Abstract
Goal of work
Aim of the present observational study is to focus on health-related quality of life (HRQL), mood and everyday life of breast cancer affected women disease-free 6 months after mastectomy, paying particular attention to the International Classification of Functioning, Disability and Health (ICF) framework contribution.
Materials and methods
Sixty-five breast cancer-affected women disease-free 6 months after mastectomy hospitalized for reconstructive surgery (mean age 46.3 ± 7.3) were enrolled. Their depressive symptoms (Beck Depression Inventory—BDI-II), HRQL, and every day life functioning/barriers and facilitators (ICF) were assessed.
Results
At the BDI-II, 6 patients (9.2 %) reported mild depression and 6 (9.2 %) severe depression; when the subscales were considered, 7 (10.8%) resulted depressed at the somatic–affective factor and 16 (24.6 %) at the cognitive factor. Compared to normative data no differences emerged at the HRQL Physical Component Summary (46.4 ± 9.3 vs 49.1 ± 10.1), whereas patients reported lower scores at the Mental HRQL Component Summary (45.9 ± 10.1 vs 51.5 ± 9.1; p = 0.00001 t = −4.3). As for the activity and participation domain, 11 of the 42 categories investigated were compromised in at least 20% of the sample: lifting and carrying objects (d430), acquisition of goods and services (d620), doing housework (d640), remunerative employment (d850), and many categories relating to interpersonal relationships; moreover the caregiver seems to be perceived as an important and positive modulator of disability.
Conclusions
The addition of the ICF evaluation to the usual psychological assessment gives a more complete picture, enabling a broader perspective of the psychological–clinical implications. Mainly, the women that we have evaluated continue to function in their everyday lives, thanks in part to their ability to accept help from their own families. However, they inevitably carry signs of their disease which some translating into problems with interpersonal relationships, depressive thoughts and negative ideation. Only the synergistic use of all these assessment instruments can one truly perceive all the nuances relating to the social and psychological conditions of the assessed patients’ life, overcoming a binomial vision of well-being and ill-being.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the second most common cancer worldwide and, according to the World Health Organization (WHO), the most common cancer in women. Every year, more than one million women are diagnosed with the disease, corresponding to 23 % of all cancer cases in women and 10 % of new cancer cases [35]. In 2002, there were 1.15 million new cases of breast cancer and approximately 4.4 million women, diagnosed with the disease in the previous 5 years, were still alive [21]. As a result of advances in treatment, including the combined use of surgery, radiation therapy, and chemotherapy, cancer survivor rates have increased by 50 % [6]. Nevertheless, breast cancer is associated with a wide range of functional and emotional impairments which has a profound psychosocial impact.
The spectrum of psychiatric disorders and psychological distress in cancer sufferers has been assessed over many years and in various studies. Anxiety, depression, energy loss, fatigue, and sleeping problems are common responses to stressors [10, 27]. The prevalence of depression among women with early diagnosed breast cancer is twice as high as that found in the general female population, especially during the first year after diagnosis [8]. However, major depression and depressive symptoms are underrated and undertreated in women with breast cancer [28]. Failure to diagnose mood disorders may cause problems as depression and its associated symptoms lower health-related quality of life (HRQL), affect compliance with medical therapies and could contribute to a reduced survival rate. The latter is due to the fact that depression may affect interpersonal relationships, occupational performance, stress, and perceptions of health and physical symptoms. Many studies have found that depression is correlated with a lower HRQL [25], but few studies have concentrated specifically on long-term HRQL in disease-free breast cancer survivors. These patients seem to have a good HRQL, less affected by the type of treatment than by their demographic characteristics, elapsed time since surgery, comorbidity, fatigue, and depression [1].
Bearing in mind the effect of breast cancer treatment on a patient’s HRQL is a central clinical and research issue. HRQL assessment generally refers to a number of domains including physical functioning, psychological well-being (such as level of anxiety and depression), and social support. Based on a review by Peery and colleagues, HRQL instruments were identified as being the most widely used assessment tools within the breast cancer population. Because of the complexity of breast cancer and the heterogeneity of the patients affected, no single instrument is both comprehensive and sensitive enough to perceive clinically meaningful changes in all outcomes across all phases of care [22]. Knowing patients’ subjective experience of physical and mental health, functioning in daily living, participation in social networks and general sense of well-being have become important factors in cancer patients’ evaluation.
The International Classification of Functioning, Disability and Health (ICF) framework provided a new perspective for the assessment of a patient’s disability, and the potential benefit of the synergism between the ICF evaluation and HRQL in terms of quality of care, evaluation of needs and optimisation of resource use has been underscored [9, 11, 18]. In fact, the ICF [2, 7, 9, 20, 34] has ratified the importance of a broad vision of a person’s life, picking up, describing, and classifying a person’s health condition with respect to the individual and society and not only with respect to the functional profile or the subjective perception of well-being [12]. In fact, the ICF describes disability as the result of interactions between the individual, society, and the environment in terms of both barriers and facilitators.
Some studies are now available on the implementation of the ICF in cancer [2, 29, 30] and in palliative care of patients with advanced stages of cancer [12] but only few have focused on women with breast cancer [7, 14, 31] and on women who have had breast cancer but are currently disease-free [35].
The aim of the present observational study was to focus on HRQL, mood, and everyday life of women with breast cancer who had been disease-free for at least 6 months after mastectomy, paying particular attention to the contribution made by the ICF.
Method
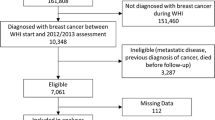
Procedure and study population
From May 2008 to November 2010 all women at the Breast Surgery Unit who had undergone primary curative surgery for breast cancer and hospitalized for reconstructive surgery were consecutively enrolled. Women were eligible to participate if they had had a past diagnosis of breast cancer, were on no current cancer therapy other than tamoxifen, were currently free of the disease, and had no other history of cancer. Exclusion criteria were: cognitive deficits interfering with language and reasoning, psychiatric or severe psychological disorders prior to the disease onset, and other relevant clinical conditions.
Overall, 65 consecutive in-patients were enrolled into the study. There were no refusals to participate, probably because psychological assessment is part of routine clinical work and psychologists are usually accepted well by both patients and relatives.
The study was approved by the institute’s ethics committee and all patients signed an informed medical consent form.
Instruments
During the first week of admission, patients were administered the following:
-
A socio-demographic and perceived health status schedule: assessing socio-demographic and clinical characteristics, and perceived health status (subjective evaluation of mental and physical health on a five-point Likert scale). The questionnaire consisted of 15 questions and had been appropriately developed by our study team.
-
Beck Depression Inventory II (BDI II) [4]: a 21-item rating scale to assess the presence and prominence of depressive symptoms which reflects the diagnostic criteria of the Diagnostic and Statistical Manual for Mental Disorders—Fourth Edition. It identifies a total score and two factors (Somatic-Affective and Cognitive). Raw scores (range 0–63) can be transformed into percentile scores when compared to the Italian normative sample (<85th percentile, no depression; 85th–90th percentile, mild depression; 91st–95th percentile, moderate depression; >95th percentile, severe depression). BDI-II has already been used with cancer patients [23].
-
Short-Form Health Survey-12 (SF-12) [33]: a HRQL instrument based on the reputable 36-item Short-Form Health survey (SF-36) [32]. Two synthetic scores are available: Physical Component Summary (PCS) and Mental Component Summary (MCS) (range 0–100; lower scores representing greater functional impairment).
-
ICF Checklist [20, 34]: a user–friendly display of the most relevant ICF categories for clinical purposes in order to record information regarding an individual’s functioning and disability. In this study only the “Activity and Participation” and the “Environmental Factors” domains were taken into consideration. Activity is the execution of a task or action by an individual whereas Participation is a person’s involvement in a real-life situation; it represents the societal perspective of functioning. The Environmental Factors refer to all aspects globally—both barriers and facilitators—of the external or extrinsic world that form the context of an individual’s life and, as such, have an impact on that person’s functioning.
As to the activity and participation domain, activity limitations and participation restrictions were assessed by means of two qualificators: (1) “performance with equipment aids only”—considering only the help provided by equipment and instrumental aids; and (2) “performance with equipment aids and with other’s assistance”—considering both the help provided by equipment and instrumental aids and the help provided by family members, friends, and other people. The qualificators range from 0 (no activity limitation nor participation restriction) to 4 (maximum activity limitation or participation restriction). In this study, the delta values originating from the difference between activity and participation categories together with equipment aids only and activity and participation categories with equipment aids along with a person’s help were also considered. Delta values provided information about the caregiver’s impact: a delta value = 0 neutral caregiver role, a delta value ≥1 caregiver as a positive disability modulator (facilitator), while a delta value <0 caregiver as a negative disability modulator (barrier) [12].
With regard to the environmental factors domain, the qualifier, in a range of 0–4, can be used to denote the extent of positive effects (facilitator—positive values) or the negative effects (barrier—negative values) of the environment.
All questionnaires and tools were administered in their Italian-validated versions [3, 5, 20]. Women self compiled the socio-demographic and perceived health status schedule, BDI-II and SF-12; the ICF checklist was completed during an interview carried by trained psychologists.
Statistical analyses
Descriptive analyses were performed on the socio-demographic data and depression (BDI-II) and QoL (SF-12) scores. The SF-12 scores were compared to normative data by means of a t test for independent variables. P was set at 0.01.
As for the ICF classification, a descriptive analysis, mode, and median of the ICF Activity and Participation delta values and chapters e3 and e4 of the environmental factors was calculated. All qualifiers, 8 (not specified) and 9 (not applicable), were considered as missing data. Statistical analyses were performed using SPSS 11.0.
Results
Table 1 represents the socio-demographic and clinical characteristics, and data regarding perceived health status. The mean age of the women considered was 46.3 ± 7.3 years. All patients did not change their marital status after the cancer diagnosis and each of them had at least one clearly identified caregiver (mainly partner and/or daughter/son).
The mean score of the BDI-II total score was 8.6 ± 6.0 (somatic–affective factor 6.1 ± 3.8 and cognitive factor 2.5 ± 3.0). As for the percentile scores, 6 patients (9.2 %) reported mild depression and 6 (9.2 %) severe depression; when the subscales were considered, 7 patients resulted depressed as regards the somatic–affective factor (3.1 % mild, 3.1 % moderate, and 4.6 % severe) and 16 resulted depressed as regards the cognitive factor (4.6 % mild, 4.6 % moderate, and 15.4 % severe).
The SF-12 showed no differences between the study subjects and a normative sample with regards to PCS (46.4 ± 9.3 vs 49.1 ± 10.1) indicating that physical health-related quality of life among respondents was as the general population; whereas patients reported lower scores for the MCS (45.9 ± 10.1 vs 51.5 ± 9.1; p = 0.00001, t = −4.3) showing a slightly lower mental HRQL than that of the general population.
As far as the activity and participation domain is concerned, 11 out of the 42 categories investigated were compromised in at least 20 % of the samples: lifting and carrying objects (d430), acquisition of goods and services (d620), doing housework (d640), remunerative employment (d850) (Table 2). Moreover, women report a significant perceived disability in the area relating to interpersonal relationships, both formal and informal, mainly with family members. Finally, also the intimate relationship with their significant other resulted impaired.
The caregiver was perceived as holding a neutral role or as a facilitator; in none of the domains resulted to be a barrier. Table 3 shows ICF activity and participation categories with the median of delta values ≥1 (caregiver as a facilitator) and delta values distribution.
Table 4 shows frequencies and percentages of ICF environmental factors qualificators. Many domains are perceived neither as a barrier nor as a facilitator. Products or substances for personal consumption are perceived as facilitators: patients mainly refer to cancer therapy availability in Italy. Also, health and social security services, systems, and policies are considered as reducing disability. All people with an informal connection with the women assessed (family, friends and acquaintances) and the healthcare team, and their attitudes, are often perceived as facilitators, positively modulating the patient’s perceived disability.
Discussion
The data from the BDI-II show that our patients had a fairly substantial level of depressive symptoms: although this was a sample of mastectomized women who were currently free of disease, 18.4 % of the patients had depression scores above the norm. Subscale analysis enabled more precise and better definition of the nature of the symptoms: 24.6 % of the sample had compromised cognitive features of depression (pessimism, sense of guilt, low self-esteem), while the somatic-affective sphere was compromised in only 10.8 % of the case study (loss of interest, loss of energy, sleep disorders, changes in appetite, restlessness, crying). The depressive symptoms were, therefore, related mainly to a redefinition of self and the history of the disease, in the context of which the patient must find room both to rebuild her own female identity and to create a new view of the future and expectations.
In concordance with the data from the BDI-II, the data from the SF-12, compared with scores obtained from normal groups, showed a reduction in perceived mental health, while the perceived state of physical health did not seem to be compromised. Indeed, the patients reported a certain psychological distress and consequent social and personal disability due to problems relating to the emotional sphere.
Similarly, at a qualitative level, the responses concerning perception of one’s own physical and mental health, mirrored those from the SF-12: 83.1 % of the women in our sample reported good/very good physical health, but only 67.7 % reported good/very good mental health.
The data derived from using the ICF Checklist could be used to describe the disability perceived by the women in the sample, taking into account the impact the disease had on the women’s life in more detail.
As far as the activity and participation domain is concerned, 11 out of the 42 categories investigated were compromised and concerned activities such as lifting and carrying objects (d430), acquisition of goods and services (d620), doing housework (d640), remunerative employment (d850), and interpersonal relationships. In the first three categories, the differences between capacity and performance highlight the facilitating role of environmental factors: treatments, together with family and social support, are helpful at an everyday activities and participation level. In our sample, in particular, the caregiver seems to play an important modulator role of the disability: the presence of a caregiver enables the patient to function well in everyday life, even with regards to those activities which could otherwise be affected by the disease.
The data relating to environmental factors confirm the foregoing. The number of categories of this component reveals the extensive involvement of contextual factors in the effective management of our patients. Women regard support and relationships (e3) and attitudes (e4) of family, friends, and health professionals as well as social and healthcare services and policies (e5) to be of great importance and support.
Consistent with results from the psychosocial literature on breast cancer, the level of independence in performing activities, the importance of positive relations and the amount of social support is assumed to be major factors in psychosocial adjustment and to influence patients’ health final outcomes [16, 17, 24].
Matching ICF-based information regarding impairments, activities, participation, and environmental factors with HRQL data, could provide useful information on service utilization. Healthcare services might use this information when planning support and care for the patients and their families.
Conclusions
The data regarding depressive symptoms and perceived disability, if evaluated independently, show an apparently contradictory picture: the patients evaluated, despite having symptoms of depression, do not report significant impairment in everyday life, thanks above all to the active and psychological help provided by caregivers. Cancer seems to be an occasion for reorganizing roles of the family unit [13]. This was found to be the case also in a study carried out on Arab women: the husbands of Arab breast cancer survivors were more involved in household chores than husbands of matched healthy women even several years after the oncology treatment [15].
The addition of the ICF evaluation to the usual psychological assessment gives a more complete picture, enabling a broader perspective of the psychological–clinical implications. The women that we have evaluated continue to function as normal in their everyday lives, thanks in part to their ability to accept help from their own families. However, they inevitably carry signs of their disease which some translate into problems with interpersonal relationships, depressive thoughts, and negative ideation, and are certainly a source of distress. It is, therefore, important not to underestimate the significance of depressive symptoms, even those occurring some time after the acute event. Only the synergistic use of all these assessment instruments can one truly detect all the nuances of the social and psychological conditions of the assessed patients’ life, overcoming a binomial vision of well-being and ill-being [19, 26].
The psychological intervention should not, therefore, be focused only on depressive features, but also on the reorganization of a female identity, related to both physical appearance and everyday life, as well as considering the active role of the family caregiver. The aim is, therefore, to guide patients towards a narration of self which can integrate the inevitably present psychological distress during active participation in life.
References
Ahn SH, Park BW, Noh DT, Nam SJ, Lee ES, Lee MK, Kim SH, Lee KM, Park SM, Yun YH (2007) Health-related quality of life in disease-free survivors of breast cancer with the general population. Annals of Oncology 18:173–182
Ajovalasit D, Vago C, Usilla A, Riva D, Fidani P, Serra A, Gentile S, Massimino M, Biassoni V, Leonardi M (2009) Use of ICF to describe functioning and disability in children with brain tumours. Disabil Rehabil 31(Suppl 1):S100–107
Apolone G, Mosconi P, Quattrociocchi L, Granicolo EAL, Groth N, Ware JE Jr (2001) Questionario sullo stato di salute SF-12, versione italiana. Guerini e Associati Editore, Milano
Beck AT, Steer RA, Brown GK (1996) Beck Depression Inventory, 2nd edn. The Psychological Corporation Harcourt Brace and Company, San Antonio, Manual
Ghisi M, Flebus GB, Montano A, Sanavio E, Sica C (eds) (2007) BDI-II manual. Giunti OS Organizzazioni Speciali, Firenze
Berry DA, Cronin KA, Plevritis SK, Fryback DG, Clarke L, Zelen M, Mandelblatt JS, Yakovlev AY, Habbema JD, Feuer EJ, Cancer Intervention and Surveillance Modeling Network (CISNET) Collaborators (2005) Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med 353:1784–1792
Brach M, Cieza A, Stucki G, Füssl M, Cole A, Ellerin B, Fialka-Moser V, Kostanjsek N, Melvin J (2004) ICF Core Sets for breast cancer. J Rehabil Med (44 Suppl):121–127
Burgess C, Cornelius V, Love S, Graham J, Richards M, Ramirez A (2005) Depression and anxiety in women with early breast cancer: five year observational cohort study. BMJ 330:702–705
Cieza A, Bickenbach J, Chatterji S (2008) The ICF as a conceptual platform to specify and discuss health and health-related concepts. Gesundheitswesen 70:e47–56
Dow KH, Ferrell BR, Leigh S, Ly J, Gulasekaram P (1996) An evaluation of quality of life among long term survivors of breast cancer. Breast Cancer Res Treat 39:261–273
Fayed N, Schiariti V, Bostan C, Cieza A, Klassen A (2011) Health status and QOL instruments used in childhood cancer research: deciphering conceptual content using World Health Organization definitions. Qual Life Res 20:1247–1258
Giardini A, Ferrari P, Majani G, Negri EM, Rossi S, Magnani C, Preti P (2010) International Classification of Functioning Disability and Health (ICF) e Qualità della Vita nel paziente oncologico in fase avanzata di malattia. G Ital Med Lav Ergon 32(3 Suppl B):B29–36
Giardini A, Giorgi I, Sguazzin C, Callegari S, Ferrari P, Preti P, Miotti D (2011) Knowledge and expectations of patients in palliative care: issues regarding communication with people affected by life-threatening diseases. G Ital Med Lav Ergon 33(1 Suppl A):A41–46
Glaessel A, Kirchberger I, Stucki G, Cieza A (2011) Does the comprehensive International Classification of Functioning, Disability and Health (ICF) Core Set for Breast Cancer capture the problems in functioning treated by physiotherapists in women with breast cancer? Physiotherapy 97:33–46
Goldblatt H, Cohen M, Azaiza F, Manassa R (2012) Being within or being between? The cultural context of Arab women’s experience of coping with breast cancer in Israel. Psycho-Oncology. doi:10.1002/pon.3078
Irvine D, Brown B, Crooks D, Roberts J, Browne G (1991) Psychosocial adjustment in women with breast cancer. Cancer 15:1097–1117
Lampic C, Thurfjell E, Bergh J, Carlsson M, Sjoden PO (2003) Atteinment and importance of life values among patients with primary breast cancer. Cancer Nurs 26:295–304
Lollar D (2002) Public health and disability: emerging opportunities. Public Health Rep 117:131–136
Majani G (2011) Positive psychology in psychological interventions in rehabilitation medicine. G Ital Med Lav Ergon 33(1 Suppl A):A64–68
OMS (2003) Classificazione Internazionale del Funzionamento, della Disabilità e della Salute (ICF) ICF Checklist. Edizioni Centro Studi Erickson, Trento
Parkin DM, Bray F, Ferlay J, Pisani P (2005) Global cancer statistics, 2002. CA Cancer J 55:74–108
Perry S, Kowalski T, Chang C (2007) Quality of life assessment in women with breast cancer: benefits, acceptability and utilization. Heath Qual Life Outcomes 5:24
Pezzilli R, Campana D, Morselli-Labate AM, Fabbri MC, Brocchi E, Tomassetti P (2009) Patient-reported outcomes in subjects with neuroendocrine tumors of the pancreas. World J Gastroenterol 15:5067–5073
Pistrang N, Barker C (1998) Partners and fellow patients: two sources of emotional support for women with breast cancer. Am J Community Psychol 26:439–456
Reich M, Lesur A, Pedrizet-chevallier C (2008) Depression, quality of life and breast cancer: a review of the literature. Breast Cancer Res Treat 110:9–17
Seligman MEP, Csikszentmihalyi M (2000) Positive psychology—an introduction. Am Psychol 55:5–14
Shimozuma K, Ganz PA, Petersen L, Hirji K (1999) Quality of life in the first year after breast cancer surgery: rehabilitation needs and patterns of recovery. Breast Cancer Res Treat 56:45–57
Somerset W, Stout SC, Miller AH, Musselman D (2004) Breast cancer and depression. Oncology 18:1021–1034
Tschiesner U, Linseisen E, Becker S, Mast G, Rogers SN, Walvekar RR, Berghaus A, Cieza A (2010) Content validation of the international classification of functioning, disability and health core sets for head and neck cancer: a multicentre study. J Otolaryngol Head Neck Surg 39:674–687
Tschiesner U, Oberhauser C, Cieza A (2011) ICF Core Set for head and neck cancer: do the categories discriminate among clinically relevant subgroups of patients? Int J Rehabil Res 34:121–130
Tsauo JY, Hung HC, Tsai HJ, Huang CS (2011) Can ICF model for patients with breast-cancer-related lymphedema predict quality of life? Support Care Cancer 19:599–604
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30:473–483
Ware JE, Kosinski M, Keller SD (1996) A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Medical care 34:220–233
World Health Organization (2001) ICF-International classification of functioning, disability and health. WHO Library, Geneva
World Health Organization (2009) World Cancer Report 2008. International Agency for Research on Cancer, Lyon
Acknowledgments
This research was conducted with the support of the Extraordinary National Cancer Program 2006 “ISS for ACC” Project, WP 2. QUALITA’ DI VITA E ICF IN PAZIENTI ONCOLOGICI.
Conflict of interest
The authors do not have conflicts of interest, have full control of all primary data, and allow the journal to review their data if requested.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Anna, G., Camilla, P., Ines, G. et al. ICF, quality of life, and depression in breast cancer: perceived disability in disease-free women 6 months after mastectomy. Support Care Cancer 21, 2453–2460 (2013). https://doi.org/10.1007/s00520-013-1794-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-013-1794-7