Abstract
Purpose
Improving health-related quality of life (HRQL) is the main goal of palliative care and an important outcome for oncology trials. This study examines medical and sociodemographic determinants of HRQL in outpatients with advanced cancer.
Methods
Patients with metastatic gastrointestinal, genitourinary, breast, lung or gynecological cancer, ECOG 0-2, and clinical prognosis of 6 months to 2 years were recruited from outpatient medical oncology clinics. HRQL was measured using the FACT-G questionnaire and the FACIT-Sp meaning and peace (existential) subscale. The influence of demographic and medical characteristics on HRQL was determined using t tests and analysis of variance, with Tukey’s correction for multiple comparisons. Multivariate linear regression was used to determine independent predictors.
Results
Of 285 patients, 57% were female and the median age was 61 years; 44% were alive at latest follow-up; and of those deceased, the mean survival time was 10 months. The strongest determinants of overall HRQL were increased age (p < 0.001), good performance status (PS; p < 0.001) and survival time >6 months (p = 0.001). Compared to patients receiving cancer treatment, those awaiting new treatment had worse emotional well-being (p < 0.001), while those on surveillance or whose treatment had been stopped had worse existential well-being (p = 0.03). Male gender predicted better emotional and physical well-being and lower income predicted worse social well-being.
Conclusions
Age, PS, survival time, and treatment status are important determinants of HRQL in patients with advanced cancer. Decision aids, open communication, and involvement of supportive care specialists may improve emotional and existential distress associated with changing or stopping cancer treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Maximizing health related quality of life (HRQL) for patients is a central focus of palliative care [1–3]. HRQL is typically measured according to physical, functional, social, and psychological domains; in addition, the existential domain is of particular relevance in patients with advanced cancer [4–6]. HRQL is determined not only by the disease and its treatment, but also by other medical and sociodemographic characteristics [7–11]. It is important to develop an understanding of variables that may influence HRQL for patients with advanced cancer, so that these can be accounted for in clinical trials; it is also important to identify vulnerable groups, so that their HRQL can be specifically addressed and optimized.
Most studies of determinants of HRQL have been conducted in general populations [7–10]. Such studies have reported better HRQL among those who are younger [7, 9, 10], male [9, 10], married [7, 8], and have higher education [7, 8]. Studies comparing cancer and non-cancer populations have shown that a malignant diagnosis is not associated with reduced global HRQL, although having cancer reduces physical and role function [11, 12]. There have been only three studies investigating determinants of HRQL for patients with advanced cancer [13–15], only two of which had significant results [13, 14]. Both used the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire-Core 30 (EORTC QLQ-C30) and reported less pain and better emotional functioning in older patients, more nausea and vomiting in women, and worse social functioning in married/cohabiting patients [13, 14]. The third study used the Functional Assessment of Cancer Therapy-General (FACT-G) measure and found that HRQL in people with advanced cancer (clinical prognosis 3 months to 2 years) did not vary significantly in relation to marital status, education level, ECOG performance status, or clinician-estimated life expectancy [15]. Although spiritual well-being was strongly associated with HRQL in this last study [15] and it has been recommended that spirituality be included as a domain in HRQL measures [6, 16], no previous study has included the existential domain as an outcome rather than a predictor of HRQL. Treatment status was only assessed in one study, where just 13% of patients were receiving cancer treatment [13]; no impact on HRQL was found.
The purpose of our study was to examine factors associated with HRQL for outpatients with advanced cancer, including physical, emotional, social, functional, and existential domains. We hypothesized that better HRQL would be associated with demographic factors such as increased age, male gender, and higher income, and with disease-related factors such as better performance status, lower comorbidity, and increased survival time. For treatment status we had no directional hypotheses, as HRQL could improve with treatment, but could also be influenced by side effects.
Patients and methods
Study participants
Patients were recruited from December 2006 to December 2008, as part of a cluster randomized controlled trial of early intervention by a specialized palliative care team versus routine oncology care in patients with advanced cancer. Recruitment took place at 24 oncology clinics at Princess Margaret Hospital, a comprehensive cancer center in Toronto, Canada.
Eligibility criteria included a diagnosis of stage IV gastrointestinal, genitourinary, breast or gynecological cancer, or stage III/IV lung cancer, ECOG ≤2, and a clinical prognosis of 6 months to 2 years (the latter two criteria were determined by the patient’s primary oncologist). Patients with locally advanced pancreatic or esophageal cancer were also included. Those with insufficient English to complete the questionnaires or who did not pass the cognitive screening test (Short Orientation-Memory-Concentration Test score <20 or >10 errors) [17] were excluded.
All patients provided written informed consent; those who did not wish to proceed with the trial were asked for written consent to complete baseline measures only. Because this was a cluster-randomized study, randomization of clinics occurred before patient consent. To decrease bias, patients recruited for the control group were not told about the existence of a trial and were invited to participate in a study assessing quality of life and satisfaction with care. This consent process has been used previously in cluster-randomized trials of palliative care [18] and other interventions [19, 20]. The protocol was approved by the Research Ethics Board of the University Health Network.
Measures
Consenting patients completed measures of HRQL at baseline and at monthly intervals for 4 months. For this study, baseline measures were used for all analyses.
The FACT-G is a 27-item internationally validated questionnaire. The core of the FACIT scales, it is divided into four primary HRQL domains: physical well-being, social/family well-being, emotional well-being and functional well-being [21, 22]. The total FACT-G score is calculated by summing the four subscale scores. A two-point difference on the FACT-G subscale scores and a five-point difference on the FACT-G are associated with clinically and subjectively meaningful differences [22–24].
The 12-item Functional Assessment of Chronic Illness Therapy-Spiritual Well-being (FACIT-Sp) is a validated measure of spiritual well-being [16, 25], which consists of two subscales complementary to the FACT-G. One subscale measures existential well-being (meaning and peace; eight items) and includes statements such as “I have a reason for living”. The other assesses religious well-being (faith; four items), and includes items such as “I find comfort in my faith or spiritual beliefs”. HRQL is reported to depend much more on the meaning and peace than on the faith subscale [6, 15], which may even have a negative impact [26]. We used the eight-item meaning and peace subscale to measure existential well-being.
The primary outcome was HRQL including physical, social, emotional, functional, and existential well-being, as measured by the combined score of the four FACT-G subscales and the meaning and peace subscale; secondary outcomes were the individual subscales. As suggested in the FACT-G and FACIT-Sp scoring guidelines [22], when there were missing items, subscale scores were prorated by multiplying the sum of the subscale by the number of items in that subscale, then dividing by the number of questions answered. This is considered acceptable as long as more than 50% of the items are answered for that subscale [22].
The Charlson Comorbidity Index (CCI) generates a weighted score based on the presence of various medical illnesses [27]; it has good reliability and validity, and is the most commonly used measure of comorbidity for patients with cancer [28].
Patients completed a demographic questionnaire at the time of enrolment. This included age, gender, ethnic origin [29], level of education, marital status, living arrangement, employment status, household income, cancer treatment, and comorbid diagnoses. In addition, research staff reviewed medical records to document and verify demographic data, cancer diagnosis, stage, and cancer treatment status. The latter was abstracted in duplicate (DB, CZ) using a standardized abstraction sheet. Discrepancies were resolved by jointly referring to the medical records.
Statistical analyses
The mean total and subscale scores for the HRQL scales were compared among subgroups according to patient medical and sociodemographic characteristics using Student’s t test and one-way analysis of variance, with Tukey’s correction for multiple comparisons. Demographic variables included those listed above; medical variables included performance status, primary cancer site, survival time after completion of the measures, and cancer treatment status. Treatment status was categorized as follows: “receiving cancer treatment” (receiving chemotherapy, hormonal therapy and/or radiation); “awaiting new treatment” (those awaiting a further line of treatment), or “no cancer treatment” (those on surveillance or where treatment had been stopped).
The influence of medical and demographic characteristics on HRQL was examined using multivariate linear regression. The initial model included all of the above covariates except marital status, cancer site, and employment status. Marital status was excluded due to collinearity with living situation, and employment status due to collinearity with age. Cancer site was excluded because certain sites are gender-specific (e.g., breast and gynecological). Age, comorbidity, and performance status were included as continuous variables. The following variables were dichotomized: income (≥$60,000 vs. <$60,000), education (≥high school vs. >high school), living situation (alone vs. with others), and ethnic origin (non-European vs. European).
For survival following completion of the questionnaires, multiple dichotomous (‘dummy’) variables were first entered into the model: ≤6 months, >6-12 months, >12-18 months, >18-24 months, and >24-30 months, with alive as the reference variable. However, only survival ≤6 months was significantly associated with any HRQL outcomes, and so this variable was subsequently dichotomized (≤6 vs. >6 months). Multiple dichotomous variables were also created for treatment status, with receiving cancer treatment as the referent. In total, there were ten independent variables; thus, the recommended sample size for adequate power is at least 200 subjects (20 subjects per independent variable) [30].
A backwards stepwise selection process was used to build the regression models. A two-sided p < 0.05 was considered statistically significant. Analyses were performed with SPSS, version 16.0 (SPSS Inc, Chicago, IL, USA).
Results
Patient characteristics
Of 582 eligible patients approached, 285 completed baseline measures; an additional 96 initially consented to participate but did not ultimately complete baseline measures. The most common reasons for declining to participate were lack of interest (n = 84) and time required (n = 45).
Table 1 shows the demographic and Table 2 the medical characteristics of the study sample (n = 285). The median age was 61 years, 57% were female, 72% were married/common law, and 18% lived alone. Forty-four percent were alive at the time of analysis; and of those who were deceased, the mean interval from completion of measures to death was 10 months. Comorbidity was low with a median CCI score of 0 (range, 0-6). The most prevalent coexisting medical diagnoses were hypertension (n = 81), high cholesterol (n = 39), diabetes (n = 37), ischemic heart disease (n = 24), and arthritis (n = 24), psychiatric diagnoses included depression (n = 13), and anxiety disorder (n = 5). The mean and median FACT-G and FACIT-Sp subscale and total scores are shown on Table 3.
Univariate analyses
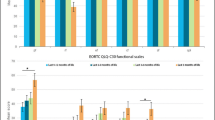
HRQL scores according to demographic and medical characteristics are shown on Table 4. Older patients and men had better physical and emotional well-being than younger patients and women. Patients of European background reported better physical well-being than those of non-European origin. Patients with lower income had worse social well-being on the FACT-G scale. Those who were employed or retired had better well-being for the physical, functional, and emotional subscales than those who were unemployed or on disability.
Patients with poor performance status had worse physical, emotional, functional, and existential well-being. Patients with lung cancer had the worst physical and functional HRQL while emotional well-being was lowest for those with breast and gynecological cancers. There were no significant differences for treatment status (Table 4) nor for living situation, marital status, or education (data not shown). Patients who survived less than 6 months had the worst HRQL subscores for all domains except social well-being.
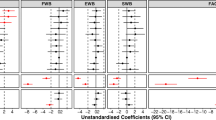
Determinants of HRQL according to multivariate analyses
The strongest and most consistent determinants of overall HRQL were increased age, good performance status, and a survival time of greater than 6 months (Table 5). Older age was a particularly strong predictor of physical and emotional well-being and better performance status and longer survival were especially associated with physical and functional well-being. Compared to patients receiving cancer treatment, those awaiting a new treatment line had worse emotional well-being, while those who were not receiving treatment had worse existential well-being. Male gender predicted better emotional and physical well-being and lower income predicted worse social well-being.
Discussion
This study examined sociodemographic and medical determinants of HRQL for outpatients with advanced cancer using validated measures including the existential domain. The strongest determinants of overall HRQL were older age, good performance status, and subsequent survival of more than 6 months. Treatment status had a strong impact on emotional well-being and also affected existential well-being. Other predictors such as male gender and higher income had a smaller impact on particular subscales.
Younger age was associated with worse HRQL, particularly in the physical and emotional domains. These findings are similar to those of two studies using the EORTC QLQ-C30 to measure HRQL in patients with advanced cancer, which found associations between younger age, and worse emotional functioning and pain control [13, 14]. In contrast, studies in general populations have consistently reported a decline in HRQL with older age [7, 9–11, 31]. This contrasting influence of age in general populations compared to patients with advanced cancer may be explained by the fact that comorbidity contributes to worsening HRQL with age [11], but may not be of the same relative importance for patients with advanced cancer. A diagnosis of advanced cancer may also be more traumatizing for younger patients, because they are less likely to expect a diagnosis of terminal illness [32], and are more likely to have concurrent roles and responsibilities such as being the main family wage earner or the parent of young children [33, 34]. There remains a dearth of literature on the specific needs of younger patients with cancer and their families and further research is needed in this area.
Both performance status and survival time were independent determinants of physical, functional, emotional, and existential well-being. These findings confirm those of a study using the EORTC QLQ-C30 measure [13] and demonstrate that although performance status is a predictor of prognosis [35], it cannot be used reliably as a proxy for survival time. Rather, survival time should also be included as a covariate in trials of advanced cancer patients with HRQL as an outcome. This can be done by waiting at least 6 months after completion of the study before conducting analyses and dichotomizing by survival <6 versus ≥6 months. Another study measuring existential well-being found that this was associated with self-rated performance status; however, it was unclear whether patients found more meaning and peace because they were less affected by their illness, or whether their existential well-being protected them from feeling the effects of their illness [6]. Our finding that survival time and clinician-rated performance status are associated with existential well-being indicates that spiritual well-being decreases with advancing disease and decline in function. Lack of existential well-being has in turn been associated with depression [36] and may be amenable to change with psychotherapeutic and palliative interventions [37, 38].
To our knowledge, the current study is the first to report the impact of treatment status on HRQL in patients with advanced cancer; in another study where only 13% of patients were receiving chemotherapy, treatment status was examined but not found to be significant [13]. Allowing for age, performance status, and survival time, patients in our study who were awaiting a new line of chemotherapy had the worst emotional well-being, while those who were neither receiving nor anticipating treatment had the worst existential well-being. There was no association between treatment status and functional or physical well-being. Because patients awaiting new treatment have recently received news that their cancer is getting worse, their distress may reflect this news, combined with the uncertainty of whether or not the next treatment will be effective. Conversely, receiving active treatment in the setting of advanced disease may convey a false sense of security and prevent end-of-life planning or the engagement in meaningful life review [39]. Decision aids; open, honest communication of expectations; and the involvement of palliative care and psychosocial oncology specialists may help to guide patients and clinicians through the difficult decisions associated with cancer treatment at the end of life.
Emotional as well as physical well-being was also impacted by gender. Our findings of worse physical and emotional well-being in women are similar to those of a general population study using the FACT-G [7], although the scores in our sample were worse, and the gender differences more pronounced. Population studies using the EORTC QLQ-C30 have also found better emotional functioning in men than in women [9–11], and investigations in oncology regarding specific symptoms have noted increased severity in women of depression [40–44], anxiety [43–45], fatigue [13, 46–49], and nausea [50]. It is not clear whether these findings indicate a gender disparity in symptom perception [51], reporting [52], or treatment, and further studies are indicated to explain these differences.
Social well-being was rated consistently high and had few significant determinants other than level of income. Indeed, compared with general population data from the USA [12], Austria [7], and Australia [8], social/family well-being was rated slightly better in our sample (22 vs. 19-20), although our sample scored worse on the FACT-G total score (75 vs. 80-87). Our sample also scored worse on all domains of HRQL than those in previous studies of HRQL of heterogeneous cancer populations (mean FACT-G total score 80.4 [53] and 80.9 [12], respectively), but the social well-being subscore in these studies was similar to that found for our sample (22.1 and 22.3, respectively). These findings of higher perceived social well-being for patients with cancer, whether in the early or advanced stage, may reflect a greater need for support from family and friends during serious illness. The questionnaire contains items such as “I get emotional support from my family” and “I get support from my friends”. This support may be more apparent in a situation where it is explicitly required.
Limitations of our study include the generally high income, high level of education, and predominantly European ethnic origin of our sample, which has also been the case for other studies [54]. We also limited the study to those with relatively good performance status to ensure appropriate trial follow-up, which may restrict generalizability. This was also the case for two previous studies assessing determinants of HRQL in patients with advanced cancer [13, 15]; studies recruiting patients specifically to assess HRQL determinants are needed. There was a high proportion of missing data for income, which may have influenced the results. Data for this study are cross-sectional and further longitudinal studies are necessary to investigate the relationship of HRQL to treatment status and survival time. Finally, we used measures designed for cancer but not specifically for palliative care. However, although the latter measures usually include existential well-being, they may measure inadequately physical and functional aspects of HRQL [55]. We therefore complemented the well-validated FACT-G with a measure of existential well-being.
Our results show that for outpatients with advanced cancer, the most important sociodemographic and medical determinants of HRQL are age, performance status, survival time, and treatment status. Although the former two are generally accounted for in trials of palliative care interventions, the latter are often omitted. The impact of treatment status on emotional and existential well-being underscores the importance of attending to communication of treatment decisions and providing adequate psychological and spiritual support. Further epidemiologic studies in ethnically diverse populations and with patients of mixed sociodemographic and educational backgrounds are necessary. Further research is also needed regarding the effectiveness of targeted interventions for specific patient subgroups.
References
World Health Organization. WHO definition of palliative care. Available from URL: http://www.who.int/cancer/palliative/definition/en. 2002. Accessed 23 Oct 2009
Kaasa S, Loge JH (2003) Quality of life in palliative care: principles and practice. Palliat Med 17:11–20
Morrison RS, Meier DE (2004) Clinical practice. Palliative care. N Engl J Med 350:2582–2590
Steinhauser KE, Christakis NA, Clipp EC, McNeilly M, McIntyre L, Tulsky JA (2000) Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA 284:2476–2482
Wilson KG, Chochinov HM, McPherson CJ, LeMay K, Allard P, Chary S et al (2007) Suffering with advanced cancer. J Clin Oncol 25:1691–1697
Whitford HS, Olver IN, Peterson MJ (2008) Spirituality as a core domain in the assessment of quality of life in oncology. Psycho Oncology 17:1121–1128
Holzner B, Kemmler G, Cella D, De Paoli C, Meraner V, Kopp M et al (2004) Normative data for functional assessment of cancer therapy—general scale and its use for the interpretation of quality of life scores in cancer survivors. Acta Oncol 43:153–160
Janda M, Disipio T, Hurst C, Cella D, Newman B (2009) The Queensland cancer risk study: general population norms for the Functional Assessment of Cancer Therapy-General (FACT-G). Psycho Oncology 18:606–614
Hjermstad MJ, Fayers PM, Bjordal K, Kaasa S (1998) Health-related quality of life in the general Norwegian population assessed by the European Organization for Research and Treatment of Cancer Core Quality of Life Questionnaire: the QLQ = C30 (+ 3). J Clin Oncol 16:1188–1196
Schwarz R, Hinz A (2001) Reference data for the quality of life questionnaire EORTC QLQ-C30 in the general German population. Eur J Cancer 37:1345–1351
Fossa SD, Hess SL, Dahl AA, Hjermstad MJ, Veenstra M (2007) Stability of health-related quality of life in the Norwegian general population and impact of chronic morbidity in individuals with and without a cancer diagnosis. Acta Oncol 46:452–461
Brucker PS, Yost K, Cashy J, Webster K, Cella D (2005) General population and cancer patient norms for the Functional Assessment of Cancer Therapy-General (FACT-G). Eval Health Prof 28:192–211
Jordhoy MS, Fayers P, Loge JH, Saltnes T, Ahlner-Elmqvist M, Kaasa S (2001) Quality of life in advanced cancer patients: the impact of sociodemographic and medical characteristics. Br J Cancer 85:1478–1485
Lundh HC, Seiger A, Furst CJ (2006) Quality of life in terminal care—with special reference to age, gender and marital status. Support Care Cancer 14:320–328
Fisch MJ, Titzer ML, Kristeller JL, Shen J, Loehrer PJ, Jung SH et al (2003) Assessment of quality of life in outpatients with advanced cancer: the accuracy of clinician estimations and the relevance of spiritual well-being—a Hoosier oncology group study. J Clin Oncol 21:2754–2759
Brady MJ, Peterman AH, Fitchett G, Mo M, Cella D (1999) A case for including spirituality in quality of life measurement in oncology. Psycho Oncology 8:417–428
Katzman R, Brown T, Fuld P, Peck A, Schechter R, Schimmel H (1983) Validation of a short Orientation-Memory-Concentration Test of cognitive impairment. Am J Psychiatry 140:734–739
Jordhoy MS, Fayers P, Loge JH, Ahlner-Elmqvist M, Kaasa S (2001) Quality of life in palliative cancer care: results from a cluster randomized trial. J Clin Oncol 19:3884–3894
Donner A, Piaggio G, Villar J, Pinol A, Al Mazrou Y, Ba'aqeel H et al (1998) Methodological considerations in the design of the WHO antenatal care randomized controlled trial. Paediatr Perinat Epidemiol 12(Suppl 2):59–74
Kronborg O, Fenger C, Olsen J, Jorgensen OD, Sondergaard O (1996) Randomized study of screening for colorectal cancer with faecal-occult blood test. Lancet 348:1467–1471
Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A et al (1993) The functional assessment of cancer therapy scale: development and validation of the general measure. J Clin Oncol 11:570–579
Webster K, Cella D, Yost K (2003) The Functional Assessment of Chronic Illness Therapy (FACIT) measurement system: properties, applications, and interpretation. Health Qual Life Outcomes 1(1):79
Cella D, Eton DT, Lai JS, Peterman AH, Merkel DE (2002) Combining anchor and distribution-based methods to derive minimal clinically important differences on the Functional Assessment of Cancer Therapy (FACT) anemia and fatigue scales. J Pain Symptom Manage 24:547–561
Yost KJ, Eton DT (2005) Combining distribution- and anchor-based approaches to determine minimally important differences: the FACIT experience. Eval Health Prof 28:172–191
Peterman AH, Fitchett G, Brady MJ, Hernandez L, Cella D (2002) Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy—Spiritual Well-being Scale (FACIT-Sp). Ann Behav Med 24:49–58
Edmondson D, Park CL, Blank TO, Fenster JR, Mills MA (2008) Deconstructing spiritual well-being: existential well-being and HRQOL in cancer survivors. Psycho Oncology 17:161–169
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Extermann M (2000) Measuring comorbidity in older cancer patients. Eur J Cancer 36:453–471
Statistics Canada. Ethnic Origin. http://www12.statcan.ca/english/census01/Products/Reference/dict/pop040.htm. 2002. Accessed 23 Dec 2009
Feinstein AR (1996) Multivariable analysis: an introduction. Yale University Press, New Haven
Hjermstad MJ, Fayers PM, Bjordal K, Kaasa S (1998) Using reference data on quality of life—the importance of adjusting for age and gender, exemplified by the EORTC QLQ-C30 (+3). Eur J Cancer 34:1381–1389
Exley C, Letherby G (2009) Managing a disrupted lifecourse: issues of identity and emotion work. Health 5:112–132
Rauch PK, Muriel AC (2004) The importance of parenting concerns among patients with cancer. Crit Rev Oncol Hematol 49(1):37–42
Mor V, Allen S, Malin M (1994) The psychosocial impact of cancer on older versus younger patients and their families. Cancer 74:2118–2127
Chow E, Abdolell M, Panzarella T, Harris K, Bezjak A, Warde P et al (2008) Predictive model for survival in patients with advanced cancer. J Clin Oncol 26:5863–5869
Nelson CJ, Rosenfeld B, Breitbart W, Galietta M (2002) Spirituality, religion, and depression in the terminally ill. Psychosomatics 43:213–220
Breitbart W (2002) Spirituality and meaning in supportive care: spirituality- and meaning-centered group psychotherapy interventions in advanced cancer. Support Care Cancer 10:272–280
Ando M, Morita T, Okamoto T, Ninosaka Y (2008) One-week short-term life review interview can improve spiritual well-being of terminally ill cancer patients. Psycho Oncology 17:885–890
Harrington SE, Smith TJ (2008) The role of chemotherapy at the end of life: "when is enough, enough?". JAMA 299:2667–2678
Hopwood P, Stephens RJ (2000) Depression in patients with lung cancer: prevalence and risk factors derived from quality-of-life data. J Clin Oncol 18:893–903
De Leeuw JR, de Graeff A, Ros WJ, Blijham GH, Hordijk GJ, Winnubst JA (2001) Prediction of depression 6 months to 3 years after treatment of head and neck cancer. Head Neck 23:892–898
Carlson LE, Angen M, Cullum J, Goodey E, Koopmans J, Lamont L et al (2004) High levels of untreated distress and fatigue in cancer patients. Br J Cancer 90:2297–2304
Strong V, Waters R, Hibberd C, Rush R, Cargill A, Storey D et al (2007) Emotional distress in cancer patients: the Edinburgh Cancer Center symptom study. Br J Cancer 96:868–874
Pascoe S, Edelman S, Kidman A (2000) Prevalence of psychological distress and use of support services by cancer patients at Sydney hospitals. Aust NZ J Psychiatry 34:785–791
Aass N, Fossa SD, Dahl AA, Moe TJ (1997) Prevalence of anxiety and depression in cancer patients seen at the Norwegian Radium Hospital. Eur J Cancer 33:1597–1604
Husain AF, Stewart K, Arseneault R, Moineddin R, Cellarius V, Librach SL et al (2007) Women experience higher levels of fatigue than men at the end of life: a longitudinal home palliative care study. J Pain Symptom Manage 33:389–397
Akechi T, Kugaya A, Okamura H, Yamawaki S, Uchitomi Y (1999) Fatigue and its associated factors in ambulatory cancer patients: a preliminary study. J Pain Symptom Manage 17:42–48
Redeker NS, Lev EL, Ruggiero J (2000) Insomnia, fatigue, anxiety, depression, and quality of life of cancer patients undergoing chemotherapy. Sch Inq Nurs Pract 14:275–290
Pater JL, Zee B, Palmer M, Johnston D, Osoba D (1997) Fatigue in patients with cancer: results with national cancer institute of canada clinical trials group studies employing the EORTC QLQ-C30. Support Care Cancer 5:410–413
Walsh D, Donnelly S, Rybicki L (2000) The symptoms of advanced cancer: relationship to age, gender, and performance status in 1,000 patients. Support Care Cancer 8:175–179
van Wijk CM, Kolk AM (1997) Sex differences in physical symptoms: the contribution of symptom perception theory. Soc Sci Med 45:231–246
Barsky AJ, Peekna HM, Borus JF (2001) Somatic symptom reporting in women and men. J Gen Intern Med 16:266–275
Cella D, Hahn EA, Dineen K (2002) Meaningful change in cancer-specific quality of life scores: differences between improvement and worsening. Qual Life Res 11:207–221
Wan GJ, Counte MA, Cella DF, Hernandez L, Deasy S, Shiomoto G (1999) An analysis of the impact of demographic, clinical, and social factors on health-related quality of life. Value Health 2:308–318
Jordhoy MS, Inger RG, Helbostad JL, Oldervoll L, Loge JH, Kaasa S (2007) Assessing physical functioning: a systematic review of quality of life measures developed for use in palliative care. Palliat Med 21:673–682
Acknowledgement
This research is funded by the Canadian Cancer Society (CCS Grant #017257 and #020509; CZ). The funding source had no role in the design, conduct, or preparation of the data, or in the preparation of the manuscript. This research was funded in part by the Ontario Ministry of Health and Long Term Care. The views expressed do not necessarily reflect those of the OMOHLTC. We are grateful to the patients who participated in this study, and to the clinical staff of the medical oncology clinics. Many thanks to Christopher Lo for his advice concerning statistical analyses.
Conflict of interest statement
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
This research is funded by the Canadian Cancer Society (CCS Grant #017257 and #020509; CZ). Results of this study were previously published/presented in part at the Multinational Association of Supportive Care in Cancer, 21st International Symposium, June 26-28, 2008, Houston, Texas.
Rights and permissions
About this article
Cite this article
Zimmermann, C., Burman, D., Swami, N. et al. Determinants of quality of life in patients with advanced cancer. Support Care Cancer 19, 621–629 (2011). https://doi.org/10.1007/s00520-010-0866-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-010-0866-1