Abstract
Purpose
Screening programs for colorectal cancer aim at reducing cancer mortality. We assessed psychological effects of being invited to an immunochemical fecal test (FIT)-based screening program.
Methods
Asymptomatic persons aged 50–74 years were invited to a Dutch screening pilot. The Psychological Consequences Questionnaire (PCQ) was used to measure the psychological effects of screening. Screen positives had two additional measurements: before undergoing the colonoscopy and 4 weeks after receiving the colonoscopy findings.
Results
A number of 3,828 invitees (46 % male, mean age 60 years) completed the first PCQ. FIT positives had a higher mean total PCQ score (8.32, SD 8.84; score range 0–36) than those who declined participation (3.72, SD 6.30); participants still waiting for their FIT result had a mean score of 2.74 (SD 5.11), and those with a negative FIT result had the lowest score (2.06, SD 4.43) (p < 0.001). In the 373 FIT positives who underwent colonoscopy, 195 completed the pre-colonoscopy questionnaire and 253, the post-colonoscopy questionnaire. Mean total, physical, and social PCQ scores had decreased significantly between the first questionnaire and the pre-colonoscopy one, but scores on the emotional subscale did not. In false-positives, mean total, physical, and emotional PCQ scores decreased significantly, while in true-positives, a significant decrease in mean emotional PCQ score was observed.
Conclusion
Psychological consequences for invitees to a Dutch FIT-based colorectal cancer screening pilot differ, depending on timing and FIT result. FIT positives are more distressed than FIT negatives. FIT positives still experience psychological distress 6 weeks after a normal colonoscopy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Screening programs for colorectal cancer (CRC) aim at detecting CRC in an early stage and thereby decreasing CRC-related morbidity and mortality. As is the case with any screening program, only a few persons will directly benefit from participation, whereas a large proportion of invitees have to undergo screening. Invitees are confronted with the possibility of having cancer, which can cause distress by itself.
Most of what is known on adverse psychological effects following screening stems from studies among women invited for breast cancer screening [1–8]. These studies focused mainly on adverse effects associated with receiving false-positive mammography results, since these women are exposed to distress surrounding a positive screen but do not benefit in terms of an early detection of significant lesions. A recent meta-analysis of 17 studies demonstrated that receiving a false-positive mammogram was associated with greater anxiety and distress about breast cancer [9]. Negative psychological effects can persist for up to 3 years after the screening process [10, 11].
To our knowledge, only two studies have addressed negative psychological effects or distress in screening for colorectal cancer using stool tests [12, 13]. These Scandinavian studies demonstrated no substantial adverse effects on psychological well-being 12 months following CRC screening. We designed a study to assess the psychological effects of being invited for and participating in a pilot CRC screening program using a fecal immunochemical test (FIT). We aimed to explore differences in psychological effects cross-sectionally after receipt of the invitation in all invitees and longitudinally in participants with a positive FIT result.
Methods
Data were collected in the second round of a Dutch biennial FIT-based CRC screening pilot in the Amsterdam region. The program design of the first and second round has been reported in detail elsewhere [14, 15]. A summary is given below.
Design of the second round of the screening pilot
In 2008, a random sample of average-risk persons aged 50 to 74, living in the screening pilot catchment area in the Amsterdam region of the Netherlands, was selected from the population database, based on date of birth and postal code. They were sent an invitation package for a second screening round 2 years after the first round. All first round invitees were approached regardless of whether or not they had participated in the first round. The first round of the screening pilot was conducted in 2006; in that round, invitees had been randomly allocated to receive either a guaiac fecal occult blood test or a FIT. All persons who had been invited for the first round and who still fulfilled eligibility criteria were invited again for the second round. Those who had a positive test result in the first round were not re-invited but enrolled in a surveillance program according to the Dutch guidelines when indicated [16].
Invitation
The invitation package included an invitation letter, an information leaflet, a FAQ card, and the FIT with a detailed test instruction. The FIT used was the OC-Sensor, developed by Eiken, Tokyo, Japan. This was a single test, sampled at one occasion. In the invitation letter, invitees were instructed not to take part in the screening but to contact their general practitioner in case of bloody stool or changed bowel habits during the last 3 months. The information leaflet included information on the screening procedure, the meaning of a positive and a negative test result, the possibilities of false-positive and false-negative test results, and a figure illustrating the chances of having a positive test result and of being diagnosed with advanced adenomas or CRC at the follow-up procedure (colonoscopy). The information leaflet was designed specifically for this study. It was based on a review of the literature and on feedback from the first round. It was put together in close relation with a linguistic expert specialized in patient information provision.
Screening procedure
Invitees could participate in the screening pilot by performing the FIT at home and returning the test in a postage-free envelope. They received the results within 2 weeks after performing the test. Participants with a negative test result were informed through a letter by postal mail. The message specified that the stool sample did not contain blood and that follow-up investigations were unnecessary at this time. The letter explained that a negative test result does not guarantee complete absence of significant lesions and emphasized that persons should contact their general practitioner in case of any alarming symptoms suggestive of cancer, such as blood in stool, or changed bowel habits.
In case of a positive test result, screening participants were informed through a letter that the test result was unfavorable, explaining that blood was detected in their stool sample. The blood could be indicative of cancer but could also come from other, less serious, sources, such as hemorrhoids, benign polyps, or fissures. Participants with a positive test result were invited for a visit to the screening center. In the absence of contraindications, they were scheduled for colonoscopy within 2 weeks. On the day of the colonoscopy, participants were informed about the preliminary results before going home. Two weeks after the colonoscopy, they were contacted by phone or invited for a face-to-face consultation to discuss the histopathological results and follow-up procedures.
Psychological consequences of screening questionnaire
Psychological consequences of screening were elicited with a questionnaire, distributed at three different time points. We sent a first questionnaire 2 weeks after the invitation. To distinguish between participants that had already been informed on their test result and participants that were still waiting, we included two additional items in this first questionnaire, asking whether or not participants had already performed the test and whether or not they had been informed about the results.
We sent a second questionnaire to participants with a positive test result just before the colonoscopy procedure and a third questionnaire to all positive screenees that underwent a colonoscopy 4 weeks after they had been informed about the colonoscopy results, which is about 6 weeks after the colonoscopy had taken place.
To evaluate psychological consequences of screening, we used the Dutch version of the Psychological Consequences of Screening Questionnaire (PCQ). This is a validated measure of screen-specific anxiety, originally designed for breast cancer screening [17, 18]. The PCQ consists of 22 items. Since the focus of our study was on adverse psychological effects, we only used the 12 items on the negative consequences of screening.
With the PCQ, invitees were asked to indicate how often they had experienced each of a list of 12 symptoms “over the past week as a consequence of thoughts and feelings about colorectal cancer.” Answers could be given on a four-point Likert scale anchored at 0 (not at all) and at 3 (quite a lot of the time). The 12 items referred to effects of screening on an individual’s functioning, on the emotional domain (e.g., feeling down, feeling nervous, worried about future), the social domain (e.g., holding back, having trouble going to work/meeting others), and physical life (e.g., sleep disturbances, changed appetite). The answers resulted in a score for each of the three domains and a total score. Higher scores indicate more adverse effects. The PCQ total score can range between 0 and 36; the emotional subscale score, between 0 and 15; the social subscale score, between 0 and 9; and the physical subscale score, between 0 and 12.
Data analysis
We included data in the analysis from all invitees that had returned the first questionnaire. We analyzed the data by time point and by test result. The primary analysis focused on the PCQ total score; additional analyses were done for the PCQ emotional, physical, and social subscores.
Data for the first time point were analyzed conditional on the responses to the question whether or not invitees had performed the FIT and, if so, whether or not they had already been informed about the test result and, if so, on the test result (positive or negative). For those that had indicated that they had been informed about the test results, we retrieved the result from the screening database. A hemoglobin value of 50 ng/ml was used as the test positivity threshold: hemoglobin levels of over 50 ng/ml were classified as a positive test result and hemoglobin levels under 50 ng/ml as negative. This way, we could classify respondents into four groups: invitees who had not performed the test at the time of completing the first questionnaire, invitees who had performed the test but who were still waiting for their result, invitees who had performed the test and had received a negative test result, and persons who had performed the test and had received a positive test result. For each group, we computed a mean PCQ total score at the first time point. We compared means between groups using the ANOVA test statistic. We hypothesized that scores would be different, with participants that had already been informed about a negative test result having the lowest score and participants that had been informed about a positive test result the highest score.
We then analyzed the scores at the second time point, prior to colonoscopy. We computed a mean total PCQ score for all FIT positives who had returned the pre-procedure questionnaire and compared it with the scores of the subgroup that was already aware of their positive FIT result at the first time point. We hypothesized that the pre-colonoscopy PCQ total score would be higher than the first PCQ score in this subgroup. This hypothesis was based on our experience that persons who have to undergo a colonoscopy to rule out cancer appear to be rather anxious before undergoing the procedure. To test for a significant change in PCQ total score, we included all FIT-positive participants with a both a baseline PCQ total score and a pre-colonoscopy PCQ total score to compute a paired t test statistic.
For our analysis of the third time point, post-colonoscopy, we organized the participants into two groups, based on their colonoscopy results: persons with a true-positive FIT result and persons with a false-positive FIT result. Persons with a true-positive FIT result were those in whom at least one carcinoma or advanced adenoma had been detected at colonoscopy. Advanced adenomas were adenomas at a size of 10 mm or larger or adenomas with a villous component of more than 20 % or high-grade dysplasia. All other participants who had undergone the colonoscopy were classified as false-positives. We hypothesized that the post-colonoscopy PCQ score would be higher for true-positives than for false-positives and tested the difference using ANOVA. To test for significant changes in PCQ score before and after colonoscopy, we included all FIT-positive participants with both a pre-colonoscopy and a post-colonoscopy PCQ score to compute paired t test statistics.
Since this is one of the first papers looking at the psychological consequences of population-based CRC screening, and most prior data come from female populations only, in breast cancer and cervical screening programs, we also performed some exploratory analyses looking at gender differences in PCQ scores. A significance level of 0.05 was used in all hypothesis tests. Data were analyzed using the statistical software SPSS 18.0.
Ethical approval
Ethical approval for the screening program and data collection was provided by the Dutch Health Council (2005/03WBO, The Hague, The Netherlands).
Results
A total of 10,265 persons were invited for participation in the second screening round; 49 % were male, mean age 60 ± 7. Of these, 5,367 (52 %) returned the FIT; 424 of these participants (8 %) had a positive test result. Most test positives (n = 373; 88 %) underwent a follow-up colonoscopy, of which 163 (44 %) turned out to have a true-positive test result versus 210 (56 %) with a false-positive test result.
First questionnaire
Overall, 3,828 invitees (37 %) completed the first PCQ questionnaire. Table 1 shows the characteristics of questionnaire responders and nonresponders. As can be appreciated from this table, males were less likely to return the questionnaire, and questionnaire responders were older on average than nonresponders. Of those who returned the first PCQ, 228 (6 %) had not performed the test at the time of questionnaire completion; 1,385 (36 %) had performed the test but were still waiting on their test result; 2,053 (53 %) had already received a negative test result; and 162 (4 %) had already received a positive test result.
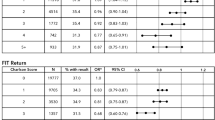
Figure 1a–d shows the mean PCQ total scores as well as the mean scores for the emotional, physical, and social subscales for the four groups specified above. The mean PCQ total score at the first time point was higher in participants who had received a positive test result (mean total PCQ score 8.32, SD 8.84, 95 % CI 6.95 to 9.69), than in those who had not performed the test (mean PCQ 3.72, SD 6.30, 95 % CI 2.90 to 4.54) and participants who were still waiting on their result (mean PCQ 2.74, SD 5.11, 95 % CI 2.47 to 3.01). The mean PCQ total score was lower in those who had received a negative test result (mean PCQ 2.06, SD 4.43, 95 % CI 1.87 to 2.25). These differences were statistically significant (p < 0.001). Similar patterns were observed for the three PCQ subscales: overall group differences in mean score at the first time point were significantly different (p < 0.001). Additional pairwise analyses showed no significant difference between the “no-test-performed” subgroup and the “waiting-for-test-result” subgroup on the PCQ physical and PCQ social subscales.
a Changes in mean PCQ total score (score range 0–36). b Changes in mean PCQ emotional subscore (score range 0–15). c Changes in mean PCQ physical subscore (score range 0–12). d Changes in mean PCQ social subscore (score range 0–9). All figures show the mean score in function of time. Error bars represent the standard error of the mean
No significant differences were found between men and women without a test result. In those who had been informed about their result, significantly lower mean total PCQ scores were observed in men compared with women: 6.9 versus 10.1 after a positive test result (p = 0.021) and 1.8 versus 2.2 after a negative test result; (p = 0.025).
Furthermore, in those who had been informed about their negative result, significantly higher mean total PCQ scores were observed in previous nonparticipants compared with previous participants (2.7 versus 1.9; p = 0.029).
Pre-colonoscopy analysis in FIT positives
Of the 373 FIT positives who underwent a colonoscopy 195 (52 %) completed both the first and the pre-colonoscopy questionnaire. Their mean pre-colonoscopy PCQ total score was 6.86 (SD 6.78, 95 % CI 5.91 to 7.82), significantly lower than the mean score in those who had learned of a positive FIT result at the time of first questionnaire completion (p = 0.020). The mean PCQ score on the physical and social subscales showed a significant decrease between the first and the pre-colonoscopy measurement (p = 0.017 and p = 0.010 respectively) but scores on the emotional subscale remained at a similar level (p = 0.31). Mean pre-colonoscopy PCQ total score was lower in men than in women (5.7 versus 8.0; p = 0.017).
No significant differences in mean pre-colonoscopy scores were observed between previous participants, previous nonparticipants and first time invitees (7.0, 5.7 and 7.9 respectively; p = 0.48).
Post-colonoscopy analysis comparing true-positives and false-positives
Of the 373 FIT positives who underwent a colonoscopy, 253 (68 %) persons also completed the post-colonoscopy questionnaire: 133 (82 %) of true-positives and 112 (53 %) of false-positives. We observed no significant differences between false-positives and true-positives in mean post-colonoscopy PCQ scores, neither for the PCQ total nor for any of the PCQ subscales (Fig. 1). Analysis of the changes in PCQ score over time within subjects (n = 144) showed that in false-positives, the mean PCQ total and mean PCQ physical and emotional subscale scores were significantly lower after colonoscopy—reflecting fewer adverse psychological consequences—whereas the mean PCQ social score remained at a similar level (p = 0.32). In true-positives, a significant decrease in mean PCQ score was observed for the emotional subscale only (p = 0.026). Mean post-colonoscopy PCQ total score was similar in men and in women (4.9 versus 5.9; p = 0.28). Also, no differences in mean post-colonoscopy PCQ total score were observed between previous participants, previous nonparticipants, and first-time invitees (5.3, 5.7, and 5.0, respectively; p = 0.91).
Discussion
We observed that being invited for FIT-based CRC screening was associated with different levels of psychological distress, depending on the FIT result and the time point in the screening process. Adverse psychological effects of participation were most pronounced shortly after having been informed about a positive test result. Just before undergoing the colonoscopy, the overall level of psychological distress was significantly lower. We argue that this might be due to the consultation at the outpatient clinic that participants had attended in the mean time, during which the meaning and possible consequences of positive test result were elaborately discussed. Nevertheless, scores on the emotional subscale remained increased just before undergoing the colonoscopy.
Six weeks after the colonoscopy, overall psychological distress was lower compared to pre-procedure values, in both true- and false-positives. Surprisingly, no significant differences were observed between false-positives and true-positives in mean post-colonoscopy PCQ scores. A false-positive colonoscopy result seems not to be associated with some kind of appeasing effect as we would have expected. This could, in part, be due to the definition of true-positives and false-positives that were chosen in this study. A true-positive result was defined as at least one advanced neoplasia (advanced adenoma or cancer) and false-positive, as no advanced neoplasia. To screenees, however, this distinction might not be as clear. Possibly, if one would divide the group into persons with cancer and persons without cancer, the results would be different. Since the group of persons diagnosed with cancer was small in this study population, such an analysis was not feasible. Future studies should look into this in more detail.
We are aware of two other studies that looked at psychological effects of being invited for cancer screening using stool tests. Both studies used other measures, making direct comparison difficult. A recent Danish study evaluated the psychological distress following fecal occult blood test screening among average-risk persons invited for participation in a feasibility study [12]. They found that at baseline, test-positive participants were more likely to be worried of having CRC and expressed a higher degree of concern about participating in the actual screening program. They also had significantly higher somatization, depression, and anxiety scores compared to test negatives. After 3 months, only anxiety scores remained significantly higher in test positives, and at 12 months, no significant differences in any of the domains remained.
Lindholm and colleagues assessed distress created by a stool test-based CRC screening program in participants and nonparticipants by a combination of a questionnaire and a telephone survey [13]. They found that 16 % of participants and 15 % of nonparticipants reported severe distress after having received the invitation letter. In around 40 % of both participants and nonparticipants, this distress lasted for more than a week. Surprisingly, the effects of this distress on daily life were more pronounced for nonparticipants. The observation that nonparticipants experienced more effects on their daily life than participants is similar to one of our findings: nonparticipants experienced higher levels of psychological distress than persons still waiting on their test result, and persons that had already received a negative test result. These findings suggest that merely receiving an invitation to participate in screening can cause severe distress. Another explanation could be that nonparticipants are selectively not participating in screening, because of the induced distress or feelings of fear.
In Dutch cervical cancer screening, Korfage and colleagues have used the PCQ to assess psychological distress in women with low-grade abnormalities in their Pap smear. They compared these to a reference group of cervical screening participants awaiting smear taking [19]. The mean total PCQ score was five in the group with abnormalities. This score was slightly lower than in FIT positives in our population (8.32). A Swiss study that also assessed psychological consequences of a false-positive mammography result showed results more similar to ours [5]. They assessed the level of psychological consequences in screen positives 8 weeks after the notification that no abnormalities were found at follow-up. These women had a mean emotional score of around 3, a PCQ social score of 1, and a PCQ physical score of 2. When we compare these numbers to the PCQ scores we observed in false-positives, 6 weeks after the notification that no abnormalities were found at colonoscopy, we observed fairly similar scores.
As can be appreciated from the discussion above, most data on psychological consequences of screening stem from studies among women. To see whether men and women experience screening differently, we performed some exploratory analyses. We observed that men who took part in screening tend to have lower scores, indicating less psychological consequences, although at the final time point, scores were similar. Future studies should look at these differences more carefully.
Strengths of this study are the large number of persons that completed the questionnaire and the fact that it was conducted among a genuine screening population. The design of the questionnaire allowed us to compare four different groups of invitees at baseline: nonparticipants, participants still waiting on their result, and persons already aware of their result. A limitation is the relatively low response rate among nonparticipants. This makes it difficult to generalize scores observed at the first time point to the complete group of nonparticipants. A second limitation is that we cannot exclude selection bias. It is possible that invitees who experienced high levels of psychological distress were more likely to return the questionnaire. Furthermore, both screening naïve persons and persons who had already been invited to a first round were invited to participate. We also do not have PCQ scores from a reference population unexposed to screening that could have been used for comparison. We can only compare differences in psychological consequences within invitee subgroups exposed to the screening invitation. And since screen positives were only followed up once after colonoscopy, at 6 weeks, we do not know how scores develop over a longer period of time.
In conclusion, this study and the data described above show that being invited for participation in a screening program can cause psychological distress in invitees, depending on the test result and the time point in the screening process. Although some level of distress seems inevitable after receiving a positive screening result, we also showed that test-positive persons in whom no significant lesions were found at colonoscopy—the false-positives—still experienced distress 6 weeks after the procedure. We should be aware of these adverse effects and try to minimize them as much as possible, especially in those persons who do not directly benefit from screening in terms of early detection of (pre)cancerous lesions. Future studies should explore the evolution of these adverse effects in CRC screening to answer the question whether these scores remain at an elevated level, or return to baseline in, for example, 12 months time.
References
Barton MB, Morley DS, Moore S, Allen JD, Kleinman KP, Emmons KM, Fletcher SW (2004) Decreasing women’s anxieties after abnormal mammograms: a controlled trial. J Natl Cancer Inst 96:529–538
Bowland L, Cockburn J, Cawson J, Anderson HC, Moorehead S, Kenny M (2003) Counselling interventions to address the psychological consequences of screening mammography: a randomised trial. Patient Educ Couns 49:189–198
Gilbert FJ, Cordiner CM, Affleck IR, Hood DB, Mathieson D, Walker LG (1998) Breast screening: the psychological sequelae of false-positive recall in women with and without a family history of breast cancer. Eur J Cancer 34:2010–2014
Lowe JB, Balanda KP, Del MC, Hawes E (1999) Psychologic distress in women with abnormal findings in mass mammography screening. Cancer 85:1114–1118
Meystre-Agustoni G, Paccaud F, Jeannin A, Dubois-Arber F (2001) Anxiety in a cohort of Swiss women participating in a mammographic screening programme. J Med Screen 8:213–219
Olsson P, Armelius K, Nordahl G, Lenner P, Westman G (1999) Women with false positive screening mammograms: how do they cope? J Med Screen 6:89–93
Sandin B, Chorot P, Valiente RM, Lostao L, Santed MA (2002) Adverse psychological effects in women attending a second-stage breast cancer screening. J Psychosom Res 52:303–309
Scaf-Klomp W, Sanderman R, van de Wiel HB, Otter R, van den Heuvel WJ (1997) Distressed or relieved? Psychological side effects of breast cancer screening in The Netherlands. J Epidemiol Community Health 51:705–710
Salz T, Richman AR, Brewer NT (2010) Meta-analyses of the effect of false-positive mammograms on generic and specific psychosocial outcomes. Psychooncology 19:1026–1034
Brett J, Austoker J (2001) Women who are recalled for further investigation for breast screening: psychological consequences 3 years after recall and factors affecting re-attendance. J Public Health Med 23:292–300
Brett J, Bankhead C, Henderson B, Watson E, Austoker J (2005) The psychological impact of mammographic screening. A systematic review. Psychooncology 14:917–938
Brasso K, Ladelund S, Frederiksen BL, Jorgensen T (2010) Psychological distress following fecal occult blood test in colorectal cancer screening—a population-based study. Scand J Gastroenterol 45:1211–1216
Lindholm E, Berglund B, Kewenter J, Haglind E (1997) Worry associated with screening for colorectal carcinomas. Scand J Gastroenterol 32:238–245
Denters MJ, Deutekom M, Fockens P, Bossuyt PM, Dekker E (2009) Implementation of population screening for colorectal cancer by repeated fecal occult blood test in the Netherlands. BMC Gastroenterol 9:28
van Rossum LG, van Rijn AF, Laheij RJ, van Oijen MG, Fockens P, van Krieken HH, Verbeek AL, Jansen JB, Dekker E (2008) Random comparison of guaiac and immunochemical fecal occult blood tests for colorectal cancer in a screening population. Gastroenterology 135:82–90
Nagengast F, Kaandorp C (2002) Follow-up na poliepectomie. Herziene richtlijn. Kwalititeitsinstituut voor de Gezondheidszorg CBO
Cockburn J, De LT, Hurley S, Clover K (1992) Development and validation of the PCQ: a questionnaire to measure the psychological consequences of screening mammography. Soc Sci Med 34:1129–1134
Rijnsburger AJ, Essink-Bot ML, van As E, Cockburn J, de Koning HJ (2006) Measuring psychological consequences of screening: adaptation of the psychological consequences questionnaire into Dutch. Qual Life Res 15:933–940
Korfage IJ, van Ballegooijen M, Huveneers H, Essink-Bot ML (2010) Anxiety and borderline PAP smear results. Eur J Cancer 46:134–141
Acknowledgments
The authors thank ZonMW for funding (project numbers 120710007 and 63000004). We also thank the Comprehensive Cancer Center Amsterdam for their contributions to the study and Karin de Groot for research assistance.
Conflict of interest
None
Author information
Authors and Affiliations
Corresponding author
Additional information
Trial Registration Number: NTR1327
Rights and permissions
About this article
Cite this article
Denters, M.J., Deutekom, M., Essink-Bot, M.L. et al. FIT false-positives in colorectal cancer screening experience psychological distress up to 6 weeks after colonoscopy. Support Care Cancer 21, 2809–2815 (2013). https://doi.org/10.1007/s00520-013-1867-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-013-1867-7