Abstract
Goals of work
Certain patient and treatment characteristics are predictive of chemotherapy-induced nausea and vomiting (CINV). Objectives of this analysis were: (1) confirm the importance of several previously reported adverse risk factors for CINV in patients receiving chemotherapy, (2) assess the impact of the NK1 receptor antagonist aprepitant according to these risk factors, and (3) assess the impact of age on antiemetic outcome.
Patients and methods
Patients from two double-blind, placebo-controlled trials were randomized to an active-control group (ondansetron 32 mg IV, dexamethasone 20 mg PO day 1; dexamethasone 8 mg bid days 2–4) or an aprepitant group (aprepitant 125 mg PO, ondansetron 32 mg IV, dexamethasone 12 mg day 1; aprepitant 80 mg days 2–3; dexamethasone 8 mg qd days 2–4). The primary endpoint was complete response (no emesis or rescue therapy use). In a post-hoc analysis, multivariate logistic regression models were used to assess the impact of treatment with aprepitant and previously reported risk factors, using a modified intent-to-treat approach.
Main results
Treatment with aprepitant (p < 0.0001), male gender (p = 0.023), cisplatin dose <80 mg/m2 (p = 0.001), age ≥65 years (p = 0.021), and five or more alcoholic drinks per week (p = 0.027) were all significantly associated with improved complete response. Aprepitant improved complete response regardless of risk for all factors and neutralized the risk associated with female gender.
Conclusions
This analysis confirmed the relevance of several previously reported risk factors for CINV in patients receiving chemotherapy. Aprepitant improved complete response regardless of risk and eliminated the increased risk of CINV associated with the female gender.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients undergoing treatment with chemotherapy for cancer have consistently listed nausea and vomiting (CINV) as among the most troublesome and widely feared side-effects [14]. Significant progress has been realized over the past two decades in the development of effective and well-tolerated means to prevent nausea and vomiting in a majority of patients receiving emetogenic chemotherapy. Retrospective analyses conducted with some of the earliest antiemetic trials identified a number of patient and treatment characteristics that appeared to have predictive value for the development of CINV [2, 6, 10, 15]. Subsequent trials evaluating a variety of type 3 five-hydroxytryptamine (5-HT3) receptor antagonists have for the most part confirmed the predictive value of such factors as age, gender, alcohol use, history of motion sickness, and dose of cisplatin [1, 4, 8, 13]. Several of these trials have been relatively small in size which has limited the power of the predictive factor analysis.
In recent years, the first representative of a new class of antiemetics, the neurokinin-1 (NK1) receptor antagonists has been introduced into clinical practice. The NK1 receptor antagonist aprepitant, combined with dexamethasone and the 5-HT3 receptor antagonist ondansetron, has been shown to improve the control of CINV in the setting of both highly emetogenic (cisplatin-based) and moderately emetogenic (anthracycline+cyclophosphamide) chemotherapy [5, 9, 17].
The first two reported phase III trials of aprepitant in highly emetogenic chemotherapy provide an opportunity to study the previously described predictive factors employing a database of over 1,000 patients [5, 9]. This robust sample also allows assessment of the impact of aprepitant on these risk factors. The trials also provide an opportunity to study the impact of age in greater depth. Several prior analyses have found that age younger than 40 or 50 years is an important factor in predicting higher risk for CINV [1, 10, 12]. None of these studies, however, have been able to investigate whether this is an effect associated with younger patients only, or if this risk diminishes progressively with increasing age. In this manuscript, we have sought to confirm the importance of a number of adverse factors for CINV in patients receiving cisplatin-based chemotherapy and to assess the impact of the NK1 receptor antagonist aprepitant according to these risk factors.
Patients and methods
Design
Two identically designed phase III, multicenter, randomized, double-blind, parallel-group, placebo-controlled trials were conducted. Written informed consent to participate was obtained from every patient and was approved by the institutional review board of each participating site. All study procedures were followed in accordance with applicable ethical requirements. Detailed descriptions of the design (including enrollment criteria), as well as the primary efficacy and tolerability results of the individual studies, are published elsewhere [5, 9].
Patients
The studies enrolled cisplatin-naive patients who were scheduled to receive their first cycle of chemotherapy including cisplatin ≥70 mg/m2. Patients were randomized to one of two treatment groups: patients in the active-control group received intravenous ondansetron 32 mg and oral dexamethasone 20 mg on day 1, followed by oral dexamethasone 8 mg twice daily on days 2–4; patients in the aprepitant-containing group received oral aprepitant 125 mg on day 1 and 80 mg on days 2 and 3, intravenous ondansetron 32 mg, and oral dexamethasone 12 mg on day 1 and 8 mg daily on days 2–4. Matching placebos were given to maintain blinding. Patients were given a take-home prescription of rescue antiemetics to be used as needed in case of nausea or vomiting.
Assessments and statistical analysis
On the first 5 days after receiving chemotherapy, patients used a diary to record the occurrence of emetic episodes, any use of rescue therapy, and daily ratings of nausea severity using a 100-mm horizontal visual analog scale. The study sponsor (Merck Research Laboratories) managed the data and performed analysis, and investigators had access to the data. The primary endpoint was complete response (defined as no emetic episodes and no rescue therapy) in the overall 5-day study period. Since anticipatory nausea and vomiting is an important risk factor that could impact results in subsequent cycles, only cycle 1 was studied in this analysis.
An analysis of combined data from the two clinical trials was prespecified. The modified intent-to-treat analysis included all patients who received cisplatin, took study drug, and had at least one posttreatment assessment. In a post-hoc analysis, the impact on complete response of treatment with aprepitant, and a number of prespecified risk factors, including gender, age (<65 and ≥65 years), alcohol use (0 to four drinks per week and five or more drinks per week), and cisplatin dose (<80 mg/m2 and ≥80 mg/m2) was assessed. The cut-off of 65 years for age was chosen based on protocol-specified subgroup summaries. The cut-off for alcohol was chosen because four drinks per week represents a low level of alcohol intake; it was also felt that higher cut points may actually represent higher alcohol usage due to suspected under-reporting of alcohol use in these studies. A higher cut-off of, for example, ten drinks per week would have also represented a very small number of patients. The cut-off for cisplatin dose of 80 mg/m2 was chosen based on the mean dose in the study. A number of other possible risk factors, including body mass index, history of motion sickness, history of chemotherapy, and history of chemotherapy-induced nausea and vomiting, were not included as they were eliminated in a stepwise logistic regression which retained factors having a significant impact on complete response. We also conducted a post-hoc analysis of the combined data set stratified by age (<60, 60–65, 65–70, and >70 years) in order to investigate the impact of older age on complete response. Logistic regression models were used for all treatment comparisons, using SAS v.9.1.3 (SAS Institute, Cary, NC, USA). Since this was a post-hoc analysis, analysis was conducted only on the primary endpoint of complete response (no emesis and no rescue therapy). No adjustment for multiple comparisons was applied and p values reported are nominal.
Results
Patient characteristics
Overall, 1,043 patients were included in these post-hoc analyses. Of these, 435 (42%) were women and the mean age was 56 years. The mean cisplatin dose was 80 mg/m2. Baseline characteristics of patients included in the analysis are shown in Table 1. It can be seen that there were no significant differences between arms, including the proportion of patients with different types of cancer and the proportion receiving concomitant emetogenic chemotherapy in addition to cisplatin. Importantly, the proportion of patients with known risk factors for CINV was similar across arms.
Figure 1 shows the complete response rates in the aprepitant-containing arm and the active-control arm for each of the prespecified risk factors studied. In a multivariate analysis including terms for treatment with aprepitant, age, gender, alcohol use, and cisplatin dose, the most significant factor impacting complete response was treatment with aprepitant (p < 0.0001). This is consistent with the primary analysis of this combined data set as described by Warr et al [16], in which 68% of patients in the aprepitant-containing arm achieved complete response compared with 48% in the active-control arm (p < 0.001). However, each of the prespecified risk factors included in the model also proved to have a statistically significant impact on complete response rates. Male gender (p = 0.023), lower cisplatin dose (p = 0.001), older age (p = 0.021), and alcohol use (p = 0.027) were all significantly associated with an increased likelihood of achieving complete response. Figure 2 shows the odds ratio of complete response for patients receiving an aprepitant-containing antiemetic regimen compared with active control for low-risk groups (Fig. 2a) and high-risk groups (Fig. 2b). Regardless of whether patients were in a low-risk group or a high-risk group, addition of aprepitant was associated with a statistically significant improvement in complete response rate for all the risk factors studied.
Percentage of patients with complete response (no emesis and no use of rescue therapy) in the overall phase (days 1–5), by treatment group (data combined from two identically designed phase III studies. Stratified by: a gender, b cisplatin dose, c alcohol use, and d age. Asterisk p < 0.0001 for aprepitant regimen vs. active control regimen. Dagger p < 0.017 for aprepitant regimen vs. active control regimen. Double dagger p < 0.016 for aprepitant regimen vs. active control regimen
Forest plot showing the odds ratio (± 95% confidence intervals) for complete response (no emesis and no use of rescue therapy) in the overall phase (days 1–5) for patients receiving an aprepitant-containing antiemetic regimen compared to the active-control regimen for low-risk groups (a) and high-risk groups (b)
Given the high complete response rates in patients receiving aprepitant in all risk groups, we compared the relative impact of aprepitant and active control in the high- and low-risk groups to determine if aprepitant was able to lessen the impact of these risk factors. Table 2 shows the relative risk of achieving complete response for high- and low-risk groups for the aprepitant-containing and active-control groups. The relative risk for high risk and low risk was significantly different for all risk factors in both groups, except for gender in the aprepitant-containing group (p = 0.54) and age in the active-control group (p = 0.073). In the active-control group, only 40.6% of women achieved complete response, compared with 52.9% of men (p = 0.005 for difference); however, in the aprepitant-containing group, the complete response rate was 66.2% for women and 68.9% for men (p = 0.54), indicating that inclusion of aprepitant-eliminated gender as a risk factor for nausea and vomiting in this population. Although there was a significant difference in complete response rate in the aprepitant-containing group between those receiving cisplatin <80 mg/m2 and ≥80 mg/m2, and between those using five or more alcoholic drinks per week and 0 to four drinks per week, there was a trend towards a greater relative improvement in complete response in the high-risk groups with aprepitant compared with active control for these two risk factors, as evidenced by a smaller relative risk ratio (Table 2). For age <65 and ≥65 years, there was no difference in relative improvement in complete response rate between the aprepitant-containing and active-control arms.
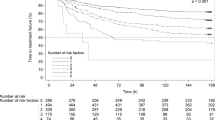
The combined study population included 124 patients over 70 years of age, affording an opportunity to further investigate the impact of older age on the risk of CINV. The population was divided into three age strata: <60, 60–65, 65–70, and >70 years. There were no significant differences in baseline characteristics across the four age strata, all being similar to the overall population. The complete response rates for each of the age strata are shown in Fig. 3a. The complete response rate was significantly greater for the aprepitant-containing arm than the active-control arm, regardless of age (Fig. 3b). Multivariate logistic regression demonstrated a significant age effect in the overall population (p = 0.006); however, when considered separately, the aprepitant-containing arm and the active-control arm did not reach statistical significance (p = 0.070 and p = 0.106, respectively). Figure 3a suggests a trend for higher complete response rates with increasing age, most evident in the aprepitant group. However, this effect was not statistically significant, with univariate contrast analysis demonstrating no difference in complete response rate between patients >70 years of age and those 60–65 (p = 0.747) and 65–70 years (p = 0.451). There was a significant difference in complete response rates between younger patients <60 years of age and older patients 65–70 years (p = 0.018) and >70 years of age (p = 0.004).
a Percentage of patients with complete response (no emesis and no use of rescue therapy) in the overall phase (days 1–5), stratified by age, < 60, 60–65, 65–70 and > 70 years. b Forest plot showing odds ratio (± 95% confidence intervals) for complete response (no emesis and no use of rescue therapy) in the overall phase (days 1–5) for patients receiving an aprepitant-containing antiemetic regimen compared with the active-control regimen for different age strata
Discussion
The multivariate analysis described here has confirmed the importance of age, gender, alcohol use, and cisplatin dose as prognostic risk factors for CINV. Younger age, female gender, light or no alcohol use, and higher cisplatin dose were all associated with worse outcome in terms of complete response to antiemetic therapy. A number of other previously identified risk factors for CINV were not included in this analysis because they were eliminated from a stepwise logistic regression designed to keep only those factors that met the statistical threshold. These included history of motion sickness, history of vomiting associated with pregnancy, history of prior chemotherapy, and history of CINV. It is possible that while these factors may be important in some populations, they were unimportant in this study compared with the stronger associations seen with the factors kept in the model, possibly due to interaction with factors such as gender. Although prior studies have each identified some of these predictive factors for CINV [1, 2, 6, 8, 10, 13, 15], this analysis confirmed the importance of all of these risk factors for the first time in a single-study population. The data presented here further demonstrates that regardless of whether patients were in a low-risk or high-risk group, addition of aprepitant was associated with a statistically significant improvement in complete response rate for all the risk factors studied.
We also attempted in this analysis to determine whether the relative risk of achieving a complete response in the high- vs. low-risk groups could be affected by the addition of aprepitant. With gender, the negative impact of female gender was negated in the aprepitant group. Complete response rates were not significantly different in men compared with women in those receiving aprepitant (68.9% vs. 66.2%, p = 0.54, respectively). This finding implies that women may derive a greater degree of benefit than men from the addition of aprepitant. Nevertheless, men still significantly benefited as well from treatment with aprepitant (p < 0.0001).
A similar trend was seen with cisplatin dose and alcohol use. Although significant differences between high- and low-risk groups were maintained, the relative risk associated with higher cisplatin dose and light or no alcohol use was reduced for patients receiving an aprepitant-containing regimen. The relative risk associated with younger age was not impacted by the addition of aprepitant.
Younger age has long been recognized as a prognostic risk factor for CINV [10]. The large size of our study population permitted an exploratory analysis of the possible impact of advancing age on antiemetic outcome. It has been suggested that confounding factors such as reduced chemotherapy dose in older patients explain the identification of age as a prognostic factor [15]. In this study, however, the correlation between age and cisplatin dose was weak, although statistically significant (R 2 = 0.103, p < 0.0001; data not shown); this likely reached statistical significance due to the more than 1,000 patients in the data set. Although there appeared to be a trend toward better complete response with increasing age, there was no significant difference between patients >70 years of age and those 60–65 and 65–70 years of age. However, there was a significant difference in complete response between the two highest age strata and the <60 years stratum. As the population of cancer patients continues to age, it is likely that larger numbers of older patients will be included in future antiemetic trials. Further insights into the possible impact of advancing age on antiemetic outcome may be obtained from these trials.
In summary, this study has confirmed the importance of a number of risk factors, including age, gender, alcohol use, and cisplatin dose, for predicting the development of CINV in patients receiving cisplatin-based therapy. The NK1 receptor antagonist aprepitant improved complete response rates in all patients, regardless of which risk factors were present, and completely neutralized the excess risk of CINV associated with female gender. These results support the recommendations of current treatment guidelines [3, 7, 11] that aprepitant be included in the antiemetic regimen for all patients receiving highly emetogenic chemotherapy.
References
Booth CM, Clemons M, Dranitsaris G, Joy A, Young S, Callaghan W, Trudeau M, Petrella T (2007) Chemotherapy-induced nausea and vomiting in breast cancer patients: a prospective observational study. J Support Oncol 5:374–380
D’Acquisto R, Tyson LB, Gralla RJ (1986) The influence of a chronic high alcohol intake on chemotherapy-induced nausea and vomiting. Proc Am Soc Clin Oncol 5:257
Herrstedt J, Roila F (2008) Chemotherapy-induced nausea and vomiting: ESMO clinical recommendations for prophylaxis. Ann Oncol 19(Suppl 2):ii110–ii112
Hesketh PJ (1999) Defining the emetogenicity of cancer chemotherapy regimens: relevance to clinical practice. Oncologist 4:191–196
Hesketh PJ, Grunberg SM, Gralla RJ, Warr DG, Roila F, de Wit R, Chawla SP, Carides AD, Ianus J, Elmer ME, Evans JK, Beck K, Reines S, Horgan KJ (2003) The oral neurokinin-1 antagonist aprepitant for the prevention of chemotherapy-induced nausea and vomiting: a multinational, randomized, double-blind, placebo-controlled trial in patients receiving high-dose cisplatin—the aprepitant protocol 052 study group. J Clin Oncol 21:4112–4119
Hesketh PJ, Plagge P, Bryson JC (1992) Single-dose ondansetron for prevention of acute cisplatin-induced emesis: analysis of efficacy and prognostic factors. In: Bianchi AL, Grelot L, Miller AD (eds) Mechanisms and control of emesis. Libbey, London, pp 25–26
Kris MG, Hesketh PJ, Somerfield MR, Feyer P, Clark-Snow R, Koeller JM, Morrow GR, Chinnery LW, Chesney MJ, Gralla RJ, Grunberg SM (2006) American Society of Clinical Oncology guideline for antiemetics in oncology: update 2006. J Clin Oncol 24:2932–2947
Osoba D, Zee B, Pater J, Warr D, Latreille J, Kaizer L (1997) Determinants of postchemotherapy nausea and vomiting in patients with cancer. Quality of Life and Symptom Control Committees of the National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol 15:116–123
Poli-Bigelli S, Rodrigues-Pereira J, Carides AD, Julie Ma G, Eldridge K, Hipple A, Evans JK, Horgan KJ, Lawson F (2003) Addition of the neurokinin 1 receptor antagonist aprepitant to standard antiemetic therapy improves control of chemotherapy-induced nausea and vomiting. Results from a randomized, double-blind, placebo-controlled trial in Latin America. Cancer 97:3090–3098
Pollera CF, Giannarelli D (1989) Prognostic factors influencing cisplatin-induced emesis. Definition and validation of a predictive logistic model. Cancer 64:1117–1122
Roila F, Hesketh PJ, Herrstedt J (2006) Prevention of chemotherapy- and radiotherapy-induced emesis: results of the 2004 Perugia International Antiemetic Consensus Conference. Ann Oncol 17:20–28
Roila F, Tonato M, Basurto C, Picciafuoco M, Bracarda S, Donati D, Malacarne P, Monici L, Di Costanzo F, Patoia L et al (1989) Protection from nausea and vomiting in cisplatin-treated patients: high-dose metoclopramide combined with methylprednisolone versus metoclopramide combined with dexamethasone and diphenhydramine: a study of the Italian oncology group for clinical research. J Clin Oncol 7:1693–1700
Schwartzberg LS (2007) Chemotherapy-induced nausea and vomiting: clinician and patient perspectives. J Support Oncol 5:5–12
Sun CC, Bodurka DC, Weaver CB, Rasu R, Wolf JK, Bevers MW, Smith JA, Wharton JT, Rubenstein EB (2005) Rankings and symptom assessments of side effects from chemotherapy: insights from experienced patients with ovarian cancer. Support Care Cancer 13:219–227
Tonato M, Roila F, Del Favero A (1991) Methodology of antiemetic trials: a review. Ann Oncol 2:107–114
Warr DG, Grunberg SM, Gralla RJ, Hesketh PJ, Roila F, Wit R, Carides AD, Taylor A, Evans JK, Horgan KJ (2005) The oral NK(1) antagonist aprepitant for the prevention of acute and delayed chemotherapy-induced nausea and vomiting: pooled data from 2 randomised, double-blind, placebo controlled trials. Eur J Cancer 41:1278–1285
Warr DG, Hesketh PJ, Gralla RJ, Muss HB, Herrstedt J, Eisenberg PD, Raftopoulos H, Grunberg SM, Gabriel M, Rodgers A, Bohidar N, Klinger G, Hustad CM, Horgan KJ, Skobieranda F (2005) Efficacy and tolerability of aprepitant for the prevention of chemotherapy-induced nausea and vomiting in patients with breast cancer after moderately emetogenic chemotherapy. J Clin Oncol 23:2822–2830
Disclosures
Paul Hesketh is a consultant and has received research funding from Merck & Co. and GlaxoSmithKline, and has received honoraria from Merck & Co.
Matti Aapro is a consultant and has received research funding and honoraria from Merck & Co.
James Street is a paid consultant to Merck & Co.
Alexandra Carides is an employee of Merck Research Labs.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hesketh, P.J., Aapro, M., Street, J.C. et al. Evaluation of risk factors predictive of nausea and vomiting with current standard-of-care antiemetic treatment: analysis of two phase III trials of aprepitant in patients receiving cisplatin-based chemotherapy. Support Care Cancer 18, 1171–1177 (2010). https://doi.org/10.1007/s00520-009-0737-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-009-0737-9