Abstract
Background
Febrile neutropenic cancer patients represent a heterogeneous population with a limited proportion at risk of serious medical complications. The Multinational Association for Supportive Care in Cancer (MASCC) score has been developed and validated for identifying low-risk patients at the onset of febrile neutropenia. Since bacteremia, although not documented at baseline, is a predictor of pejorative outcome, the purpose of this study was to investigate the possible interaction between the MASCC score and bacteremic status and to assess whether, assuming that bacteremic status could be predicted at onset of febrile neutropenia, adding bacteremia as a covariate in a risk model would improve the accuracy of low-risk patients identification.
Methods
Two consecutive multicentric observational studies were carried out from 1994 till 2005 involving 2,142 febrile neutropenic patients. The study data bases were retrospectively used for the present analysis.
Results
A predictive value was found for the MASCC score in all strata obtained by stratification for the bacteremic status with odds ratios for successful outcome being, in patients with a score ≥21, respectively, 6.06 (95%CI: 4.51–8.15), 3.42 (95%CI: 1.95–5.98), and 6.04 (95%CI: 3.01–12.09) in patients without bacteremia, gram-positive bacteremia, and gram-negative bacteremia. No interaction between the MASCC score and the bacteremic status was present. A clinical prediction rule integrating the MASCC score and the bacteremic status was not helpful in improving the identification of low-risk patients. This rule may then be used in a general population of patients with febrile neutropenia without having concerns for a lower predictive value in bacteremic patients.
Conclusions
Our results suggest that the knowledge, provided we could find a model to predict it at fever onset, of a bacteremic etiology of the fever would be of little additional value to the MASCC score when attempting to identify low-risk patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Febrile neutropenia (FN) represents one of the most common complications of chemotherapy in cancer patients. It is a cause of considerable morbidity and carries a significant risk of mortality. Complications and mortality rates have been reported higher in bacteremic patients, especially those with gram-negative bacteremia [1]. However, the prediction of bacteremia or of absence of bacteremia at the onset of FN has proven to be difficult. Although factors such as shock, temperature higher than 40°C, and severe thrombocytopenia have been found to be associated with gram-negative bacteremia [2], a predictive model developed by Viscoli, on the basis of these parameters, was insufficiently discriminant when tested in a validation set [3]. In a more recent population-based study of patients with hematological malignancies, the risk of bacteremia varied greatly according to the type of malignancy; however, the mortality rates (overall cumulative mortality rate at 30 days of 32%) were similar for all underlying neoplastic diseases [4]. Bacteremia documentation being unavailable when treatment has to be initiated and to predict its occurrence appearing unreliable up to now, the further question for the clinician is: Do we really need the documentation of bacteremia? Or can we rely on other systems predictive of risk of complications without integrating bacteremic status?
Several predictive models have indeed been developed to identify patients at low risk of complications [5, 6]. The latter so-called Multinational Association for Supportive Care in Cancer (MASCC) scoring system has been internationally validated under various clinical conditions [7, 8] and has been widely accepted [9]. The use of the MASCC score also allows the selection of low-risk patients who can be safely treated with orally administered antibiotics and be, for at least some of them, successfully discharged early after a 24-h in-hospital observation [8]. However, there is still room for improvement of the MASCC score.
Therefore, as bacteremia is a known risk factor for the occurrence of complication, we hypothesized that the integration of this covariate, if known, could improve the discriminant ability of the MASCC score. Therefore, we were interested in (1) analyzing the MASCC score discriminant ability when stratifying the patients by bacteremic status, (2) assessing whether the baseline knowledge of bacteremia could improve risk assessment models targeted at the identification of low-risk patients, and (3) further exploring the ability to predict bacteremia at the time of treatment initiation in more recent series of patients.
Methods
We consecutively carried out two multicenter prospective observational studies from 1994 till 2005 involving patients treated with empiric antibiotic regimens for chemotherapy-induced FN. The first study led to the development of the so-called MASCC score, internationally validated, aimed at identifying low-risk patients (those defined as having a probability of at least 95% of fever resolution without developing a serious medical complication or death) at the onset of FN. The second survey was performed in order to look more closely at variables susceptible to have an impact on the neutropenia duration as it was hypothesized that the integration of such variables could improve the model. The results of this second survey are not yet published.
Data from 2,142 eligible patients (respectively, 1,139 and 1,003) were collected and pooled together for the present analysis. The full list of the participating investigators and institutions is given in Appendix.
Statistical methodology
The data were thoroughly inspected and explored using univariate analyses (contingency tables and descriptive statistics) as well as multivariate analyses (scatter matrices and logistic regression) to detect multicollinearity and outliers that were checked. The χ 2 test and Fisher’s exact test were used to test the statistical significance of differences in discrete data; Student’s t test and Mann–Whitney’s test were used to compare continuous variables. Homogeneity of the odds ratios (OR) was assessed using the Breslow–Day test. All reported P values were two-tailed, and we considered as significant a nominal P < 0.05, although multiple tests were done, considering that all the analyses that were carried out had an exploratory purpose.
To assess whether the integration of bacteremic status improves the MASCC score, the data were separated into a development set and a test set. The models were constructed using the development set (first study, 1994–1997, n = 1,139) and prospectively tested on the test set (second study, 1997–2005, n = 1,003). Confidence intervals at 95% of the area under the receiver operating characteristic (ROC) curves (AUCs) on the test set were calculated, and the method proposed by DeLong and colleagues was used to check for statistically significant differences in AUCs [10].
To address the problem of predicting bacteremia/absence of bacteremia, a logistic regression model was constructed. The factors considered as possibly associated with the diagnosis of bacteremia or gram-negative bacteremia, all available at FN onset, were: age (<60, ≥60), sex, underlying cancer (hematological, solid), treatment setting (adjuvant or neoadjuvant, first line, second line, bone marrow transplant), presence of a clinical site of infection (yes/no), controlled cancer (yes/no), granulopoiesis stimulating factors (yes/no), prophylactic antibiotics (yes/no), ECOG performance status (0 to 4), burden of illness (no symptoms, mild symptoms, moderate symptoms, severe symptoms, moribund), hospitalization status (inpatient/outpatient), temperature (<39°C, ≥39°C), fever duration at presentation (<24 h, ≥24 h), abnormality on the chest X-ray (yes/no), hypotension (yes/no), pulse (≥120 beats/min, <120 beats/min), respiratory rate (>24 breaths/min, ≤24 breaths/min), comorbidity (multiple choices possible: cardiac disease, chronic obstructive pulmonary disease, diabetes, confusion or alteration of mental state, blood loss, dehydration, weight loss of >5% within 1 month), previous FN (yes/no), previous fungal infection (yes/no), Talcott group (I to IV), hemoglobin level (≥8 g/dL, <8 g/dL), absolute neutrophil count (≥100/µL, <100/µL), platelet count (≥5,000/µL, <5,000/µL), creatininemia (≥2 mg/dL, <2 mg/dL), bilirubinemia (≥2 mg/dL, <2 mg/dL), albumin level (≥2.5 g/dL, <2.5 g/dL), and the MASCC score (<21, ≥21). Then based on forward–backward selection methods (using the statistical significance level of the differences in χ 2) and after checking for interactions among the factors and determining whether the model was linear in the logit for continuous factors, an input selection was made for the logistic regression models. The data were not separated into a development set and a test set, resulting in an overestimation of the predictive performance. The reason for doing this was the limited number of patients with gram-negative bacteremia: we wanted to have the largest possible number of such cases in order not to miss any possible prognostic marker.
Results
Patient characteristics
Median age was 52 years, the male-to-female ratio was almost 1:1. Fifty-seven percent (1,223 of 2,142) had hematological tumor, and 69% (1,488 of 2,142) of the patients were predicted at low risk (MASCC ≥ 21) with a 91% successful outcome rate (1,349 of 1,488) among them.
In 23% (499 of 2,142), bacteremia was present: 8% (168 of 2,142) single gram-negative bacteremia, 13% (283 of 2,142) single gram-positive bacteremia, and 2% (48 of 2,142) polymicrobial bacteremia. The overall serious complications rate including death was 14% (228 of 1,643) in non-bacteremic patients, 40% (68 of 168) in single gram-negative bacteremia, 25% (70 of 283) in single gram-positive bacteremia, and 35% (17 of 48) in polymicrobial bacteremia.
More details on the sociodemographic characteristics and pathogens causative for bacteremia were given in a previous publication [1] which looked at the outcomes and types of complications developed by patients with bacteremia.
Effect of MASCC score on complications with stratification by bacteremia status
Table 1 indicates patients’ outcome (complications and mortality) according to the MASCC score and stratifying for the bacteremic status. Predicted low-risk non-bacteremic patients had an overall 7% rate of severe complications including a mortality rate of 1%. On the other hand, in predicted high-risk patients, the corresponding rates were 32% and 9%. The rates of resolution without complication were statistically significant between the two groups (P < 0.001). Similar results were observed for single gram-positive and single gram-negative bacteremias: e.g., patients with gram-negative bacteremia and with a MASCC score <21 had a rate of complications of 60% including a mortality of 29%, while the corresponding rates in patients with gram-negative bacteremia and a MASCC score ≥21 were 20% and 6% (P < 0.001). No heterogeneity in the odds of having a successful outcome in both risk groups could be detected (P = 0.20) for the three strata of bacteremic status.
Since the negative predictive value of the MASCC score is better in patients with a solid tumor and bacteremia occurs more frequently in hematological malignancies, the analysis was further stratified according to tumor type with comparable results in both disease groups: patients with MASCC score <21 have poorer outcomes than patients predicted at a low risk of complications, regardless of tumor type.
As indicated in Table 2, the MASCC index score does not only predict differences when dichotomized. As expected, due to the construction of the score, the lower the score, the greater the risk of complications and death. This increased risk of complications and death is most significant in patients with a MASCC score below 15.
The incidence of bacteremia in the sample population is related to the MASCC score (Table 3). Bacteremia was less often present in predicted low-risk patients (MASCC ≥ 21): 19% (290 of 1,488) compared to 32% (209 of 654) in predicted high-risk patients (MASCC <21) (OR, 0.52; 95%CI, 0.42–0.63, P < 0.001). Mainly single gram-negative bacteremia appeared less frequently in low-risk patients, i.e., only 5% (81 of 1,488) versus 13% (87 of 654) in non-low-risk patients (OR, 0.38; 95%CI, 0.27–0.52, P < 0.001).
Does the inclusion of bacteremia as a baseline covariate improve the MASCC score?
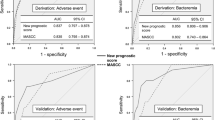
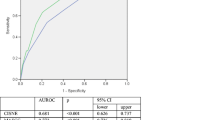
Or in other words, would knowledge—at the time of fever onset—of the presence of a bacteremia improve the identification of low-risk or high-risk patients? Three logistic regression models were constructed on the derivation set (first study, 1994–1997, n = 1,139) in order to predict a successful outcome (no serious complications) using as explanatory variables: (1) the MASCC score, (2) the MASCC score in combination with bacteremia, and (3) the MASCC score in combination with gram-negative bacteremia (all variables had P < 0.001). The ROCs from applying the three models (1), (2) and (3) to the test data (second study, 1997–2005, n = 1,003) are shown in Fig. 1. The AUC is significantly better when considering the model with the MASCC score and the knowledge of bacteremia, but this better performance is due to improvements occurring at low values of sensitivity. As our goal with a revised prediction rule would be to improve sensitivity while preserving the positive predictive value, there is no clinical relevance for the improvement. The AUCs and comparison tests were: (1) 0.756 (95%CI, 0.720–0.792), (2) 0.773 (95%CI, 0.738–0.807), (3) 0.755 (95%CI, 0.719–0.792); (1) versus (2) P = 0.02, (1) versus (3) P = 0.89. When the analysis was restricted to death prediction, bacteremia as well as gram-negative bacteremia were significantly associated with mortality when combined with the MASCC score (chi-square P = 0.03 and P = 0.01 on the development set). No difference in AUCs could be observed in the test data (see Fig. 2): (1) 0.778 (95%CI 0.715–0.840), (2) 0.790 (95%CI 0.729–0.851), (3) 0.791 (95%CI 0.729–0.854). The P values for the comparisons between the areas were (1) versus (2) P = 0.31 and (1) versus (3) P = 0.12.
Prediction of bacteremia and gram-negative bacteremia
Although there are significant differences in the incidence of bacteremia according to the MASCC score, the score cannot be reliably used for predicting bacteremia: sensitivity of 42% (209 of 499), specificity of 73% (1,198 of 1,643), positive predictive value (PPV) of 32% (209 of 654), and negative predictive value (NPV) of 81% (1,198 of 1,488). The same holds for the prediction of gram-negative bacteremia: sensitivity of 52% (87 of 168), specificity of 71% (1,407 of 1,974), PPV of 13% (87 of 654), and NPV of 95% (1,407 of 1,488).
Therefore, a predictive model was built considering 28 characteristics for input selection as stated in the methodology section. Logistic regression analysis resulted in the delineation of an optimal set of variables independently related to the presence of bacteremia (Table 4). The predictive performance of this model was the following: area under the ROC curve of 0.720 (95%CI, 0.695–0.744), sensitivity 69%, specificity 64%, PPV 37%, and NPV 87% at a probability cutoff level of 0.24.
Similarly, a model was constructed in order to predict gram-negative bacteremia; for that purpose, the gram-negative bacteremias considered were the single gram-negative bacteremias and the polymicrobial bacteremias containing at least one gram-negative organism (Table 4). The area under the ROC curve was 0.742 (95%CI, 0.707–0.776), sensitivity 72%, specificity 66%, PPV 17%, and NPV 96% at a probability cutoff level of 0.09.
Discussion
We found a significant association between the predicted risk of complications and the bacteremic documentation: patients at a low risk of complications have also a lower risk of bacteremia than the other patients. Namely, gram-negative bacteremia is significantly more frequent (13%) in the high-risk patients compared to the low-risk group (5%).
The risk of complications and death was increased in bacteremic patients in both strata of predicted low- and high-risk patients—especially in patients with gram-negative bacteremia. However, we did not detect any interaction between the MASCC score and the bacteremic status, which led us to the conclusion that the MASCC score is discriminant in all strata. These results remain true if we are dividing patients into three risk groups rather than two.
In addition, the integration of the bacteremic status failed to increase the accuracy of a clinical prediction rule aiming at identifying patients at low risk of complications. The reverse situation would have led us to solve the problem of estimating the presence of bacteremia at fever onset, although we were not able to solve it. Indeed, our results confirm that the absence of bacteremia is unpredictable, at least with the covariates that we assess today systematically. As bacteremia is a heterogeneous entity, we also attempted to predict the absence of gram-negative bacteremia with the same conclusion that we failed to develop a satisfactory model. In the future, it is possible that we might have some laboratory parameters to be used as markers for bacteremia like C-reactive protein, interleukin, or procalcitonin levels; but—up to now—these markers were not demonstrated specific enough, specially at the start of a febrile episode [11–13], and were most often studied in single-institution studies with small sample sizes and heterogeneous patient populations. Multicenter trials with larger numbers of patients are needed to clarify the role of these markers and their potential to be useful early enough for the prediction of serious complication which is in fact a clinically important event, above the knowledge of bacteremia. Nevertheless, early identification of bacteremia remains an interesting theoretical issue as well as a practical issue for targeting the choice of the antibiotherapy (for instance if the absence of gram-negative bacteremia could be predicted) and a potential area for further research.
We observed that patients with a low MASCC score and a gram-negative bacteremia have a very high rate of complications and death (60% and 29%, respectively). Predicting such high-risk patients is another very interesting issue that was not really addressed by the clinical prediction rule derived from the MASCC score. This subgroup of patients fortunately represents a low proportion of febrile neutropenic patients, and any attempt to develop a rule for predicting such a high-risk population would need a further study with a sample size larger than the one of the data base we were presently able to analyze.
Our data indicate that, whatever the MASCC score is, the mortality in patients with gram-positive bacteremia is not different from that of non-bacteremic patients, confirming previous observations about the relatively indolent course of gram-positive infections in neutropenic patients [2, 14], except in those with a very low (<15) score, in whom gram-positive bacteremia can be a very serious event.
Finally, our conclusions were not different in patients with hematological malignancies and in those with solid tumors, although the negative predictive value of the MASCC score is slightly better in solid tumor patients than in hematological patients; this means that the MASCC score is able to capture, using other covariates, the predictive value that the underlying disease carries and, contrary to the bacteremic status, the underlying disease is not an independent prognostic factor of outcome which is against a common belief that a patient with a hematological underlying disease is always at high risk of complications and death during an episode of FN [15, 16]. We also confirmed that the MASCC score is not only helpful with a dichotomization into patients at predicted low and high risk. The MASCC score is also able to identify patients at very high risk of complications, and this was further discussed in a previous publication [1]. Developing specific therapeutic approaches for this very high-risk group is another very interesting topic for further research.
References
Klastersky J, Ameye L, Maertens J et al (2007) Bacteraemia in febrile neutropenic cancer patients. Int J Antimicrob Agents 30(suppl 1):S51–S59
Klastersky J, Zinner SH, Calandra T et al (1988) Empiric antimicrobial therapy for febrile granulocytopenic cancer patients: lessons from four EORTC trials. Eur J Cancer Clin Oncol 24(suppl 1):S35–S45
Viscoli C, Bruzzi P, Castagnola E et al (1994) Factors associated with bacteremia in febrile, granulocytopenic cancer patients. Eur J Cancer 30:430–437
Norgaard M, Larsson H, Pedersen G, Schonheyder HC, Sorensen HT (2006) Risk of bacteraemia and mortality in patients with haematological malignancies. Clin Microbiol Infect 12:217–223
Talcott JA, Siegel RD, Finberg R, Goldman L (1992) Risk assessment in cancer patients with fever and neutropenia: a prospective, two-center validation of a prediction rule. J Clin Oncol 10:316–322
Klastersky J, Paesmans M, Rubenstein EB et al (2000) The Multinational Association for Supportive Care in Cancer risk index: a multinational scoring system for identifying low-risk febrile neutropenic cancer patients. J Clin Oncol 18:3038–3051
Uys A, Rapoport BL, Anderson R (2004) Febrile neutropenia: a prospective study to validate the Multinational Association of Supportive Care of Cancer (MASCC) risk-index score. Support Care Cancer 12:555–560
Klastersky J, Paesmans M, Georgala A et al (2006) Outpatient oral antibiotics for febrile neutropenic cancer patients using a score predictive for complications. J Clin Oncol 24:4129–4134
Hughes WT, Armstrong D, Bodey GP et al (2002) 2002 guidelines for the use of antimicrobial agents in neutropenic patients with cancer. Clin Infect Dis 34:730–751
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845
Kern WV, Heiss M, Steinbach G (2001) Prediction of gram-negative bacteremia in patients with cancer and febrile neutropenia by means of interleukin-8 levels in serum: targeting empirical monotherapy versus combination therapy. Clin Infect Dis 32:832–835
Massaro KS, Costa SF, Leone C, Chamone DA (2007) Procalcitonin (PCT) and C-reactive protein (CRP) as severe systemic infection markers in febrile neutropenic adults. BMC Infect Dis 7:137
Uys A, Rapoport BL, Fickl H, Meyer PW, Anderson R (2007) Prediction of outcome in cancer patients with febrile neutropenia: comparison of the Multinational Association of Supportive Care in Cancer risk-index score with procalcitonin, C-reactive protein, serum amyloid A, and interleukins-1beta, -6, -8 and -10. Eur J Cancer Care 16:475–483
Elting LS, Rubenstein EB, Rolston KVI, Bodey GP (1997) Outcomes of bacteremia in patients with cancer and neutropenia: observations from two decades of epidemiological and clinical trials. Clin Infect Dis 25:247–259
Freifeld A, Marchigiani D, Walsh T et al (1999) A double-blind comparison of empirical oral and intravenous antibiotic therapy for low-risk febrile patients with neutropenia during cancer chemotherapy. N Engl J Med 341:305–311
Kern WV, Cometta A, de Rock R et al (1999) Oral versus intravenous empirical antimicrobial therapy for fever in patients with granulocytopenia who are receiving cancer chemotherapy. N Engl J Med 341:312–318
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Participating Institutions and Investigators
The following investigators and institutions did contribute to the two observational studies which are the basis of the report (number of eligible episodes given in parentheses):
MASCC survey I (reference [6])
L. Elting, K. Rolston, E. Rubenstein; MD Anderson Cancer Center, Houston, TX, USA (172 patients)
T. Berghmans, J. Klastersky, P. Mommen, M. Paesmans; Institut Jules Bordet, Brussels, Belgium (159 patients)
B. De Pauw, J.P. Donnelly; Algemeen Universitair Ziekenhuis, Nijmegen, The Netherlands (91 patients)
R. Feld, A. McGeer; Ontario Cancer Institute, Toronto, Canada (83 patients)
T. Calandra, O. Marchetti; Centre Hospitalier Universitaire Vaudois, Lausanne, Switzerland (73 patients)
W. Feremans, A. Kentos; Hôpital Erasme, Brussels, Belgium (53 patients)
I. Malik; National Cancer Institute, Karachi, Pakistan (52 patients)
J.L. Michaux, S. Neumeister; Cliniques Saint-Luc, Brussels, Belgium (50 patients)
J. Herrstedt, K. Wedervang; Herlev Hospital, University of Copenhagen, Copenhagen, Denmark (49 patients)
W. Kern; Medizinisches Universitätsklinik, Ulm, Germany (46 patients)
I. Bover; Hospital Sant Joan, Reus, Spain, (43 patients)
M. Boyer; Royal Prince Alfred Hospital, Camperdown, Australia (41 patients)
P. Ljungman; Huddinge University Hospital, Huddinge, Sweden (40 patients)
J. Vorlicek; Masaryk University Hospital, Brno, Czech Republic (35 patients)
Z. Aziz; Jinnah Hospital, Lahore, Pakistan (27 patients)
B. L. Rapoport; Medical Oncology Centre of Rosebank, Johannesburg, and Pretoria Academic Hospital, Pretoria, South Africa (27 patients)
J. Gallagher; Geisinger Medical Center, Danville, PA, USA (26 patients)
J. Talcott; Dana Farber Cancer Institute, Boston, MA, USA (25 patients)
M. Viot; Centre Antoine Lacassagne, Nice, France (25 patients)
R. De Bock; Algemeen Ziekenhuis Middelheim, Antwerp, Belgium (22 patients)
Second observational study (main results not yet published)
L. Ameye, M. Aoun, M. Barette, F. Crokaert, L. Dubreucq, A. Georgala, J. Klastersky, Y. Lalami, A. Loizidou, F. Muanza, M. Paesmans, B. Plehiers, A. Schwarzbold, M. Vekemans; Institut Jules Bordet, Brussels, Belgium (618 patients)
J. Maertens; University Hospital Gasthuisberg, Leuven, Belgium (102 patients)
A. Uys, B. L. Rapoport; Medical Oncology Centre of Rosebank, Johannesburg, South Africa (71 patients)
S. Costantini, A. Ferrant; Cliniques Saint-Luc, Brussels, Belgium (63 patients)
R. De Bock; Algemeen Ziekenhuis Middelheim, Antwerp, Belgium (50 patients)
C. Slabber; Mary Potter Oncology Centre, Pretoria, South Africa (38 patients)
J. Wingard; University of Florida Shands Cancer Center, Gainesville, FL, USA (25 patients)
C. Alexopoulos; Evangelismos Hospital, Athens, Greece (16 patients)
F. Rossini, EM Monza; Lisson, Italy (11 patients)
D. Schrijvers; U.H Antwerp, Antwerpen, Belgium (9 patients)
Rights and permissions
About this article
Cite this article
Paesmans, M., Klastersky, J., Maertens, J. et al. Predicting febrile neutropenic patients at low risk using the MASCC score: does bacteremia matter?. Support Care Cancer 19, 1001–1008 (2011). https://doi.org/10.1007/s00520-010-0925-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-010-0925-7