Abstract
Purpose
The purpose of this study is to review the evidence base from 1990 to 2008 to (1) clarify the impact of cancer therapies on prevalence of osteoradionecrosis (ORN) in head and neck cancer patients, and to (2) evaluate management strategies and their consequences on quality of life and cost of care.
Methods
Articles were selected for the time period beginning after 1989, excluding the 1990 NCI monograph articles from the 1989 NIH-sponsored Oral Complications in Cancer Therapy Symposium that was published in 1990. The search included both Medline/PubMed and Embase and was limited to humans. The search was limited to publications in the English language. No abstracts were utilized in the current review. Each article was evaluated by two reviewers. A weighted prevalence was calculated for the prevalence of ORN while incorporating predetermined quality measures. The level of evidence, recommendation grade, and guideline (if possible) were provided for published preventive and management strategies for ORN.
Results
A total of 43 articles between 1990 and 2008 were reviewed. The weighted prevalence for ORN included conventional radiotherapy (RT) = 7.4%, intensity modulated RT (IMRT) = 5.1%, chemoradiotherapy (CRT) = 6.8%, and brachytherapy = 5.3%. Hyperbaric oxygen may contribute a role in management of ORN. However, no clear guideline recommendations could be established for the prevention or treatment of ORN based on the literature reviewed.
Conclusions
New cancer treatment modalities such as IMRT and concomitant CRT have had minimal effect on prevalence of ORN. No studies to date have systematically addressed impact of ORN on either quality of life or cost of care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Definition of oral complication and unanswered questions
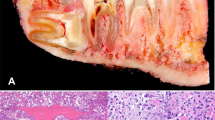
Osteoradionecrosis (ORN) is characterized by a non-healing area of exposed bone of at least 6 months duration in a patient who has been treated with radiation therapy for cancer. ORN is associated with pain and morbidity and, in advanced stages, typically requires surgical resection and reconstruction for management. An example of a case of ORN of several years duration in a cancer patient is presented (Figs. 1 and 2).
a This patient presented with osteoradionecrosis 2 years after computer-planned curative radiotherapy. Lesion causation was possibly related to an ill-fitting prosthesis. b Panoramic image with bony sequestum visible. Treatment included osteosynthesis during ablative surgery, with mandibular splinting
a This patient developed osteoradionecrosis (ORN) 5 years after curative postoperative radiotherapy. Note the extra-oral fistula from ORN of the mandible, in association with periodontal disease with the mandibular molar. No cancer recurrence was identified via biopsy. b Panoramic image of the patient demonstrating ORN contiguous with the periodontally compromised mandibular molar. Courtesy of Dr. M. Witjes, University Medical Center Groningen, The Netherlands
Risk of ORN increases with radiation dosages above 6,000 cGy, previous cancer resection, advanced dental disease status, and postradiation dental extractions [1, 2]. In a cohort of 68 patients with ORN, 34 (50%) had a tooth extraction closely associated with the onset of ORN [2]. However, not all patients who develop ORN have identifiable specific causes. Furthermore, not all risk factors (e.g., severely compromised dentition) predictably cause ORN.
The prevention or treatment of ORN often includes surgical debridement with adjunctive therapies such as antibiotics and hyperbaric oxygen (HBO) therapy. Thus, a major issue relative to ORN is the need to determine optimal preventive or treatment strategies that may or may not include HBO.
A summary of unanswered questions is listed in “Recommendations for future research directions” at the end of this report.
Historical perspective—prior to 1990
The modeling for ORN and its management was initially delineated in the 1980s. It was addressed as a component of the NIH Consensus Conference in 1989 [3]. Key Conference outcomes relative to ORN included the following:
-
ORN is one of the most serious complications arising from head and neck radiation therapy.
-
Current research has shown that ORN represents non-healing, necrotic bone and is not an infection.
-
ORN results from functional and structural bony changes that may not be expressed for months or years. Furthermore, ORN may occur either spontaneously or in response to wound causation.
-
Predisposing factors include absorbed radiation dose, fractionation, delivery modality, and dental status.
-
Timing of dental extractions and other factors affect incidence.
-
ORN may be reduced through early intraoral evaluation, treatment, and adequate healing time prior to beginning radiation therapy.
-
HBO therapy has been beneficial in the prevention and treatment of ORN. It is of paramount importance for the medical community to recognize the factors that may reduce ORN incidence, endorse oral care protocols, and acknowledge the value of HBO therapy in the prevention and treatment of this disease.
Twenty years later, another expert panel convened in April 2009 in Bethesda, Maryland to address oral complications of emerging cancer therapies, including ORN [4]. As noted above, key questions from this conference are summarized in “Recommendations for future research directions” at the end of this report.
Advances in cancer therapies since 1989
New advances in cancer therapy since 1989 are being used to provide more targeted and effective modalities of radiotherapy (RT; e.g., appearance and optimizing of 3D treatment planning, conformal radiation techniques, and intensity modulated RT (IMRT) and proton beam radiation therapy). Since 1989, the standard of care for treatment of more advanced head and neck cancers includes concurrent chemotherapy and RT that frequently incorporates IMRT technology.
New directions in treatment of ORN include ultrasound, biologics, distraction osteogenesis, and antioxidant agents. Given the relative recent use of these technologies, their relationship to ORN incidence and severity has not been systematically reported to date. Therefore, these technologies will not be addressed in further detail in this review.
Aims of systematic review
To extend on the 1989 NIH Development Consensus Conference on the Oral Complications of Cancer Therapies [3], the goals of this systematic review of ORN as an oral complication of cancer therapies were as follows:
-
1.
Determine the prevalence of ORN by cancer therapy regimen;
-
2.
Determine the impact of ORN on quality of life;
-
3.
Determine the economic impact of ORN;
-
4.
Assess prevention and management strategies for ORN and determine the quality of recommendations for different treatment strategies.
Methodology
Summary of methodology
A systematic literature search was conducted for articles published between January 1, 1990 and December 31, 2008 [5]. The goals of this search were delineation of the prevalence of ORN in head and neck cancer patients treated with RT alone or combined treatment modalities, its impact on quality of life and health care costs, and evaluation of prophylactic or treatment strategies for the lesion.
Literature search utilized
An initial literature search was completed with MEDLINE, CancerLit, EMBASE, Cochrane Library, and Best Evidence [5]. A more specific literature search was completed for the keywords “ORN” and “Cancer” to determine if additional literature was not identified in the initial literature search. Additional studies identified in the references of reviewed articles were also included in this review.
The senior author (MB) compiled of list of articles to be reviewed. A search for additional articles in each section was then performed by the authors.
The search included both Medline and Embase and was limited to humans.
No abstracts were utilized in the current review.
Types of publications excluded
The search was limited to English language [5]. Gender and age were not limited. The following publication types were eliminated by the review panel from the present systematic review: systematic and non-systematic reviews, studies not reporting actual data on ORN, studies reporting redundant data from previous publications or if later follow-up publication relevant, opinion papers and case reports, articles published before 1990, and articles from the 1990 NCI Monograph [3].
Review method
Each article was independently evaluated by two reviewers (WD, AH, AP, DS, and MB) with pilot-tested collection forms [5]. ORN was assessed by the presence (Y/N) when available. Measures of QOL and economic variables were documented if available. Further data collected for each article such as type of study, blinding, presence of control group, scale validity, and samples size were used to determine the quality grading.
Prevalence and weighting
Prevalence was reported as the proportion affected and computed (as described below) as the mean of the proportion affected from each study in the group, weighted by the assigned quality points, along with 95% confidence intervals. This method was utilized and reported in a previous analysis of the incidence of oral mucositis related to cancer therapy [6].
The overall quality adjusted ORN prevalence (p overall) was defined as
where qsj is the quality score for the jth study, and p j is the proportion of subjects with oral complications observed in the jth study [7]. We anticipated that many studies would have small sample sizes, and thus, the Gaussian approximation to the binomial distribution, which is a large sample result, would not be appropriate. Therefore, we computed an estimate of the 95% confidence interval for the overall quality-adjusted ORN prevalence using the bootstrap method as follows [8]:
One thousand bootstrap samples were generated for each treatment type, and the overall quality weighted oral complication prevalence was calculated for each bootstrap sample. The bootstrap ORN prevalences were ordered from smallest to largest, and the 2.5th percentile and 97.5th percentile bootstrap ORN prevalences were used to approximate the 95% bootstrap confidence interval for the treatment regimen. All analyses were conducted using STATA 10.1 (Statacorp, College Station, TX, USA).
Table 1 presents the raw as well as weighted data. The weighted prevalence data are included in order to enhance the accuracy of estimation of the true prevalence of ORN, by taking into account the study quality parameters as described.
Results
Articles reviewed
Forty-three articles were reviewed as a result of the literature search. The cancer types evaluated included the following: nasopharynx or sinus squamous cell carcinoma (SCCA)—one study; oropharynx, oral cavity, or tonsil SCCA—15 studies; and mixed head and neck SCCA—28 studies. Conventional RT was evaluated in 38 studies, IMRT in four studies, and brachytherapy in one study. Fifteen studies evaluated combined RT and CT, and 13 studies assessed patients treated with brachytherapy (with or without CT). The study design types included randomized clinical trials (n = 2), before and after studies (n = 10), cohort studies (n = 29), and case–control studies (n = 2).
Prevalence
Prevalence of ORN could be determined from 31 studies where the presence of ORN was appropriately assessed (Table 1). The weighted prevalence for ORN in patients treated with conventional RT was 7.4%, with IMRT = 5.2%, with RT + chemotherapy (CT) = 6.8%, and with brachytherapy with or without additional RT = 5.3%.
Impact on quality of life
There were no studies evaluating the quality of life impact of ORN.
Economic impact
There were no studies evaluating the economic impact of ORN.
Prevention and/or treatment strategies
Description of number of articles and types of strategies evaluated
A total of 13 studies that addressed intervention for the prevention or treatment of ORN was evaluated.
Summary of results for the different prevention and treatment strategies
-
(A)
Prevention of ORN (Table 2)
Table 2 Prevention of osteoradionecrosis -
1.
Spacers in brachytherapy
One study evaluated if spacers could prevent ORN in a cohort of patients treated with brachytherapy. There was a much higher prevalence of ORN in patients that were treated without spacers (40%) vs. those that were treated with spacers (2%) [9].
-
2.
HBO therapy
HBO therapy is commonly recommended for prevention of ORN, but the clinical efficacy and the cost-effectiveness of this therapy is unclear. As previously noted, dental extractions increase the risk of ORN; therefore, effective preventive therapies would be an important strategy to avoid this problematic long-term side effect of radiation therapy. In an earlier prospective clinical trial in 1985, Marx et al. showed pre- and postoperative antibiotics with atraumatic extractions in postradiation patients had a complication rate of 29.9%, while HBO decreased the complication rate to 5.4% [10]. Following the 1989 NIH Consensus Conference [3], two retrospective cohort studies have assessed the prevalence of ORN in patients receiving post-RT dental extractions that either did or did not receive HBO prior to extractions. A study by Vudiniabola et al. demonstrated one case of ORN in 29 postradiation patients (3.4%) treated with prophylactic HBO prior to extractions, while one of seven patients (14.3%) who did not receive prophylactic HBO developed ORN [11]. In another study by Sulaiman et al., two cases of ORN developed in 100 post-RT patients (2%) not treated with prophylactic HBO prior to extractions, while none of the seven patients who did receive prophylactic HBO developed ORN [12]. Of the seven patients who did receive HBO therapy, one developed a secondary tumor, and another patient developed a new primary solid tumor. In a report by Adkinson et al., ORN did not develop in 40 patients receiving prophylactic HBO therapy for dental extractions post-RT, but no comparison group was evaluated in this study [13].
-
3.
Other preventive strategies
Limited prevention studies regarding hard tissue replacement in extraction sites, use of postoperative antibiotics, and removal vs. leaving impacted third molar preradiation treatment are also reported in Table 2. Additional studies are required to further evaluate these preventive options.
-
(B)
Treatment of ORN (Table 3)
Table 3 Treatment of osteoradionecrosis -
1.
HBO therapy alone
HBO therapy provides a pressurized environment where patients breathe 100% oxygen. Originally developed for the treatment of decompression sickness, it is primarily used today as a management strategy of wound care. The mechanisms of action for HBO are thought to include enhanced perfusion, stimulation of collagen matrix for new blood vessels, improved resting oxygen levels, and bactericidal activity [14].
Seven studies were identified that evaluated the efficacy of HBO therapy with or without varying degrees of surgical management [13, 15–20]. In general, HBO therapy does not appear to have a significant advantage in resolution of ORN compared to surgical management. Resolution rates of ORN with HBO ranged from 19% to 93% and seemed to improve with concomitant surgical intervention. A 2004 randomized, placebo-controlled multicenter trial demonstrated no benefit of HBO therapy in the management of active ORN [19].
-
2.
Pentoxifylline
One study assessed the efficacy of pentoxifylline and vitamin E in a cohort of 18 patients that were refractory to prior therapy including antibiotics (n = 9), HBO therapy (n = 6), and/or sequestrectomy (n = 6) [21]. All patients received 2–4 weeks of amoxicillin/clavulanate (2 g/day), fluconazole (50 g/day), and methylprednisolone (16 mg/day) prior to pentoxifylline and vitamin E. This open-label study design demonstrated an 89% resolution of ORN, but additional, larger cohort studies that are placebo-controlled are needed to determine the efficacy of this treatment option.
-
3.
Vascularized bone-containing flap
A small open label study of nine patients with ORN demonstrated 100% resolution with the use of a vascularized bone-containing flap [22]. Confirmation with larger studies is necessary to demonstrate the efficacy of this surgical therapy.
Summary
This systematic review identified the following overall trends in the literature:
-
(A)
Prevention of ORN
-
Four studies included consideration of IMRT, a targeted cancer therapy, relative to ORN prevention [23–26]. These studies collectively demonstrated that although the weighted prevalence with IMRT was lower than with conventional RT (5.2% vs. 7.3%, respectively), additional studies are needed to determine if this difference is clinically significant.
-
Three studies evaluated the use of HBO therapy for the prevention of ORN in patients requiring dental extractions. In two non-randomized studies [11, 12], a comparison was made between patients who did vs. those who did not receive preventive HBO prior to dental extractions. Together, these two studies demonstrated a similar prevalence of ORN with 1/36 (2.8%) in the HBO group and 3/107 (2.8%) in the non-HBO group. In another study that assessed 40 patients who all receive preventive HBO prior to dental extractions, ORN was identified in seven of 456 (1.5%) of the teeth extracted [13].
-
Four other studies were identified that reported on clinical interventive strategies to prevent ORN. Of these,
-
One study involved brachytherapy with or without spacers (randomized study, n = 103). A statistically significant difference in prevalence of ORN was observed (brachytherapy with spacers, 2.1%; brachytherapy without spacers, 40%).
The three other studies were directed to,
-
Hard tissue replacement (open label study, n = 8);
-
Postoperative antibiotics (open label study, n = 43);
-
Removal of third molars pre-RT (randomized, n = 96).
-
-
-
(B)
Treatment of ORN
-
HBO-based treatment of ORN has received the most comprehensive analysis and reporting, accounting for seven of the nine studies evaluated. The clinical research has been both retrospectively as well as prospectively based.
-
The remaining two, non-HBO treatment strategies reported in the literature include pentoxyfilline (one randomized study; n = 18) and vascularized bone-containing graft (one open label study, n = 9).
-
This status of literature reported to date has resulted in limitations of the current evidence base, as summarized in “Summary of limitations of current literature” below. These limitations in turn permit generation of only selected clinical preventive or treatment recommendations relative to ORN, as described below. Current clinical decision-making for prevention or treatment of ORN is thus based on the relatively limited scope of research to date combined with professional judgment and experience.
Research opportunities exist relative to each domain cited below and as then summarized in “Recommendations for future research directions.” If successful, such research may provide the evidence base for a more comprehensive list of recommendations for prevention and treatment of ORN in the future.
Prevalence
A total of 43 articles between 1990 and 2008 were reviewed. The weighted prevalence for ORN was similar between the different cancer therapies: conventional RT (RT) = 7.4%, IMRT = 5.1%, chemoradiotherapy = 6.8%, and brachytherapy = 5.3%.
It is important to note that few studies were available for assessment of prevalence in relation to type of cancer therapy. Therefore, the weighted prevalence may not be an accurate representation of the true prevalence of ORN associated with IMRT. The difference in the mean raw prevalence and the mean weighted prevalence reflects the range of differences in study quality with the four studies evaluated in the present review.
It is also noteworthy that there was a wide range of cancer therapies reported in the literature that was reviewed. Therefore, we stratified by the four groups as delineated in Table 1. Further stratification by other specific cancer therapies was not relevant to this analytic approach, given the small number of studies (example, n = one or two) that would have otherwise resulted from this strategy. This current limitation of the collective literature could be obviated by increasing the number of high quality studies in the future. This expansion of number of published studies could in turn lead to further delineation of the relationship of IMRT and other therapies to prevalence for ORN.
QOL and economic impact
No studies to date have systematically addressed either the quality of life or health care cost impact of ORN.
High quality new clinical research in these fields is needed.
Prevention strategies with level of evidence, recommendation grade, and guideline classification
-
Use of prophylactic HBO therapy for the prevention of ORN in patients requiring post-RT dental extractions
-
Level of evidence III, recommendation grade C: no guideline possible.
-
Management strategies with level of evidence, recommendation grade, and guideline classification
-
HBO therapy for treatment of ORN
-
Level of evidence II, recommendation grade B: single therapy HBO not recommended for treatment of ORN.
(Note: This conclusion is directed to single therapy HBO only vs. HBO in combination with other treatment including surgery).
-
Summary of limitations of current literature
The current literature is collectively limited in scope and/or quality by the following issues:
-
Limited number of randomized, double-blind, placebo-controlled trials;
-
Evolving protocols relative to delivery techniques for RT;
-
Dynamic nature of concurrent chemotherapy regimens and introduction of novel drugs (e.g., biologics) with unknown effects on the ORN trajectory;
-
Clinical trial design issues, including the following:
-
Definitions of clinical endpoints and grading of ORN;
-
Variations in follow-up periods;
-
Assessment/reporting of patient-related factors (e.g., vasculo-connective tissue and other systemic disease conditions;
-
Limited reporting of local RT dose/distribution to the mandible.
-
Recommendations for future research directions
New research, particularly large prospective observational and clinical trials, is needed to answer the questions listed below. These questions have emerged from both the current systematic review as well as the April 2009 conference “Oral complications of emerging cancer therapies” [4].
Questions that ideally should be addressed in large, prospective, multi-center, observational studies of risk, outcomes, and cost of ORN for various treatment strategies are as follows:
-
What is the role of radiation treatment strategy and dental planning in relation to ORN?
-
Are there specific valid predictors of risk for ORN?
-
What is the impact of ORN on quality of life and cost of care?
-
How do the emerging, novel cancer therapies affect prevalence of ORN?
Questions that ideally should be addressed in prospective clinical trials are as follows:
-
Is prevention of ORN possible?
-
What is the role of “adjuvant preventive therapy” (e.g., HBO; antibiotics)?
-
Is there a subset of patients at risk for ORN for whom HBO is or is not effective?
-
What is the most effective method of treatment of ORN?
-
What are the mechanistic and clinical relationships of novel ORN treatment modalities (e.g., ultrasound, biologics, distraction osteogenesis, and antioxidants) in relation to ORN management?
References
Katsura K, Sasai K, Sato K, Saito M, Hoshina H, Hayashi T (2008) Relationship between oral health status and development of osteoradionecrosis of the mandible: a retrospective longitudinal study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 105:731–738
Reuther T, Schuster T, Mende U, Kubler A (2003) Osteoradionecrosis of the jaws as a side effect of radiotherapy of head and neck tumour patients—a report of a thirty year retrospective review. Int J Oral Maxillofac Surg 32:289–295
National Institutes of Health (1990) Consensus development conference on oral complications of cancer therapies: diagnosis, prevention, and treatment. Bethesda, Maryland, April 17–19, 1989. NCI Monogr 9:1–184
National Institutes of Health (2009) Oral complications of emerging cancer therapies. Bethesda, MD USA, April 14-15, 2009 (Primary funding provided by National Institutes of Health, Bethesda, MD, USA)
Brennan MT, Elting LS, Spijkervet FK (2010) Systematic reviews of oral complications from cancer therapies, Oral Care Study Group, MASCC/ISOO: methodology and quality of the literature. Supp Care Cancer. doi:10.1007/s00520-010-0856-3
Sonis ST, Elting LS, Keefe D, Peterson DE, Schubert M, Hauer-Jensen M, Bekele BN, Raber-Durlacher J, Donnelly JP, Rubenstein EB (2004) Perspectives on cancer therapy-induced mucosal injury: pathogenesis, measurement, epidemiology, and consequences for patients. Cancer 100(9 Suppl):1995–2025
Berard A, Bravo G (1998) Combining studies using effect sizes and quality scores: application to bone loss in postmenopausal women. J Clin Epidemiol 51:801–807
Efron B (1993) An introduction to the bootstrap. Chapman and Hall, New York City
Miura M, Takeda M, Sasaki T, Inoue T, Nakayama T, Fukuda H, Hoshi A, Hoshina M, Shibuya H (1998) Factors affecting mandibular complications in low dose rate brachytherapy for oral tongue carcinoma with special reference to spacer. Int J Radiat Oncol Biol Phys 41:763–770
Marx RE, Johnson RP, Kline SN (1985) Prevention of osteoradionecrosis: a randomized prospective clinical trial of hyperbaric oxygen versus penicillin. J Am Dent Assoc 111:49–54
Vudiniabola S, Pirone C, Williamson J, Goss AN (1999) Hyperbaric oxygen in the prevention of osteoradionecrosis of the jaws. Aust Dent J 44:243–247
Sulaiman F, Huryn JM, Zlotolow IM (2003) Dental extractions in the irradiated head and neck patient: a retrospective analysis of Memorial Sloan-Kettering Cancer Center protocols, criteria, and end results. J Oral Maxillofac Surg 61:1123–1131
Adkinson C, Anderson T, Chavez J, Collier R, MacLeod S, Nicholson C, Odland R, Vellis P (2005) Hyperbaric oxygen therapy: a meeting place for medicine and dentistry. Minn Med 88:42–45
Marx RE, Johnson RP (1988) Problem wounds in oral and maxillofacial surgery: the role of hyperbaric oxygenation. In: Davis JC, Hunt TK (eds) Problem wounds-the role of oxygen. Elsevier, New York, pp 65–128
Notani K, Yamazaki Y, Kitada H, Sakakibara N, Fukuda H, Omori K, Nakamura M (2003) Management of mandibular osteoradionecrosis corresponding to the severity of osteoradionecrosis and the method of radiotherapy. Head Neck 25:181–186
Jisander S, Grenthe B, Salemark L (1999) Treatment of mandibular osteoradionecrosis by cancellous bone grafting. J Oral Maxillofac Surg 57:936–942, discussion 942-943
David LA, Sandor GK, Evans AW, Brown DH (2001) Hyperbaric oxygen therapy and mandibular osteoradionecrosis: a retrospective study and analysis of treatment outcomes. J Can Dent Assoc 67:384
Maier A, Gaggl A, Klemen H, Santler G, Anegg U, Fell B, Karcher H, Smolle-Juttner FM, Friehs GB (2000) Review of severe osteoradionecrosis treated by surgery alone or surgery with postoperative hyperbaric oxygenation. Br J Oral Maxillofac Surg 38:173–176
Annane D, Depondt J, Aubert P, Villart M, Gehanno P, Gajdos P, Chevret S (2004) Hyperbaric oxygen therapy for radionecrosis of the jaw: a randomized, placebo-controlled, double-blind trial from the ORN96 study group. J Clin Oncol 22:4893–4900
Aitasalo K, Niinikoski J, Grenman R, Virolainen E (1998) A modified protocol for early treatment of osteomyelitis and osteoradionecrosis of the mandible. Head Neck 20:411–417
Delanian S, Depondt J, Lefaix JL (2005) Major healing of refractory mandible osteoradionecrosis after treatment combining pentoxifylline and tocopherol: a phase II trial. Head Neck 27:114–123
Militsakh ON, Wallace DI, Kriet JD, Tsue TT, Girod DA (2005) The role of the osteocutaneous radial forearm free flap in the treatment of mandibular osteoradionecrosis. Otolaryngol Head Neck Surg 133:80–83
Claus F, Duthoy W, Boterberg T, De Gersem W, Huys J, Vermeersch H, De Neve W (2002) Intensity modulated radiation therapy for oropharyngeal and oral cavity tumors: clinical use and experience. Oral Oncol 38:597–604
van den Broek GB, Balm AJ, van den Brekel MW, Hauptmann M, Schornagel JH, Rasch CR (2006) Relationship between clinical factors and the incidence of toxicity after intra-arterial chemoradiation for head and neck cancer. Radiother Oncol 81:143–150
Studer G, Studer SP, Zwahlen RA, Huguenin P, Gratz KW, Lutolf UM, Glanzmann C (2006) Osteoradionecrosis of the mandible: minimized risk profile following intensity-modulated radiation therapy (IMRT). Strahlenther Onkol 182:283–288
Mendenhall WM, Morris CG, Amdur RJ, Hinerman RW, Malyapa RS, Werning JW, Lansford CD, Villaret DB (2006) Definitive radiotherapy for tonsillar squamous cell carcinoma. Am J Clin Oncol 29:290–297
Ryu JK, Stern RL, Robinson MG, Bowers MK, Kubo HD, Donald PJ, Rosenthal SA, Fu KK (1995) Mandibular reconstruction using a titanium plate: the impact of radiation therapy on plate preservation. Int J Radiat Oncol Biol Phys 32:627–634
Leborgne F, Leborgne JH, Zubizarreta E, Mezzera J (2002) Cesium-137 needle brachytherapy boosts after external beam irradiation for locally advanced carcinoma of the tongue and floor of the mouth. Brachytherapy 1:126–130
Allal AS, Bieri S, Miralbell R, Marchal F, Lehmann W, Kurtz JM (1997) Feasibility and outcome of a progressively accelerated concomitant boost radiotherapy schedule for head and neck carcinomas. Int J Radiat Oncol Biol Phys 38:685–689
Toljanic JA, Ali M, Haraf DJ, Vokes EE, Moran WJ, Graham L (1998) Osteoradionecrosis of the jaws as a risk factor in radiotherapy: a report of an eight-year retrospective review. Oncol Rep 5:345–349
Grabenbauer GG, Rodel C, Brunner T, Schulze-Mosgau S, Strnad V, Muller RG, Iro H, Sauer R (2001) Interstitial brachytherapy with Ir-192 low-dose-rate in the treatment of primary and recurrent cancer of the oral cavity and oropharynx. Review of 318 patients treated between 1985 and 1997. Strahlenther Onkol 177:338–344
Takacsi-Nagy Z, Polgar C, Oberna F, Somogyi A, Major T, Remenar E, Fodor J, Kasler M, Nemeth G (2004) Interstitial high-dose-rate brachytherapy in the treatment of base of tongue carcinoma. Strahlenther Onkol 180:768–775
Abitbol A, Abdel-Wahab M, Lewin A, Troner M, Rodrigues MA, Hamilton-Nelson KL, Markoe A (2002) Phase II study of tolerance and efficacy of hyperfractionated radiotherapy and 5-fluorouracil, cisplatin, and paclitaxel (Taxol) in stage III and IV inoperable and/or unresectable head-and-neck squamous cell carcinoma: A-2 protocol. Int J Radiat Oncol Biol Phys 53:942–947
Umeda M, Komatsubara H, Nishimatsu N, Yokoo S, Shibuya Y, Komori T (2000) High-dose rate interstitial brachytherapy for stage I-II tongue cancer. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 90:667–670
Pernot M, Luporsi E, Hoffstetter S, Peiffert D, Aletti P, Marchal C, Kozminski P, Noel A, Bey P (1997) Complications following definitive irradiation for cancers of the oral cavity and the oropharynx (in a series of 1134 patients). Int J Radiat Oncol Biol Phys 37:577–585
De Crevoisier R, Domenge C, Wibault P, Koscielny S, Lusinchi A, Janot F, Bobin S, Luboinski B, Eschwege F, Bourhis J (2001) Full dose reirradiation combined with chemotherapy after salvage surgery in head and neck carcinoma. Cancer 91:2071–2076
Carl W, Ikner C (1998) Dental extractions after radiation therapy in the head and neck area and hard tissue replacement (HTR) therapy: a preliminary study. J Prosthet Dent 79:317–322
Hehr T, Classen J, Welz S, Ganswindt U, Scheithauer H, Koitschev A, Bamberg M, Budach W (2006) Hyperfractionated, accelerated chemoradiation with concurrent mitomycin-C and cisplatin in locally advanced head and neck cancer, a phase I/II study. Radiother Oncol 80:33–38
Withers HR, Peters LJ, Taylor JM, Owen JB, Morrison WH, Schultheiss TE, Keane T, O’Sullivan B, van Dyk J, Gupta N et al (1995) Late normal tissue sequelae from radiation therapy for carcinoma of the tonsil: patterns of fractionation study of radiobiology. Int J Radiat Oncol Biol Phys 33:563–568
Le Scodan R, Pommier P, Ardiet JM, Montbarbon X, Malet C, Favrel V, Zrounba P, Poupart M, Ceruse P, Ferlay C, Clippe S (2005) Exclusive brachytherapy for T1 and T2 squamous cell carcinomas of the velotonsillar area: results in 44 patients. Int J Radiat Oncol Biol Phys 63:441–448
Skladowski K, Maciejewski B, Golen M, Tarnawski R, Slosarek K, Suwinski R, Sygula M, Wygoda A (2006) Continuous accelerated 7-days-a-week radiotherapy for head-and-neck cancer: long-term results of phase III clinical trial. Int J Radiat Oncol Biol Phys 66:706–713
Huguenin P, Glanzmann C, Taussky D, Lutolf UM, Schmid S, Moe K (1998) Hyperfractionated radiotherapy and simultaneous cisplatin for stage-III and -IV carcinomas of the head and neck. Long-term results including functional outcome. Strahlenther Onkol 174:397–402
Olver IN, Hughes PG, Smith JG, Narayan K, Bishop JF (1996) Concurrent radiotherapy and continuous ambulatory infusion 5-fluorouracil in advanced head and neck cancer. Eur J Cancer 32A:249–254
Arias F, Dominguez MA, Illarramendi JJ, Martinez E, Tejedor M, Dominguez S, Duenas M, Villafranca E, Elcarte F, Miqueliz S et al (1995) Split hyperfractionated accelerated radiation therapy and concomitant cisplatin for locally advanced head and neck carcinomas: a preliminary report. Int J Radiat Oncol Biol Phys 33:675–682
Fujita M, Hirokawa Y, Kashiwado K, Akagi Y, Kashimoto K, Kiriu H, Ohtani K, Wada T (1996) An analysis of mandibular bone complications in radiotherapy for T1 and T2 carcinoma of the oral tongue. Int J Radiat Oncol Biol Phys 34:333–339
Langendijk JA, Kasperts N, Leemans CR, Doornaert P, Slotman BJ (2006) A phase II study of primary reirradiation in squamous cell carcinoma of head and neck. Radiother Oncol 78:306–312
Eisen MD, Weinstein GS, Chalian A, Machtay M, Kent K, Coia LR, Weber RS (2000) Morbidity after midline mandibulotomy and radiation therapy. Am J Otolaryngol 21:312–317
Tong AC, Leung AC, Cheng JC, Sham J (1999) Incidence of complicated healing and osteoradionecrosis following tooth extraction in patients receiving radiotherapy for treatment of nasopharyngeal carcinoma. Aust Dent J 44:187–194
Gibbs IC, Le QT, Shah RD, Terris DJ, Fee WE, Goffinet DR (2003) Long-term outcomes after external beam irradiation and brachytherapy boost for base-of-tongue cancers. Int J Radiat Oncol Biol Phys 57:489–494
Maguire PD, Meyerson MB, Neal CR, Hamann MS, Bost AL, Anagnost JW, Ungaro PC, Pollock HD, McMurray JE, Wilson EP, Kotwall CA (2004) Toxic cure: hyperfractionated radiotherapy with concurrent cisplatin and fluorouracil for stage III and IVA head-and-neck cancer in the community. Int J Radiat Oncol Biol Phys 58:698–704
Oh HK, Chambers MS, Garden AS, Wong PF, Martin JW (2004) Risk of osteoradionecrosis after extraction of impacted third molars in irradiated head and neck cancer patients. J Oral Maxillofac Surg 62:139–144
Medina JA, Rueda A, de Pasos AS, Contreras J, Cobo M, Moreno P, Benavides M, Villanueva A, Alba E (2006) A phase II study of concomitant boost radiation plus concurrent weekly cisplatin for locally advanced unresectable head and neck carcinomas. Radiother Oncol 79:34–38
Wadsley JC, Patel M, Tomlins CD, Gildersleve JQ (2003) Iridium-192 implantation for T1 and T2a carcinoma of the tongue and floor of mouth: retrospective study of the results of treatment at the Royal Berkshire Hospital. Br J Radiol 76:414–417
Acknowledgement
The authors thank Ms. Tainika Williams, Department of Oral Medicine, Carolinas Medical Center, North Carolina, USA, for her excellent administrative assistance.
Conflicts of interest
The authors declared that they have no potential conflicts of interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
All authors are members of the Oral Care Study Group of the Multinational Association of Supportive Care in Cancer (MASCC)/International Society of Oral Oncology (ISOO).
Rights and permissions
About this article
Cite this article
Peterson, D.E., Doerr, W., Hovan, A. et al. Osteoradionecrosis in cancer patients: the evidence base for treatment-dependent frequency, current management strategies, and future studies. Support Care Cancer 18, 1089–1098 (2010). https://doi.org/10.1007/s00520-010-0898-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-010-0898-6