Abstract
Background
Uncontrolled studies show fatigue, anorexia, depression, and mortality are associated with low testosterone in men with cancer. Testosterone replacement improves quality of life and diminishes fatigue in patients with non-cancer conditions. The primary objective was to evaluate the effect of testosterone replacement on fatigue in hypogonadal males with advanced cancer, by the Functional Assessment of Chronic Illness Therapy-Fatigue subscale (FACIT-Fatigue) at day 29.
Methods
This is a randomized, double-blinded placebo-controlled trial. Outpatients with advanced cancer, bioavailable testosterone (BT) <70 ng/dL and fatigue score >3/10 on the Edmonton Symptom Assessment Scale were eligible. Intra-muscular testosterone or sesame seed oil placebo was administered every 14 days to achieve BT levels 70–270 ng/dL.
Results
Sixteen placebo and 13 testosterone-treated subjects were evaluable. No statistically significant difference was found for FACIT-fatigue scores between arms (−2 ± 12 for placebo, 4 ± 8 for testosterone, p = 0.11). Sexual Desire Inventory score (p = 0.054) and performance status (p = 0.02) improved in the testosterone group. Fatigue subscale scores were significantly better (p = 0.03) in those treated with testosterone by day 72.
Conclusions
Four weeks of intramuscular testosterone replacement in hypogonadal male patients with advanced cancer did not significantly improve quality of life. Larger studies of longer duration are warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypogonadism is found in two thirds of men with advanced cancer [1, 2] and in about half of men newly diagnosed with solid tumors [3]. Uncontrolled studies show that fatigue, anorexia, depression, insomnia, and survival [4] are associated with low testosterone in men with cancer. Testosterone replacement improves quality of life and diminishes fatigue [5] in patients with non-cancer conditions.
Patients with advanced cancer frequently identify fatigue as the main impairment to their quality of life [6]. Fatigue can stem from multiple causes encompassing biological, physiological, and psychosocial domains. Unfortunately, there are few effective therapies; however, hypogonadism may be a significant, potentially treatable contributor to fatigue in male patients with cancer. Clinical practice guidelines by the Endocrine Society [7] address testosterone replacement in patients with chronic conditions such as HIV, but not in patients with cancer. Our group has published studies showing a very high prevalence of hypogonadism in male patients with cancer, particularly those on opioid therapy [8, 9]. Low testosterone levels correlated with fatigue, lower FACIT-fatigue [1] scores, and other symptoms such as depression, poor appetite, insomnia [4], and decreased sexual desire.
Patients with cancer may develop primary or secondary hypogonadism because of impaired hypothalamic-pituitary axis function, antineoplastic treatments [10], megestrol acetate [11], or opioid therapy. There are several studies in non-cancer patients showing that testosterone replacement improves symptoms [12], sexual desire [13], physical strength, mood, and cognition [14]. Testosterone replacement in HIV+ men also increases lean body mass and strength [15].
Based on the benefits of testosterone replacement in non-cancer conditions, our hypothesis was that testosterone replacement in hypogonadal males with cancer would improve symptoms of fatigue, depression, anxiety as well as physical strength, stamina, and sexual desire. The primary objective was to evaluate the effect of testosterone replacement therapy on fatigue in hypogonadal male patients with advanced cancer, as measured by the Functional Assessment of Cancer Therapy-Fatigue (FACIT-F) and its subscale (FACIT-Fatigue) after 4 weeks. The secondary objectives were to evaluate the effect of testosterone replacement therapy on additional symptoms associated with hypogonadism, including depression, measured by Hospital Anxiety and Depression Scale (HADS), low sexual desire, measured by the Sexual Desire Inventory (SDI-2) and cachexia-related quality of life, measured by the Functional Assessment of Anorexia/Cachexia Treatment scale (FAACT). Other secondary objectives were to evaluate the effect of 4 weeks of testosterone replacement therapy on Eastern Cooperative Oncology Group (ECOG) performance status and physical performance, including handgrip strength by dynamometry, the timed Get-up-and-Go test, and the 6-min walk.
Methods
Study design
A randomized, double-blinded placebo-controlled trial was conducted at Michael E. De Bakey Veterans Affairs Medical Center (VA) and University of Texas MD Anderson Cancer Center (MDACC). Ambulatory clinic outpatients with advanced cancer as defined by either metastatic cancer or locally recurrent cancer were eligible. Bioavailable testosterone (BT) <70 ng/dL, hemoglobin >9 g/dL, Eastern Cooperative Oncology Group (ECOG) performance status <3, and moderate to severe fatigue as assessed by a score >3/10 on the Edmonton Symptom Assessment Scale (ESAS) were criteria for inclusion.
Contraindications to testosterone therapy or other causes of fatigue such as hypothyroidism, hypercalcemia, uncontrolled diabetes, decompensated congestive heart failure, chronic obstructive pulmonary disease requiring oxygen replacement, excluded subjects. Patients with a creatinine clearance <60 ml/min; a history of prostate cancer; severe depression defined by a HADS score ≥15; an abnormal digital rectal exam or prostate specific antigen (PSA) level >4.0 ng/mL were also excluded. Informed consent was obtained from eligible subjects who were then electronically randomized on a 1:1 ratio to testosterone treatment or placebo. The study was approved by the Institutional Review Board of MD Anderson Cancer Center and Baylor College of Medicine. All participants gave informed consent.
Intervention
Testosterone was administered intramuscularly using a weight-based dose titrated every 14 days to a bioavailable testosterone (BT) goal of 70–270 ng/dL. Gluteal injections of 150 or 200 mg testosterone enanthate (Delatestryl, BTG Pharmaceuticals Corporation for Bristol-Myers Squibb, Princeton, NJ 08543) or matching placebo (sesame seed oil) were administered at baseline, day 15, day 29, day 43, and day 57. Starting doses were 150 mg if ≤70 kg and 200 mg if >70 kg. Low testosterone was defined using a BT < 70 ng/dL, a value based on the lowest concentration reported in healthy eugonadal men aged 20–45 [16]. A titration regimen was followed: if nadir of BT was ≤70 ng/dL, the dose increased by 50 mg/injection. If the BT level >70 ng/dL, but less than 270 ng/dL, the dose was maintained. If the level was ≥270 ng/dL, the dose was decreased by 50 mg/injection. The maximum dose provided was 300 mg, and the minimum dose was 50 mg. However, in an effort to maintain blinding, all doses were standardized to a dose volume of 2 mL, regardless of randomization.
Assessments
-
1.
The Edmonton Symptom Assessment Scale assesses ten symptoms experienced by cancer patients during the previous 24 h: pain, fatigue, nausea, depression, anxiety, drowsiness, dyspnea, anorexia, sleep disturbance, and feelings of well-being [17]. The severity of each symptom is rated on a numerical scale of 0–10 (0 = no symptom, 10 = worst possible severity). The ESAS is both valid and reliable in the assessment of the intensity of symptoms in cancer patients [18].
-
2.
Functional Assessment of Chronic Illness Therapy-Fatigue (FACIT-F)
The FACIT-F is a well-validated quality-of-life instrument widely used for the assessment of cancer-related fatigue in clinical trials. It consists of 27 general quality-of-life questions divided into 4 domains (physical, social, emotional, and functional), plus a 13-item fatigue subscore. The patient rates the intensity of fatigue and its related symptoms on a scale of 0–4. The total score ranged between 0 and 52, with higher scores denoting less fatigue. According to the scoring manual, the negatively worded items on the FACIT-F are reverse-scored so that the higher scores indicate more positive health states [19].
-
3.
Cachexia was assessed by the 12-item Functional Assessment of Anorexia/Cachexia Therapy (FAACT) subscale questionnaire. This version has been validated in patients with advanced cancer [20].
-
4.
Depression was assessed using the 14-item Hospital Anxiety and Depression (HADS) questionnaire [21]. This questionnaire has been validated in a number of clinical situations and has been widely used in medically ill patients. Only the depression subscale was used in the analyses for this study.
-
5.
Sexual Desire Inventory (SDI-2) is a self-report questionnaire that assesses sexual desire independent of engaging in actual sexual activity [22]. It contains items that measure desire with a partner (dyadic items 1–9; maximal score, 79) and in solitary situations (items 10–14; maximal score, 44). Higher scores indicate greater desire.
-
6.
The International Prostatic Symptom Score (IPSS) is a validated, eight-item scale that assesses urinary tract problems such as urinary frequency, urgency, and stream [23]. Patients were assessed at each clinic visit and if scores fell in the severe range (>19) at any assessment point, participants were withdrawn from the study.
-
7.
Body composition was be measured by bioimpedance (BIA). BIA is a noninvasive method of estimating body composition based on the ability of lean tissue to conduct an electrical current better than fat. The Tanita TBF-310 (Tanita, Tokyo, Japan) body composition analyzer/scale was used to measure total body water, total body fat, and total body lean mass.
-
8.
Measurements of strength and stamina included the 6-min walk, the Get-up-and-Go test, and Handgrip dynamometry. The 6-min walk has been recommended by the American Thoracic Society (ATS) as an objective measure of functional capacity [24]. Further evaluation of physical performance was performed using the Timed Get-Up-and-Go test [25] and Handgrip strength with a Jamar dynamometer.
-
9.
Bioavailable testosterone levels were measured by ammonium precipitation method at the Mayo Clinic, Rochester, Minnesota. The method is based on the differential precipitation of sex hormone binding globulin (SHBG) by ammonium sulfate following equilibration of the serum specimen and tracer amounts of tritium-labeled testosterone. The results are expressed as the percent of testosterone free or albumin bound (not precipitated with SHBG) compared to an albumin standard. The product of this percentage and the total testosterone measurement is the total bioavailable testosterone [26].
-
10.
Performance status was determined by the Eastern Cooperative Oncology Group (ECOG) Performance Status scale [27].
Statistical analysis
The primary objective was to determine whether the average decrease in fatigue from baseline to day 29 in patients who received testosterone replacement is greater than those who received placebo as measured by the FACIT-F and FACIT-fatigue subscale. A one-sided t test was used to analyze differences in FACIT scores and domain scores between arms because testosterone was not expected to worsen symptoms. Other variables were analyzed using similar methods. For primary analyses to compare difference scores between the two groups, a two-sample t test was used for analysis of change in symptoms, sexual desire scores, ECOG, HADS, body composition by bioelectrical impedance (BIA), and physical performance measured by 6-min walk and get-up-and-go tests. Pearson correlation was used to measure the relationship between change in testosterone levels and clinical outcomes after day 29.
Fifty evaluable patients per group would have allowed us to detect a difference between groups of approximately one half of a standard deviation assuming a one-sided significance level of 0.05 and 80 % power. We expected to enroll 80 patients at M. D. Anderson Cancer Center and 46 patients at VA; only 43 patients are reported in this study.
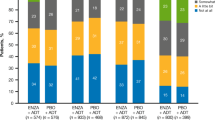
Results
Of the 48 subjects that met our criteria, 19 were randomized to testosterone and 24 to placebo. Seventy-seven percent were from MD Anderson Cancer Center (MDACC) and 23 % from the (VA) (Fig. 1). Patients declined to participate because of concerns about frequent hospital visits (every 2 weeks), testosterone side-effects, and also the possibility of receiving a placebo intramuscular injection. Once enrolled, only three subjects in the placebo arm and five in the testosterone arm stopped treatment before day 29.The frequent two weekly follow-ups and difficulty with transport to the hospitals were cited as reasons for discontinuing therapy. One subject died in the testosterone arm and this was considered unrelated to the treatment. While no significant difference was noted in age or other baseline measurements (Table 1), there were more black patients in the placebo group (6/16 vs.1/13, p = 0.04).
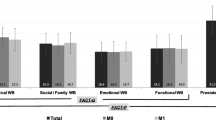
After 29 days of treatment, no statistically significant differences in FACIT-fatigue subscale scores were found between arms using a one-sided t test, although differences were in the expected direction (−2 ± 12 for placebo, 4 ± 8 for testosterone, p = 0.11) (Table 2). Similar results were found for the FACIT-F total score with a trend for testosterone to improve scores (−4 ± 20 for placebo, 4 ± 14 for testosterone, p = 0.14). A one-sided t test was used to analyze the primary outcome, since we expected an improvement in the testosterone group. The domain of emotional well-being (p = 0.007) was significantly better in the testosterone group (Table 2), while Sexual Desire Inventory scores (p = 0.054) approached significance (Table 3). The other domains of physical and functional well-being showed no difference; however, social well-being was worse in the testosterone arm (p = 0.03). After 29 days, the difference in testosterone levels between the placebo and replacement groups trended towards significance (Table 3). Pearson correlation showed significant associations between the testosterone level rise after 29 days and better FACIT-F (r = 0.812, p = 0.049) and FACIT-fatigue (r = 0.878, p = 0.021) scores (Table 4).
There was no difference in survival (p = 0.50) between groups. Adverse events, including IPSS scores were similar between groups. There were no significant differences in the secondary outcomes measured by The Hospital Anxiety and Depression Scale or symptoms scored by the ESAS, including appetite, dyspnea, insomnia, well-being, anxiety, depression, nausea, fatigue, pain and drowsiness. Improvement in ECOG performance status was a secondary outcome, but all participants required an ECOG status <3 per inclusion criteria. Both groups had a majority of patients with a baseline ECOG performance status in the 1–2 range, although more patients in the placebo group had a PS of 0 (7 vs.1) .This difference was not statistically significant (p = 0.12). ECOG status improved (p = 0.02) only in participants receiving testosterone. Handgrip by dynamometry, get-up-and-go test, and 6-min walk were not significantly different between the two groups after 4 weeks (Table 3). After 72 days of treatment, fatigue subscale scores were significantly better in the testosterone group (p = 0.03) (Table 2); however, this was not accompanied by an improved performance status or symptom scores. There were no differences in hemoglobin levels between the groups at baseline, day 29 or 72 (Table 5).
Discussion
The results of the quality of life questionnaires (FACIT-F and FACIT-fatigue) show a trend towards benefit from testosterone replacement in hypogonadal men with cancer. Although not statistically significant, the improvement of the FACIT-F in the testosterone arm may be clinically meaningful. Studies of the FACIT-F instrument have identified a minimally important difference (MID) in score. This difference in score is perceived by patients as clinically important. Scores improved by 4 for both FACIT-F and FACIT-fatigue scales after testosterone replacement, in contrast to declines in the placebo group. A change of 4 points is within the range considered to be a MID [28–31]; however, since the study was underpowered, no statistically significant difference was found. Other aspects of quality of life also showed improvement. The emotional well-being domain improved significantly and sexual desire scores approached significance, suggesting that testosterone replacement may have important benefits for aspects of intimacy and sense of self in men with advanced cancer. Sexual desire decreases with age in cross-sectional studies of healthy men and women, although ill health may exacerbate this sexual decline particularly in men [32]. There was an unexpected decline in social well-being at day 29 which is difficult to explain but could be a spurious result given the number of outcomes measured.
We had decided to use a one-sided t test a priori and assumed fatigue would not worsen with testosterone treatment. Although the trend towards improved quality of life is in the expected direction, our use of the one-sided t test may be regarded as a limitation given that one of the components of the FACIT-F (social well-being) worsened with treatment. The absence of any accompanying symptom improvement as measured by the ESAS is surprising. Prior retrospective studies from our group and others showed correlations between low testosterone levels and symptoms of appetite [33], insomnia, dyspnea [4], and fatigue [1, 34] in male patients with cancer. Explanations for the lack of symptom benefit may include the small sample size of our study or relatively insufficient testosterone replacement doses. Larger increases in testosterone levels from baseline were associated with better FACIT-F and FACIT-fatigue subscale scores (Table 4). After 4 weeks of replacement, however, the testosterone levels between the two arms were only trending towards significance (p = 0.08). In order to obtain a steady state level at 4 weeks, other routes of administration or testosterone injections at weekly levels might be required for the first 3 few weeks of treatment. By day 72, the fatigue subscale did improve significantly, indicating that patients could derive greater benefit with the prolonged use of testosterone and successful dose titration. It should be noted however that the fatigue score at day 72 was not our primary outcome. There were no changes in hemoglobin levels, which suggests that the benefits were due to effects of testosterone replacement other than bone marrow stimulation [35].
Our study has several limitations. Some of the enrolled patients may have had anemia contributing to their fatigue, since our hemoglobin cut-off was >9 g/dL. However, the association between hemoglobin levels and fatigue in patients with metastatic or locally advanced cancer is inconsistent. At least one study has suggested that anemia is not a major contributor to fatigue in patients with cancer receiving palliative care and that even hemoglobin levels above 12 g/dL are associated with high fatigue scores (6/10 on ESAS) [36]. Others have shown an association between severe fatigue and hemoglobin levels [37] and an improvement in symptoms when patients are transfused with a baseline hemoglobin of approximately 8 g/dL [38]. The benefits on dyspnea and fatigue after transfusion tended to decrease within 15 days, despite the maintenance of hemoglobin values, suggesting that other mechanisms of fatigue play a role. Our cut-off for hemoglobin was based on these studies and our institutional guidelines which discouraged transfusions for patients with hemoglobin levels >9 g/dL.
The lack of functional improvement or gains in fat-free mass is not entirely unexpected since most studies with testosterone replacement have measured these outcomes after several months. Also, our measure of body composition by bioimpedance was limited, and dual-energy X-ray absorptiometry (DEXA) [39] or computed tomography (CTscan) [40] would have been preferable to measure lean body mass outcomes. Unfortunately, our resources were limited so DEXA scans were not feasible and most of our patients had advanced cancer and were no longer undergoing routine CT scan.
Accrual was slower than expected for a number of reasons and any conclusions of the study should be interpreted with caution since the sample size was smaller than needed. The follow-up visits at two weekly intervals were burdensome for many patients, especially those from out of state. Others were reluctant to enroll in a placebo-controlled trial while public awareness campaigns and direct to consumer advertising [41] strongly asserted the advantages of testosterone replacement. A number of our patients declined to participate because they regarded the intramuscular injection as too painful and requested an alternate route of administration. Future studies may need to consider other routes of administration such as transdermal, in order to increase patient acceptability. We elected to use intramuscular testosterone because of its proven safety, low cost, and good adherence. In long-term studies, compliance with dosing exceeds 90 %. Randomized trials of intramuscular testosterone in hypogonadal males [42] demonstrate that it is well tolerated [43]. In our study, the adverse effects and toxicity in the testosterone group were similar to placebo, and the dropout rate of eligible patients was consistent with expected rates for patients with advanced cancer.
Conclusion
In hypogonadal males with advanced cancer, 4 weeks of testosterone replacement did not significantly improve quality of life measured by the FACIT-F. There was a trend for increased sexual desire and after 72 days of testosterone therapy, fatigue scores showed significant improvement. Larger studies of longer duration are warranted before routine testosterone replacement can be recommended.
References
Strasser F, Palmer JL, Schover LR et al (2006) The impact of hypogonadism and autonomic dysfunction on fatigue, emotional function, and sexual desire in male patients with advanced cancer: a pilot study. Cancer 107:2949–2957
Burney BO, Hayes TG, Smiechowska J et al (2012) Low testosterone levels and increased inflammatory markers in patients with cancer and relationship with cachexia. J Clin Endocrinol Metab 97:700–709
Chlebowski RT, Heber D (1982) Hypogonadism in male patients with metastatic cancer prior to chemotherapy. Cancer Res 42:2495–2498
Del Fabbro E, Hui D, Nooruddin ZI et al (2010) Associations among hypogonadism, C-reactive protein, symptom burden, and survival in male cancer patients with cachexia: a preliminary report. J Pain Symptom Manag 39:1016–1024
Rabkin JG, Wagner GJ, Rabkin R (2000) A double-blind, placebo-controlled trial of testosterone therapy for HIV-positive men with hypogonadal symptoms. Arch Gen Psychiatry 57:141–147
Patrick DL, Ferketich SL, Frame PS et al (2004) National Institutes of Health State-of-the-Science Conference Statement: Symptom management in cancer: pain, depression, and fatigue, July 15–17, 2002. National Institutes of Health State-of-the-Science Panel. J Natl Cancer Inst Monogr 32:9–16
Bhasin S, Cunningham GR, Hayes FJ et al (2006) Testosterone therapy in adult men with androgen deficiency syndromes: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 91:1995–2010
Garcia JM, Li H, Mann D, Epner D et al (2006) Hypogonadism in male patients with cancer. Cancer 106:2583–2591
Rajagopal A, Vassilopoulou-Sellin R, Palmer JL, Kaur G, Bruera E (2004) Symptomatic hypogonadism in male survivors of cancer with chronic exposure to opioids. Cancer 100:851–858
Gerl A, Muhlbayer D, Hansmann G, Mraz W, Hiddemann W (2001) The impact of chemotherapy on Leydig cell function in long term survivors of germ cell tumors. Cancer 91:1297–1303
Dev R, Del Fabbro E, Bruera E (2007) Association between megestrol acetate treatment and symptomatic adrenal insufficiency with hypogonadism in male patients with cancer. Cancer 110:1173–1177
Malkin CJ, Pugh PJ, Morris PD, Kerry KE, Jones RD, Jones TH, Channer KS (2004) Testosterone replacement in hypogonadal men with angina improves ischaemic threshold and quality of life. Heart 90:871–878
Chiang HS, Cho SL, Lin YC, Hwang TI (2009) Testosterone gel monotherapy improves sexual function of hypogonadal men mainly through restoring erection: evaluation by IIEF score. Urology 73:762–766
Cherrier MM, Asthana S, Plymate S, Baker L, Matsumoto AM, Peskind E, Raskind MA, Brodkin K, Bremner W, Petrova A, LaTendresse S, Craft S (2001) Testosterone supplementation improves spatial and verbal memory in healthy older men. Neurology 57:80–88
Bhasin S, Storer TW, Javanbakht M, Berman N, Yarasheski KE, Phillips J, Dike M, Sinha-Hikim I, Shen R, Hays RD, Beall G (2000) Testosterone replacement and resistance exercise in HIV-infected men with weight loss and low testosterone levels. JAMA 283:763–770
Morley JE, Charlton E, Patrick P, Kaiser FE, Cadeau P, McCready D, Perry HM (2000) Validation of a screening questionnaire for androgen deficiency in aging males. Metabolism 49:1239–1242
Bruera E, Kuehn N, Miller MJ et al (1991) The Edmonton Symptom Assessment System (ESAS). J Palliat Care 7:6–9
Chang VT, Hwang SS, Feuerman M (2000) Validation of the Edmonton Symptom Assessment Scale. Cancer 88:2164–2171
Cella D, Tulsky DS, Gray G et al (1993) The functional assessment of cancer therapy scale: development and validation of the general measure. J Clin Oncol 11:570–579
Ribaudo JM, Cella D, Hahn EA, Lloyd SR, Tchekmedyian NS et al (2000) Re-validation and shortening of the Functional Assessment of Anorexia/Cachexia Therapy (FAACT) questionnaire. Qual Life Res 9:1137–1146
Johnston M, Pollard B, Hennessey P (2000) Construct validation of the hospital anxiety and depression scale with clinical populations. J Psychosomatic Res 48:579–584
Spector IP, Carey MP, Steinberg L (1996) The Sexual Desire Inventory: development, factor structure, and evidence of reliability. J Sex Marital Ther 22:175–190
Barry MJ, Fowler FJ Jr, O'Leary MP, Bruskewitz RC et al (1992) for The Measurement Committee of the American Urological Association, The American Urological Association symptom index for benign prostatic hyperplasia. J Urol 148:1549–1557
American Thoracic Society (2002) ATS Statement: Guidelines for the Six-Minute Walk Test. Am J Respir Crit Care Med 166:111–117
Sousa N, Sampaio J (2005) Effects of progressive strength training on the performance of the Functional Reach Test and the Timed Get-Up-and-Go Test. Am J Hum Biol 17:746–751
Wheeler MJ (1995) The determination of bioavailable testosterone. Ann Clin Biochem 32:345–357
Oken MM, Creech RH, Tormey DC et al (1982) Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J ClinOncol 5:649–655
Lai JS, Beaumont JL, Ogale S, Brunetta P, Cella D (2011) Validation of the functional assessment of chronic illness therapy-fatigue scale in patients with moderately to severely active systemic lupus erythematosus, participating in a clinical trial. J Rheumatol 38:672–679
Cella D, Hahn EA, Dineen K (2002) Meaningful change in cancerspecific quality of life scores: differences between improvement and worsening. Qual Life Res 11:207–221
Yost KJ, Sorensen MV, Hahn EA, Glendenning GA, Gnanasakthy A, Cella D (2005) Using multiple anchor- and distribution-based estimates to evaluate clinically meaningful change on the Functional Assessment of Cancer Therapy-Biologic Response Modifiers (FACT-BRM) instrument. Value Health 8:117–127
Cella D, Eton DT, Lai JS et al (2002) Combining anchor and distribution-based methods to derive minimal clinically important differences on the Functional Assessment ofCancer Therapy (FACT) Anemia and Fatigue scales. J PainSymptom Manage 24:547–561
Lindau ST, Gavrilova N (2010) Sex, health, and years of sexually active life gained due to good health: evidence from two US population based cross sectional surveys of ageing. BMJ 9:340–c810
Garcia JM, Li H, Mann D, Epner D, Hayes TG, Marcelli M, Cunningham GR (2006) Hypogonadism in male patients with cancer. Cancer 106:2583–2591
Shafqat A, Einhorn LH, Hanna N, Sledge GW, Hanna A, Juliar BE, Monahan P, Bhatia S (2005) Screening studies for fatigue and laboratory correlates in cancer patients undergoing treatment. Ann Oncol 16:1545–1550
Coviello AD, Kaplan B, Lakshman KM, Chen T, Singh AB, Bhasin S (2008) Effects of graded doses of testosterone on erythropoiesis in healthy young and older men. J Clin Endocrinol Metab 93:914–919
Munch TN, Zhang T, Willey J, Palmer JL, Bruera E (2005) The association between anemia and fatigue in patients with advanced cancer receiving palliative care. J Palliat Med 8:1144–1149
Minton O, Strasser F, Radbruch L, Stone P (2012) Identification of factors associated with fatigue in advanced cancer: a subset analysis of the European palliative care research collaborative computerized symptom assessment data set. J Pain Symptom Manage 43(2):226–235
Mercadante S, Ferrera P, Villari P, David F, Giarratano A, Riina S (2009) Effects of red blood cell transfusion on anemia-related symptoms in patients with cancer. J Palliat Med 12:60–63
Trutschnigg B, Kilgour RD, Reinglas J, Rosenthall L, Hornby L, Morais JA, Vigano A (2008) Precision and reliability of strength (Jamar vs. Biodex handgrip) and body composition (dual-energy X-ray absorptiometry vs. bioimpedance analysis) measurements in advanced cancer patients. Appl Physiol Nutr Metab 33:1232–1239
MacDonald AJ, Greig CA, Baracos V (2011) The advantages and limitations of cross-sectional body composition analysis. Curr Opin Support Palliat Care 5:342–349
Eggertson L (2011) Brouhaha erupts over testosterone-testing advertising campaign. CMAJ 183:1161–1162
Marks LS, Mazer NA, Mostaghel E et al (2006) Effect of testosterone replacement therapy on prostate tissue in men with late-onset hypogonadism: a randomized controlled trial. JAMA 296:2351–2361
Rhoden EL, Morgentaler A (2003) Testosterone replacement therapy in hypogonadal men at high risk for prostate cancer: results of 1 year of treatment in men with prostatic intraepithelial neoplasia. J Urol 170:2348–2351
Acknowledgments
Funding
This work was supported by a grant from the American Cancer Society# PEP-08-299-01-PC1 to E. Del Fabbro.
E. Bruera is supported in part by a National Institutes of Health grant numbers RO1NR010162-01A1, RO1CA1222292.01, and RO1CA124481-01.
J. Garcia is supported in part by the Dept of Veterans Affairs MERIT grants (I01-BX000507 and I01 CX000174) and the NIA (T32AG000183 and AG040583).
D. Hui is supported in part by the Clinician Investigator Program, Royal College of Physicians and Surgeons of Canada.
Disclosure
The authors have declared no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
E. Del Fabbro and J.M Garcia contributed equally to this work.
Rights and permissions
About this article
Cite this article
Del Fabbro, E., Garcia, J.M., Dev, R. et al. Testosterone replacement for fatigue in hypogonadal ambulatory males with advanced cancer: a preliminary double-blind placebo-controlled trial. Support Care Cancer 21, 2599–2607 (2013). https://doi.org/10.1007/s00520-013-1832-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-013-1832-5