollen PJ, Gralla RJ, Kris MG, Potanovich LM (1993) Quality of life assessment in individuals with lung cancer: testing the Lung Cancer Symptom Scale (LCSS). Eur J Cancer 29A(suppl 1):S51–S58
Cella DF, Bonomi AE, Lloyd SR, Tulsky DS, Kaplan E, Bonomi P (1995) Reliability and validity of the Functional Assessment of Cancer Therapy-Lung (FACT-L) quality of life instrument. Lung Cancer 12:199–220
Landis JR, Koch CG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Quinten C, Maringwa J, Gotay CC, Martinelli F, Coens C, Reeve BB, Flechtner H, Greimel E, King M, Osoba D, Cleeland C, Ringash J, Schmucker-Von Koch J, Taphoorn MJ, Weis J, Bottomley A (2011) Patient self-reports of symptoms and clinician ratings as predictors of overall cancer survival. J Natl Cancer Inst 103:1851–1858
Barton JL, Criswell LA, Kaiser R, Chen YH, Schillinger D (2009) Systematic review and metaanalysis of patient self-report versus trained assessor joint counts in rheumatoid arthritis. J Rheumatol 36:2635–2641
Barton JL, Imboden J, Graf J, Glidden D, Yelin EH, Schillinger D (2010) Patient–physician discordance in assessments of global disease severity in rheumatoid arthritis. Arthritis Care Res (Hoboken) 62:857–864
Barbara AM, Loeb M, Dolovich L, Brazil K, Russell M (2012) Agreement between self-report and medical records on signs and symptoms of respiratory illness. Prim Care Respir J 21:145–152
McGrady A, Lynch DJ, Nagel RW, Tamburrino M (2010) Coherence between physician diagnosis and patient self reports of anxiety and depression in primary care. J Nerv Mental Dis 198:420–424
Mohan A, Singh P, Kumar S, Mohan C, Pathak AK, Pandey RM, Guleria R (2008) Effect of change in symptoms, respiratory status, nutritional profile and quality of life on response to treatment for advanced non-small cell lung cancer. Asian Pac J Cancer Prev 9:557–562
Wang XS, Shi Q, Lu C, Basch EM, Johnson VE, Mendoza TR, Mobley GM, Cleeland CS (2010) Prognostic value of symptom burden for overall survival in patients receiving chemotherapy for advanced non-small cell lung cancer. Cancer 116:137–145
Peeters L, Silbille A, Anrys B, Oyen C, Dooms C, Nackaerts K, Wauters I, Vansteenkiste J (2012) Maintenance therapy for advanced non-small cell lung cancer: a pilot study on patients’ perceptions. J Thorac Oncol 7:1291–1295
Bridges JF, Mohamed AF, Finnern HW, Woehl A, Hauber AB (2012) Patients’ preferences for treatment outcomes for advanced non-small cell lung cancer: a conjoint analysis. Lung Cancer 77:224–231
Acknowledgments
The Adelphi Lung Cancer Disease Specific Program was supported by Pfizer and other pharmaceutical companies; the collection of patient-reported outcomes and related analyses was sponsored by Pfizer Inc. Editorial assistance was provided by Martin Quinn at ACUMED® (Tytherington, UK) and funded by Pfizer Inc.
Conflicts of interest
Shrividya Iyer is an employee of Pfizer Inc. Adam Roughley, Alex Rider, and Gavin Taylor-Stokes are employees of Adelphi Real World, who were paid contractors to Pfizer Inc and were involved in study design, data collection, analyses, and manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Iyer, S., Roughley, A., Rider, A. et al. The symptom burden of non-small cell lung cancer in the USA: a real-world cross-sectional study. Support Care Cancer 22, 181–187 (2014). https://doi.org/10.1007/s00520-013-1959-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-013-1959-4