Abstract
Purpose
The purpose of this study is to compare the effects of anastrozole, letrozole and tamoxifen on radiation-induced pulmonary fibrosis.
Methods
Eighty female Wistar albino rats were divided into eight groups. Group (G) 1 was defined as control group. G2 was radiation therapy (RT) only group. Groups 3, 4 and 5 were tamoxifen, anastrozole and letrozole control groups respectively. Groups 6, 7 and 8 were RT plus tamoxifen, anastrozole and letrozole groups, respectively. A single dose of 12 Gy RT was given to both lungs. Tamoxifen, anastrozole and letrozole were started 1 week before the RT and continued until the animals were sacrificed 16 weeks after the RT. As an end point, the extent of pulmonary fibrosis for each rat was quantified with image analysis of histological sections of the lung. Kruskal–Wallis and Mann–Whitney U tests were used for statistical analyses.
Results
The congestion, inflammation and pulmonary fibrosis scores were significantly different between all the study groups (p values were <0.001 for each). When compared with RT only group, concomitant RT and tamoxifen group increased the radiation-induced pulmonary fibrosis (p = 0.005). However, using either anastrozole or letrozole with RT did not increase the radiation-induced pulmonary fibrosis (p values were 0.768 and 0.752, respectively).
Conclusion
Concomitant use of tamoxifen with RT seems to increase radiation-induced pulmonary toxicity. However, the use of both anastrozole and letrozole appears to be safe with concomitant RT, without increasing the risk of pulmonary fibrosis. This finding should be clarified with further clinical studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The lung is one of the most sensitive organs to ionizing radiation, and damage to normal lung tissue remains a major dose-limiting factor during irradiation of breast and thoracic tumors [1, 2]. Radiation-induced lung injury is a continuous process and regarded as the result of an abnormal healing response. It starts as an exudative inflammation, with the clinical picture of interstitial pneumonia 6–12 weeks after irradiation and proceeds to a productive chronic inflammation lasting several months and eventually terminating with scar formation which is known as lung fibrosis [3].
The alveolar epithelium consists of type I and type II epithelial cells. Type I cells cover approximately 90 % of the alveolar surface, and type II cells are the precursors of type I cells. In steady state, the turnover time of the alveolar epithelium is approximately 4–5 weeks. However after toxic injury, type I epithelial cells are denuded and the proliferation of type II cells is stimulated up to 10-fold [4]. Stimulation of type II cells promotes the secretion of growth factors and proteases and degradation of the extracellular matrix to allow removal of dead cells by normal process [3]. Pulmonary irradiation also reduces microvessel density and lung perfusion and promotes hypoxia [5]. All of these injuries stimulate the recruitment of a variety of inflammatory cells to the site of the injury, and it leads to establishment of chronic inflammation and fibrosis. In this phase vascular damage and collagen deposition become apparent. Vascular injury and activation of coagulation cascade, cellular adhesion molecules, proinflammatory and profibrotic cytokines and oxidative stress seem to play a vital role in the development of radiation fibrosis [6]. Transforming growth factor β (TGF-β) 1 plays an integral role in fibrosis formation by promoting the chemoattraction of fibroblasts and their conversion to myofibroblasts [1].
Adjuvant endocrine therapy has an important role in women with hormone receptor-positive (HR+) breast cancer. Tamoxifen which is a selective estrogen receptor modulator has been the gold standard of care for women with HR+ breast cancer for the last 30 years [7]. One nonhormonal effect of tamoxifen is the induction of TGF-β secretion. TGF-β has been implicated in the pathogenesis of radiation-induced fibrosis. There are many clinical and experimental studies evaluating the effect of tamoxifen on radiation-induced fibrosis [8–11]. The results demonstrated that when used concomitantly with radiotherapy, tamoxifen may increase induced pulmonary fibrosis.
Aromatase inhibitors (AIs) have now replaced tamoxifen as the standard of care for adjuvant endocrine therapy in the treatment of postmenopausal women (PMW) with hormone-sensitive breast cancer. AIs have more favorable tolerability profiles than tamoxifen. Most side effects are explained by the general estrogen deprivation, predictable and similar to those of natural menopause. Anastrozole and letrozole are well known third-generation reversible AIs. Although the pulmonary fibrosis of RT worsens when used with concurrent tamoxifen, there are no data regarding to pulmonary toxicities of AIs. In this experimental study, we aimed to evaluate whether there is any effect of AIs on the development of radiation-induced pulmonary fibrosis.
Methods and materials
Study design
The study included 80 adult female Wistar albino rats (250–300 g), the use of which was approved by the Selcuk University Animal Care and Use Committee. Animals were housed four per cage in a controlled animal holding room with a 12/12-h light/dark cycle; temperature and relative humidity were continually monitored to provide standard laboratory conditions. Food and water were provided ad libitum. Rats were divided into eight groups (G) composed of 10 animals. G1 was defined as control group, and rats of this group were sham irradiated. G2 was radiation therapy (RT) only group. Groups 3, 4 and 5 were tamoxifen, anastrozole and letrozole control groups, respectively. Groups 6, 7 and 8 were RT plus tamoxifen, anastrozole and letrozole groups, respectively (Table 1). Tamoxifen, anastrozole and letrozole were started 1 week before the RT and continued until the animals were sacrificed 16 weeks after the RT. As an end point, the extent of pulmonary congestion, inflammation and fibrosis for each rat were quantified with image analysis of histological sections of the lung.
Irradiation protocol
RT was applied under general anesthesia with intraperitoneally administered 90 mg/kg ketamine hydrochloride and 10 mg/kg xyalazine. A single dose of 12 Gy that has been shown to lead lung fibrosis [8] with 6-MV photon beams was applied via a single anterior field to 2 cm depth with SAD (source–axis distance) technique. One centimetre elasto-gel bolus was used to build up the radiation dose on the lungs and to provide contour regularity. The field size was 4 × 4 cm and included the both lungs.
Tamoxifen, anastrozole and letrozole protocols
Tamoxifen, anastrozole and letrozole doses which were equivalent to 20, 1 and 2.5 mg/kg adult doses, respectively, were calculated for each rat, and administered orally with a feeding tube once daily, including weekends, until the animals were sacrificed at the end of 16th week after the RT. In order to achieve adequate plasma concentration of the drugs, they were started 1 week before the RT administration.
Morphologic study and light microscopy
The animals were anesthetized and sacrificed by cervical dislocation 16 weeks after the start of irradiation. The lungs were excised and fixed in 10 % formaldehyde solution and embedded in paraffin for light microscopic examination. The slices obtained were stained with haematoxylin and eosin (H&E) to evaluate the inflammation, and with immunohistochemical triple staining to identify the fibrosis in the lung. Extent of the inflammation and congestion was graded on a scale of 0 (normal) to 3 (severe) as described in Table 2. Fibrosis was defined as the thickened alveolar walls with superimposed collagen. As a quantitive end point, extent of the radiation-induced fibrosis was graded on a scale of 0 (normal lung or minimal fibrous thickening) to 4 (total fibrous obliteration of the field) as described in Table 3 [12]. The pathologist was not aware of the treatment groups at the time of the histological examination of the specimens. After examining the whole sections for each rat, the average value was taken as the fibrosis score and mean values of the groups were calculated.
Statistical method
The Statistical Package for Social Sciences v. 13.0 was used for statistical analyses. As the pathological scores were ordinal in nature, the differences in pathological findings between the study groups were analyzed using the Kruskal–Wallis test. When an overall statistically significant difference was observed, pairwise comparisons were performed using the Mann–Whitney U test. Bonferroni correction was used for multiple comparisons. A 5 % type I error level was used for the statistical significance cutoff for overall comparisons.
Results
The median, minimum and maximum values of congestion, inflammation and pulmonary fibrosis scores were shown in Table 4. We found significant differences between all the study groups regarding to congestion, inflammation and pulmonary fibrosis scores with Kruskal–Wallis test (p values were <0.001 for each).
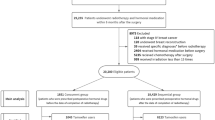
When we compared the RT control group, only the RT + tamoxifen group showed a significant difference in pulmonary fibrosis score (p = 0.005). However there were not any significant differences between the RT control group and RT + anastrozole and RT + letrozole groups (p values were 0.768 and 0.752, respectively; Table 5 and Fig. 1).
Immunohistochemical triple staining (×200): section from the lungs of the rats from a RT only group, b RT + tamoxifen group, c RT + anastrozole group, d RT + letrozole group. a There was thickening in the alveolar walls with intensive fibrosis. b There was thickening of the alveolar walls with massive fibrosis. There was total lung obliteration. c There was thickening in the alveolar walls with fibrosis. d There was thickening in the alveolar walls with fibrosis
At the histological examination, all of the rats of the RT groups had inflammation. Two rats from the RT + letrozole group had diffuse abscess formation. However there was not any statistically significant difference between the RT only group and RT + letrozole group regarding inflammation scores (p > 0.99). The inflammation scores significantly differed between the RT only and RT + tamoxifen (p = 0.005), RT + tamoxifen and RT + anastrozole (p = 0.001), and RT + tamoxifen and RT + letrozole (p = 0.005) groups (Table 5 and Fig. 2).
H&E staining (×200): section from the lungs of the rats from a control group, b RT only group, c tamoxifen only group, d anastrozole only group and e letrozole only group. a Normal lung. b There was thickening of the alveolar walls with severe inflammation and congestion. c There was minimal congestion in the alveolar walls. d Normal lung. e There was minimal congestion in the alveolar walls
In terms of the all parameters including pulmonary congestion, inflammation and fibrosis, there was not any significant difference between the control group and anastrozole only group (p values were 0.081, 0.374 and 0.615, respectively) and letrozole only group (p values were 0.067, 0.648 and 0.075, respectively). On the other hand, tamoxifen only group caused a significant difference in congestion score (p = 0.001). However using tamoxifen alone did not cause significant differences in pulmonary inflammation and fibrosis scores when compared to the control group (p = 0.374 and 0.028 for inflammation and fibrosis scores, respectively) (Table 6).
Discussion
The present study sought to compare the effects of tamoxifen and AIs on radiation-induced pulmonary toxicity. And our results revealed that concomitant use of tamoxifen with RT increased the radiation-induced pulmonary fibrosis; on the other hand, anastrozole and letrozole did not increased radiation-induced pulmonary fibrosis. The use of tamoxifen even without RT caused congestion when compared to the control and anastrozole only groups. Anastrozole and letrozole when used alone or with concomitant RT did not change histological findings.
The lung is one of the most radiosensitive organs, yet is frequently irradiated as a part of treatment programs for a variety of tumors in and around the thorax. Therefore pulmonary fibrosis is a well-known consequence of irradiation following the treatment of breast cancer, lung cancer and other mediastinal tumors. Adjuvant endocrine therapy has an important role in women with HR+ breast cancer. Efficacy of anti-hormonal treatment of early breast cancer is based on the fact that estrogens may stimulate the growth of residual cancer cells or contribute to the initiation of a new primary cancer over time.
The optimal sequencing of radiation and AIs as well as tamoxifen has not been established yet. Tamoxifen has no significant radiosensitizing properties; however, tamoxifen is a cytostatic drug that arrests cells in G1, a relatively radioresistant cell cycle phase [13]. Although some basic studies have demonstrated reduced radiosensitivity of human tumor cells pretreated with tamoxifen [14, 15], the effects have not been uniform; some studies demonstrated no effect [16], and others have suggested enhanced radiosensitivity [17]. There is no clinical evidence that concomitant tamoxifen and RT could reduce the efficacy of RT alone or in sequential schedule with tamoxifen. Like tamoxifen, AIs appear to cause G1 cell cycle arrest, suggesting that administration of these drugs with radiation could lead to decreased radiation sensitivity [18]. However, in a preclinical study with a breast cancer cell line transfected with an aromatase gene, it was shown that letrozole had a strong radiosensitizing effect [19]. Even with hyperfractionation schedules, if concurrent therapy remained more effective with acceptable or equivalent toxicity, it would likely be preferred.
The first study evaluating the increased risk of radiation-induced pulmonary fibrosis with the concomitant use of tamoxifen was reported by Bentzen and colleagues [11]. After this study two more studies were demonstrated that tamoxifen treatment during post-mastectomy RT enhances the risk of radiation-induced pulmonary fibrosis [9, 10]. Evidence suggests that radiation-induced fibrosis is, in part, mediated by TGF-β. The association of radiation and aromatase inhibitors has not been reported yet. To the best of our knowledge, there are no clinical data in the literature regarding the potential interaction of ionizing radiation and AIs on pulmonary fibrosis.
Bese and colleagues evaluated the effects of tamoxifen on radiation-induced pulmonary fibrosis in Wistar albino rats and found that tamoxifen increased radiation-induced pulmonary fibrosis when used with concomitant radiotherapy [8]. This finding supports our results. In this study a total dose of 30 Gy in 10 fractions RT was given to the rats over 2 weeks. The irradiation doses used in routine clinical practice are different from the ones used in animal studies. Most patients in routine practice are treated with conventional fractionation to a total dose of 50–70 Gy, and it is given in 25–35 fractions. In animal studies it is not practical to use the fractionated schemes. Therefore the biologically equivalent dose of the same total dose in one fraction should be calculated. It has been postulated that the linear quadratic model is an appropriate methodology for determining isoeffective doses at large dose per fraction [20]. According to the linear quadratic model, the 12-Gy single dose of radiotherapy, as used in our study, corresponds to 30 Gy, in the fractions, when α/β ratio of 3–4 is used.
The Arimidex, Tamoxifen, Alone or in Combination (ATAC) trials have shown significantly prolonged disease-free survival, lower rates of recurrence and distant recurrence, and significantly reduced contralateral breast cancer in patients treated with anastrozole compared with tamoxifen [21–23]. Additionally, anastrozole was associated with significantly fewer serious adverse events than tamoxifen, including fewer patients with endometrial cancer, but increased numbers of fractures and reports of arthralgia during treatment [24]. Ten-year analysis of the ATAC trial confirmed the previously reported efficacy and tolerability benefits of anastrozole as initial adjuvant therapy for PMW HR+ breast cancer [25]. Severe adverse events were similar between treatment groups after treatment, and no new safety concerns were reported. In a study of letrozole in women completing tamoxifen, more rapid return to normal endometrial thickness was noted after tamoxifen in women receiving letrozole than those on no treatment [26]. Other short-term side effects such as nausea/vomiting, fatigue, mood disturbance, headaches and dizziness were noted with equal frequency in both arms. In all the trials comparing the third-generation aromatase inhibitors with tamoxifen, the adverse events caused by tamoxifen’s ‘estrogenic’ properties were significantly less common in the aromatase inhibitor groups [27–29]. AI use is associated with fewer endometrial cancers and thromboembolic events than tamoxifen but with more arthralgia and fractures.
Radiation-induced lung damage which is also named as ‘radiation pneumonopathy’ is a continuous process. Radiation-induced lung damage starts as an exudative inflammation, with the clinical picture of interstitial pneumonia 6–12 weeks after irradiation and proceeds to a productive chronic inflammation lasting several months. Inflammation is an essential part of the normal wound healing process [1, 3]. Clinically radiation-induced lung injury is typically divided into two phases: pneumonitis and fibrosis. The fibrotic phase tends to manifest >3 months after treatment. Fibrosis is a kind of wound healing process. Therefore radiation fibrosis is a form of chronic lung damage that usually evolves over 4–24 months after irradiation. In the current study, similar to other studies in the literature, we observed the animals for 16 weeks after the completion of RT [8, 30].
In our study we also found that the use of tamoxifen even without RT caused congestion when compared to the control and anastrozole only groups. Letrozole, both alone and with RT, led to congestion. When we looked at Table 4, although there was not any significant finding, the congestion score of the RT + letrozole group was the worst. Tamoxifen, when used with concomitant RT, increased alveolar inflammation when compared to RT only, RT + anastrozole and RT + letrozole groups. On the other hand, two rats from the RT + letrozole group had lung abscess; yet, the fibrosis scores of the RT only group and RT + letrozole group were not statistically different. This may be due to our sample size. Considering all of these findings together, concomitant use of RT and Tamoxifen is harmful in terms of pulmonary toxicity and concomitant use of RT and anastrozole seems to be the safest.
As a conclusion, concomitant use of tamoxifen appears to increase radiation-induced pulmonary toxicity. However, the use of both anastrozole and letrozole appears to be safe with concomitant RT, without increasing the risk of pulmonary fibrosis. This finding should be clarified with further clinical studies.
References
Graves PR, Siddiqui F, Anscher MS, Movsas B (2010) Radiation pulmonary toxicity: from mechanisms to management. Semin Radiat Oncol 20:201–207
Kocak Z, Evans ES, Zhou SM (2005) Challenges in defining radiation pneumonitis in patients with lung cancer. Int J Radiat Oncol Biol Phys 62:635–638
Trott KR, Herrmann T, Kasper M (2004) Target cells in radiation pneumopathy. Int J Radiat Oncol Biol Phys 58(2):463–469
Kasper M, Haroske G (1996) Alterations in the alveolar epithelium after injury leading to pulmonary fibrosis. Histol Histopathol 11:463–483
Fleckenstein K, Zgonjanin L, Chen L (2007) Temporal onset of hypoxia and oxidative stress after pulmonary irradiation. Int J Radiat Oncol Biol Phys 68:196–204
Chen Y, Williams J, Ding I et al (2002) Radiation pneumonitis and early circulatory cytokine markers. Semin Radiat Oncol 12:26–33
Jordan VC (2004) Selective estrogen receptor modulation: concept and consequences in cancer. Cancer Cell 5:207–213
Bese NS, Umay C, Yildirim S, Ilvan S, Dirican A, Salar S et al (2006) The effects of tamoxifen on radiation-induced pulmonary fibrosis in Wistar albino rats: results of an experimental study. Breast 15:456–460
Koc M, Polat P, Suma S (2002) Effects of tamoxifen on pulmonary fibrosis after cobalt-60 radiotherapy in breast cancer patients. Radiother Oncol 64:171–175
Huang E-Y, Wang C-J, Chen H-C et al (2000) Multivariate analysis of pulmonary fibrosis after electron beam irradiation for postmastectomy chest wall and regional lypmhatics: evidence for non-dosimetric factors. Radiother Oncol 57:91–96
Bentzen SM, Skoczylas JZ, Overgaard M, Overgaard J (1996) Radiotherapy-related lung fibrosis enhanced by tamoxifen. J Natl Cancer Inst 88:918–922
Ashcroft T, Simpson JM, Timbrelli V (1988) Simple method of estimating severity of pulmonary fibrosis on a numerical scale. J Clin Pathol 41:467–470
Osborne C, Boldt D, Clark G et al (1983) Effects of tamoxifen on human breast cancer cell cycle kinetics: accumulation of cells in early G1 phase. Cancer Res 43:3583–3585
Wazer D, Tercilla O, Lin P et al (1989) Modulation in the radiosensitivity of MCF-7 human breast carcinoma cells by 17-estradiol and tamoxifen. Br J Radiol 62:1079–1083
Paulsen G, Strickert T, Marthinsen A et al (1996) Changes in radiation sensitivity and steroid receptor content induced by hormonal agents and ionizing radiation in breast cancer cells in vitro. Acta Oncol 35:1011–1019
Sarkaria J, Miller E, Parker C et al (1994) 4-Hydroxytamoxifen, an active metabolite of tamoxifen, does not alter the radiation sensitivity of MCF-7 breast carcinoma cells irradiated in vitro. Breast Cancer Res Treat 30:159–165
Ellis P, Saccani-Jotti G, Clarke R et al (1997) Introduction of apoptosis by tamoxifen and ICI 182780 in primary breast cancer. Int J Cancer 72:608–613
Whelan T, Levine M (2005) Radiation therapy and tamoxifen: concurrent or sequential? That is the question. J Clin Oncol 23(1):1–4
Azria D, Larbouret C, Cunat S et al (2005) Letrozole sensitizes breast cancer cells to ionizing radiation. Breast Cancer Res 7(1):R156–R163
Brenner DJ (2008) The linear-quadratic model is an appropriate methodology for determining isoeffective doses at large doses per fraction. Semin Radiat Oncol 18(4):234–239
Baum M, Buzdar A, Cuzick J et al (2003) Anastrozole alone or in combination with tamoxifen versus tamoxifen alone for adjuvant treatment of postmenopausal women with early-stage breast cancer: results of the ATAC (Arimidex, Tamoxifen Alone or in Combination) trial efficacy and safety update analyses. Cancer 98:1802–1810
Howell A, Cuzick J, Baum M et al (2005) Results of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) trial after completion of 5 years’ adjuvant treatment for breast cancer. Lancet 365:60–62
Forbes JF, Cuzick J, Buzdar A et al (2008) Effect of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: 100-month analysis of the ATAC trial. Lancet Oncol 9:45–53
Buzdar A, Howell A, Cuzick J et al (2006) Comprehensive side-effect profile of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: long-term safety analysis of the ATAC trial. Lancet Oncol 7:633–643
Cuzick J, Sestak I, Baum M, Buzdar A, Howell A, Dowsett M, Forbes JF, ATAC/LATTE investigators (2010) Effect of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: 10-year analysis of the ATAC trial. Lancet Oncol 11(12):1135–1141
ATAC Trialists’ Group (2002) Anastrozole alone or in combination with tamoxifen versus tamoxifen alone for adjuvant treatment of postmenopausal women with early breast cancer: first results of the ATAC randomized trial. Lancet 359:2131–2139
Coombes RC, Hall E, Gibson LJ, Paridaens R, Jassem J et al (2004) A randomized trial of exemestane after two to three years of tamoxifen therapy in postmenopausal women with primary breast cancer. N Engl J Med 350:1081–1092
Goss PE, Hadji P, Subar M, Abreu P, Thomsen T, Banke-Bochita J (2007) Effects of steroidal and non-steroidal aromatase inhibitors on markers of bone turnover in healthy postmenopausal women. Breast Cancer Res 9(4):R52
Love RR, Barden HS, Mazess RB, Epstein S, Chappell RJ (1994) Effect of tamoxifen on lumbar spine bone mineral density in postmenopausal women after 5 years. Arch Intern Med 154:2585–2588
Bese NS, Umay C, Serdengecti S, Kepil N, Sut N, Altug T, Ober A (2010) The impact of trastuzumab on radiation-induced pulmonary fibrosis: results of an experimental study. Med Oncol 27(4):1415–1419
Acknowledgments
Funding source
This work is supported by Selcuk University, Selcuklu Faculty of Medicine (SUSFM 12401036). There is no role of study sponsors in the study design, in the collection, analysis and interpretation of data; in the writing of the manuscript and in the decision to submit the manuscript for publication.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yavas, G., Yavas, C., Acar, H. et al. Comparison of the effects of aromatase inhibitors and tamoxifen on radiation-induced lung toxicity: results of an experimental study. Support Care Cancer 21, 811–817 (2013). https://doi.org/10.1007/s00520-012-1584-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-012-1584-7