Abstract
Goals of work
Genetic counseling for hereditary cancer is expected to involve a growing number of individuals in the near future since an increasing number of genetic tests are offered. This study was designed to identify psychosocial variables predicting distress after genetic investigation and genetic counseling (GC) in order to develop new counseling strategies.
Materials and methods
A prospective multi-site study was undertaken on 214 patients undergoing GC for hereditary cancer to explore the relationships between socio-demographic variables, medical variables, social support, self-efficacy, physical functioning, satisfaction with GC, the level of worry after GC, results of genetic testing, and the course and outcomes of distress. Distress was measured with the Impact of Event Scale, which includes subscales of intrusion and avoidance. Patients completed questionnaires mailed to them before and after GC.
Main results
The mean level of intrusion and avoidance was moderate, even though one quarter of participants reported a severe level of intrusion at baseline. Subjects with a low level of self-efficacy at baseline and high level of worry immediately after GC seemed to be vulnerable to both intrusion and avoidance. Lower level of intrusion was also associated with having a first-degree relative with cancer, while a lower avoidance level was associated with a higher level of education, having cancer, more social support, and higher satisfaction with GC.
Conclusions
In this study, subjects who had lower level of self-efficacy at baseline and a high level of worry immediately after GC seemed to be vulnerable to both intrusion and avoidance in this study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Much has been published about an individual’s reactions to becoming ill with a serious disease such as cancer [2, 22, 26, 39] or other potentially life-threatening diseases [8, 35]. Being diagnosed with a life-threatening disease such as cancer is considered a traumatic life event [18] similar to the stressor in posttraumatic stress disorder (PTSD; the Diagnostic and Statistical Manual of Mental Disorders 4th Ed. DSM IV) [1]. Using information gained from in-depth evaluation and psychotherapy sessions, Horowitz abstracted two basic reactions to a wide range of traumatic events as follows: “Intrusion was characterized by unbidden thoughts and images, troubled dreams, strong pangs or waves of feelings, and repetitive behavior. Avoidance responses included ideational constriction, denial of the meanings and consequences of the event, blunted sensation, behavioral inhibition or counterphobic activity, and awareness of emotional numbness” [16, p. 210]. These reactions can be associated with other stress reactions, psychiatric symptoms, and changes in function, which can lead to the diagnosis of PTSD. They can also be studied as reactions to actual or potential threatening events without implicating a diagnosis of PTSD, as in the present study.
Information about the possibility of future cancer is one of the core elements of genetic counseling (GC) and testing, and these interventions are also important from a health promoting perspective. On the other hand, GC can cause uncertainty about potentially threatening implications, and this uncertainty can be a strong stressor [24] that may lead to an increased level of distress, activating intrusion or avoidance or both.
We need to learn more about possible stress-related reactions such as intrusion and avoidance and to identify individual and situational characteristics that might be related to these reactions. We also need to know more about the psychological implications and consequences of learning this information.
In this study, the symptoms of intrusion and avoidance were measured with Horowitz’s Impact of Event Scale –15 (IES). Others have used this scale in research related to GC for hereditary cancer. Several of these studies have reported moderate levels of intrusion and avoidance in connection with GC [4, 13, 29, 34, 42]. In a prospective study of women undergoing predictive genetic testing for Breast Cancer 1 and 2 genes (BRCA1/2), the mean IES scores were within the moderately elevated level both before genetic testing and 1 year after disclosure of the test results [9]. The total IES score decreased from baseline to follow-up, both for breast and ovarian cancer distress respectively. In addition, there were no differences between carrier of a mutated cancer gene and the noncarrier.
In women undergoing genetic testing for BRCA1 mutations, a cancer diagnosis was associated with higher levels of intrusion and avoidance [29]. The total IES score decreased in noncarriers from before to after the test [9]. Other studies indicate that a relative’s health status is related to intrusion and avoidance; for example, having a first-degree relative with colorectal disease predicted a higher level of distress about colorectal cancer, as measured by the IES [31].
In a sample of colorectal cancer survivors undergoing genetic testing for hereditary nonpolyposis colorectal cancer (HNPCC), higher levels of intrusion and avoidance assessed after the GC were related to less social support and an avoidant coping style [12]. Greater social support was also related to a lower level of avoidance 2 months after baseline assessment in patients with terminal cancer [30].
Research on stress and coping has demonstrated that self-efficacy is an important predictor of the level of distress after a wide range of demanding life events [3]. A lower level of cancer-specific self-efficacy was related to a higher level of intrusion and avoidance among women recently diagnosed with breast cancer [21].
Researchers are increasingly interested in participants’ satisfaction with a counseling program, and satisfaction should be studied in relation to the outcomes of GC [11, 19, 25]. The level of worry associated with GC and physical health is related to the outcome in GC [5, 15, 17, 46], but we do not have scientific knowledge about how satisfaction with the counseling program is related to avoidance and intrusion.
The present study used an empirical approach, and our goal was to explore the course and outcome of genetic counseling. The particular variables and questionnaires used in the present study were chosen based on earlier studies, clinical knowledge of genetic counseling, and medical genetics.
To our knowledge, there seem to be few longitudinal studies of the relationship between intrusion and avoidance in subjects undergoing GC for hereditary cancer and even fewer involving follow-up of 1 year or longer [4, 9, 29]. It is important to monitor subjects undergoing GC in order understand the psychological effects of GC and to develop new strategies given the complex future of counseling expected to result from increasing use of genetic testing.
The aims of this study were:
-
1.
To investigate the level of intrusion and avoidance in subjects undergoing GC for hereditary cancer and to evaluate any changes occurring during the study period of 1 year after GC and
-
2.
To explore the possible relationship between socio-demographic variables (age, gender, education level, cohabiting status, having children), medical variables (having cancer themselves, having a first-degree relative with cancer, result of gene tests, physical functioning), psychosocial variables (social support, GC-specific self-efficacy, satisfaction with the GC session, the level of worry after GC), and the course and outcomes of intrusion and avoidance.
Materials and methods
Study design and procedures
A prospective multi-site study was undertaken involving subjects undergoing GC for hereditary cancer. Questionnaires were mailed to the participants before and after the GC session. The main questionnaire in this paper (IES-15) was administered to the subjects 2 weeks before GC (T1, baseline), 4 weeks after GC (T4), 6 months after GC (T5), and 1 year after GC (T6). Data were also collected from the subjects immediately before GC (T2) and immediately after GC (T3). These data were not relevant for the present study, except for the assessment of worry related to the counseling session and the satisfaction with the GC session (T3), which we adjusted for in the regression analysis.
Participants provided written informed consent. The Regional Committee for Medical Research Ethics, Western Norway, and The National Data Inspectorate approved the study.
Study sample
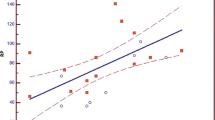
The study procedures and the sample population are described elsewhere [6] and will be outlined only briefly here. Participants were recruited consecutively from the genetic outpatient clinics at three university hospitals in Norway from October 2002 to January 2004. The inclusion criteria were first-time counselees over 18 years of age and with at least one first- or second-degree relative (through males) with breast and ovarian cancer or colorectal cancer or both. From 275 eligible subjects, 214 (77.8%) agreed to participate and answered the baseline questionnaire (T1). Information about the participants at the various data collection times, dropouts, and nonresponders is presented in Fig. 1.
Flow chart of participation. The beginning of the circular arrows to the left indicates the number of nonresponders at that data collection point, and the end of the arrow indicates the data collection point when they next responded. The arrows to the right indicate the number of permanent dropouts at the time
The GC protocol
All participants were counseled according to the same protocol that is described by Bjorvatn et al. [6, 7]. In Norway, the counseling session and the surveillance program are closely linked, and all genetic counseling sessions are held by trained staff at a department of medical genetics. The departments of medical genetics refer the patients to various surveillance programs after GC if appropriate. Results from such surveillance consultations are reported back to medical genetics. Thus, a GC session is a “package” comprising counseling, having a contact person (counselor or physician) for the follow-up after the genetic counseling and the possibility of enrolment in a surveillance program. Patients not attending the recommended surveillance program are re-contacted by the department of medical genetics for new appointment. Thus, the participation in the various surveillance programs is almost 100%.
Some patients did also undergo genetic testing for six known mutations in the BRCA1 gene. Those individuals received their test results in a counseling session between T4 and T5. After GC, subjects were included in a surveillance program if they met the following criteria. For breast and ovarian cancer, inclusion was based on the Biomed 2 Demonstration Program. A subject was included in the surveillance program if she had a family history of two or more first-degree relatives with early onset of breast cancer (<50 years of age), and/or multiple cases of breast cancer in the same lineage compatible with dominant inheritance in the family, and/or a combination of early onset breast cancer and ovarian cancer in the family [23]. Inclusion in the HNPCC surveillance program was based on the Amsterdam I criteria. Subjects were included if three relatives had colorectal cancer; one of whom was a first-degree relative of the other two, involving at least two generations, and if one or more cases were diagnosed before the age of 50 years [43]. Individuals who met the Amsterdam criteria II [44] were also offered inclusion in the surveillance program. The Amsterdam II criteria extend the Amsterdam I criteria to include cancers of the endometrium, small intestine, urether, and renal pelvis. We used the modified Amsterdam criteria for smaller families [32].
Individuals not included in a surveillance program were either too young to be included or males in HBOC families.
Study measurements
Predictor variables assessed before GC (baseline, T1)
Sociodemographic and medical variables
Information about age, gender, cohabiting status, number of children, and level of education was collected together with information about each subject’s cancer diagnosis, as well as the diagnoses of first-degree relatives with cancer.
Social support
Social support was measured with the Interpersonal Support Evaluation List (ISEL) [20]. ISEL comprises 30 items that are answered on a four-point scale (range 1–4). The average sum score of ISEL was used. The reliability of the ISEL, estimated by Cronbach’s alpha, was 0.92.
Self-efficacy
A GC-specific self-efficacy scale, the Bergen Genetic Counseling Self-Efficacy Scale, was developed for this study using Bandura’s Guidelines for Constructing Self-efficacy Scales, (undated) Albert Bandura, Stanford University, Palo Alto, CA, USA. The scale was developed by a panel of medical geneticists, genetic counselors, and psychologists and was piloted by genetic counselors in a clinical setting [6]. The scale comprises 20 items describing tasks and challenges that are likely to occur during and after GC, and the individual’s beliefs that he or she would be able to cope with these. The items cover self-efficacy beliefs related to the counseling session, including the ability to process and remember the information given (e.g., “Understand what the counselor is explaining”) and to maintain emotional control (e.g., “Not becoming worried, scared, or frightened”), and self-efficacy beliefs related to the consequences of the counseling session (e.g., “Being able to tell the others in the family about the participant’s own risk of cancer”). Each item was rated on a scale from 0 to 10 (0 = cannot do at all, 10 = can do without difficulty). The average total sum score of the GC-specific self-efficacy scale (range 0–10) was used. The reliability of the scale, estimated by Cronbach’s alpha, was 0.95.
Physical functioning
Self-rated physical functioning was assessed with the Physical Functioning (PF) subscale from the acute version of the Short Form-36 Health Survey (SF-36) with a 1-week recall period [45]. PF comprises ten items covering the limitations in physical functioning in daily life that are not specific to age, disease, or treatment. Raw scores were linearly transformed to a scale ranging from 0 (worst physical functioning) to 100 (best possible physical functioning). Cronbach’s alpha for the PF subscale was 0.88 in this sample.
Predictor variables assessed immediately after GC (T3) and 6 months after GC (T5)
Satisfaction with GC at T3
The patients completed the Satisfaction with Genetic Counseling Scale immediately after the counseling session [36]. This scale comprises three subscales: instrumental satisfaction, affective satisfaction, and procedural satisfaction, each with three items. The response format was from 1 = “not at all satisfied” to 4 = “as satisfied as possible” for all items [25, 36]. Cronbach’s alpha for the subscales were as follows: procedural, 0.54; instrumental, 0.58; and affective, 0.70.
Level of GC-related worry at T3
The patients’ worry related to the GC session was assessed on a seven-point single-item scale immediately following the counseling session (1 = no worry at all, 7 = worst possible worry) [25]. The worry question was designed to measure the state of worry related to the GC session.
Results of genetic testing at T5
The results of genetic testing were collected from the hospital records by medical staff. The subjects undergoing genetic testing had received their results between T4 and T5.
Outcome variable
The IES was filled in by participants at T1, T4, T5, and T6. The IES is a 15-item questionnaire comprising two subscales: intrusion (IES-I), which includes seven items and is scored from 0 to 35, and avoidance (IES-A), which consists of eight items, and is scored from 0 to 40. The scale was developed to measure stress reactions after a specific traumatic event [16]. We defined “cancer disease” as the specific traumatic event for this scale. Subsequently, the subjects may incorporate their own experiences of cancer diseases into the concept. The introduction of the questionnaire sets the context of hereditary cancer and how the subjects perceive their situation when undergoing GC. A subscale scores of 0–8 is considered low, 9–19 is considered moderate, and 20 or greater is considered severe [16]. IES is used widely as a measure of event-related distress [37] and within the context of GC for hereditary cancer [4, 29, 38]. In our study, reliability values for the IES-I and IES-A, estimated with Cronbach’s alpha, were 0.93 and 0.87.
Statistical methods
The paired sample t test was used to analyze the changes in mean values of the IES-I and IES-A. McNemar’s exact test was used to analyze the changes in the proportion of individuals with high scores on intrusion and avoidance from T1 to T6 and T4 to T5. These tests were done to give a crude comparison of the overall changes in IES-I and IES-A from start to end. To test for differences between the participants who completed the study and dropouts, we used the Mann–Whitney’s U test or an independent-sample t test for continuous variables and Pearson’s exact χ 2 test for categorical variables.
To identify the characteristics related to the IES-I and IES-A and to test the changes of IES-I and IES-A during the study period, the subscale scores were regressed on the selected predictor variables using the mixed linear model module of SPSS 15.0. The mixed linear model uses all available data and can account for correlations between repeated measurements on the same subjects and has sufficient flexibility to model time effects [14]. The predictors were entered into the mixed linear models to assess both main effects and possible interactions with time. The set of predictors comprised the following variables. At T1, the variables were age, gender, having children, cohabiting status, educational level, having cancer, a first-degree relative with cancer, social support, GC-specific self-efficacy, and SF-36 PF. At T3, the variables were satisfaction with the GC session (instrumental, affective, and procedural) and the level of worry, and at T5, the one variable was the results of genetic testing.
The regression analyses were run stepwise, both with and without interactions with time. First, we performed a backward elimination of all variables with insignificant main effects, and then we ran a forward selection of variables with significant main effect on IES-I and IES-A. To cross-validate the findings, we also ran a stepwise forward procedure on the main effects (not reported here).
A two-tailed significance level of α = 0.10 was used in the mixed linear model analysis because we considered it important not to prematurely reject variables from further investigation in an exploratory study like this.
Missing values were replaced by the individual’s own average score for each questionnaire if 60% or more of the items were answered. All statistical analyses were performed using SPSS 15.0.
Results
Study sample
The baseline characteristics of the study sample are presented in Table 1. The mean age was 42 years (range 18–80 years), and most of the participants were women. The rate of unemployment was low (1.4%). Half the sample was self-referred and only 10% had cancer themselves. On average, the participants reported high levels of social support and self-efficacy and good self-rated physical functioning. Satisfaction with the GC session was also high. A total of 103 individuals were offered inclusion in one of the surveillance programs immediately after the GC session.
The dropouts did not differ significantly on any of the baseline variables except that more of the dropouts had cancer (n = 11/65, 17%) compared with the study sample (n = 22/214, 10%; P = 0.046).
Level of intrusion (IES-I) and avoidance (IES-A) during the study period
The mean levels of both IES-I and IES-A were highest at baseline and had decreased at the follow-up 1 year after GC (P < 0.0001 and P = 0.006, respectively, paired t test; Table 2).
The lowest average scores for IES-I and IES-A were observed 2 weeks after the GC (T4).
The proportion of persons with an IES-I score indicating a severe response decreased from baseline (T1) to the 1-year follow-up (T6; P < 0.001, McNemar’s exact test). In contrast, the proportion of participants with an IES-A score at the severe level was low and stable during the same period (P = 0.27, McNemar exact test). However, the number of participants with scores at the severe level on both IES-I and IES-A increased significantly from 4 weeks after GC (T4) to 6 months after (T5) P = 0.001, and P = 0.039 McNemar exact test, respectively (Table 2). The inter-correlations between IES-I and IES-A scores at the different times were high, ranging from 0.66 (T1) to 0.76 (T5).
Mixed linear models for intrusion (IES-I) and avoidance (IES-A)
The results of the stepwise selection process for IES-I score are given in Table 3. After 13 backward steps, the final mixed linear model showed that the average level of IES-I varied with time. The level of intrusion was lower if the participants had a first-degree relative with cancer, higher level of GC-specific self-efficacy at baseline, and lower level of worry immediately after the GC. For example, this means that one point increase in worry will result in 2.36 point increase in IES-I. The effect of GC-specific self-efficacy on intrusion showed a significant interaction with time and was strongest at 6 months and 1 year after GC. For example, this means that at T5, one point increase in CG-specific self-efficacy at baseline gives a 1.13 points decrease in IES-I, while at T4, this decrease is only 0.25 points. The following variables were not retained in the final model: age, gender, having children, cohabiting status, educational level, having cancer themselves, social support, physical function, satisfaction with GC (instrumental, affective, procedural), and the result of genetic testing.
The results of the stepwise selection process for the IES-A are reported in Table 4. The average IES-A score also varied with time, and a lower IES-A score was related to a higher level of education, having cancer, higher GC-specific self-efficacy, more social support, higher instrumental satisfaction with the GC session, and lower level of worry immediately after the GC. Having cancer showed a significant interaction with time and had the strongest effect 2 weeks before GC (T1) and 6 months after GC (T5). One year after GC, the effect of having cancer was no longer significant.
The following variables were not included in the final model for avoidance: age, gender, having children, cohabiting status, first-degree relative with cancer, physical function, satisfaction with GC (affective, procedural), and the result of genetic testing.
Testing the main effects in a stepwise forward procedure gave the same results as the stepwise backward procedure for both the IES-A and IES-I, and these effects are not reported here.
Discussion
The mean IES-I and IES-A scores at all assessments were within the moderate level according to Horowitz’s classification. One should note, however, that nearly one fourth of the subjects scored above the cut-off for severe intrusion while waiting for the GC session. Even though the mean score on the IES-I and IES-A were relatively low at baseline, they declined significantly from baseline and 1 year after GC, a trend that is consistent with earlier research [9]. The reduction in average IES-I score represents 10% of the scoring range and should be considered clinically significant, whereas the reduction in IES-A score was smaller. This tendency is also consistent with previous research findings [21], indicating that symptoms of intrusion may be activated more easily than are symptoms of avoidance and therefore have the possibility of a decline [41]. We cannot, however, exclude the possibility that the low level of avoidance is the result of a selection bias because an individual with a higher level of habitual avoidance would be less likely to seek out GC.
One important aspect in GC is identifying potential psychologically vulnerable patients to secure them adequate support during and after the GC session. The observation that nearly one fourth of the subjects had a severe level of intrusion was surprising. One previous study showed that a high level of intrusion occurs infrequently (almost 11%) among women without cancer undergoing counseling and testing for hereditary cancer [28]. These subjects had earlier attended GC and had just recently received a letter offering them genetic testing due to a discovered mutation in BRCA-1 in a family member [28]. Another study showed that women at risk for breast or colorectal cancer with no detected mutation in their family exhibit intrusion levels similar to our findings [13]. We might have expected that the knowledge of a mutated cancer gene in the family was more distressing than approaching a department of medical genetics for a GC session. The findings in the present study and a previous study [13] seem to indicate that the absence of a demonstrated mutation results in higher level of distress than among subjects with a knowledge of mutation in their family [28].
The observed reduction of the proportion of individuals with a score in the severe range of intrusion from before to 1 year after the GC may be related to several factors. The change indicates that the intrusion reactions have more of an anticipatory character and that the contact and information given in the GC session may have attenuated the negative implications for many participants. Helping people cope with the knowledge that cancer is part of their genetic inheritance is crucial in GC. This may include helping the individual to sort out various feelings and thoughts about the cancer risk, referring them to adequate surveillance programs, and explaining the nature of heredity. All of these aspects could contribute to the decreased level of intrusion with time. On the other hand, a substantial number of subjects were not included in the surveillance programs directly after GC, and this may also have had a reassuring effect, even though some of these subjects will be included as they age (see inclusion criteria to surveillance program in “The GC protocol”). We are cautious when drawing specific conclusions about the effect of GC because some of the participants were probably experiencing other important life events, which we could not adjust for. We also note that the results of the genetic test given shortly before T5 were unrelated to both intrusion and avoidance in the mixed models, even though both intrusion and avoidance increased at that time. The genetic test result may on the other hand not be such a good predictor in this sample since only six mutation carriers were detected. In an earlier publication of the same sample [6], we reported finding support for buffer effects of social support 6 months after GC, indicating that this time may be a challenge for people undergoing GC for hereditary cancer. The effect of the genetic test should be examined in larger samples.
The proportion of individuals with a severe level of avoidance was low at baseline and did not decrease significantly from before GC to 1 year after GC, which is consistent with pervious findings [29]. The most likely explanation is that this is a “floor-effect” because the average IES-A score was low at baseline and could not improve much from there. As mentioned, this may be an effect of selection bias.
Even though we found low mean IES scores for the total sample, a group of participants reported a severe level of intrusion and avoidance. These individuals should receive more individualized attention and information. It is important to identify those with a severe level of both IES-I and IES-A to provide this information and ensure adequate follow-up.
Some of the effects of socio-demographic, medical, and psychosocial variables on avoidance and intrusion were more prominent than others. First, lower baseline level of GC-specific self-efficacy predicted higher IES-I and IES-A scores. The GC-specific self-efficacy instrument measures the subject’s own beliefs about his or her ability to cope with the various tasks and demands related to the GC. In other words, how a person expects to be able to cope with the situation is important for the outcome in terms of intrusion and avoidance. GC-specific self-efficacy also interacted significantly with time and intrusion, indicating that the baseline GC-specific self-efficacy had the strongest effect on the long-term level of intrusion, i.e., 6 months and 1 year after GC. This suggests a possible causal effect of self-efficacy on intrusion. The GC-specific self-efficacy questionnaire seems to be sufficiently sensitive to identify those subjects more vulnerable to long-term intrusion and could therefore be useful as a screening tool. Future research should involve intervention studies based on improving the GC-specific self-efficacy of the counselees.
Second, the level of worry after GC was also related to both intrusion and avoidance. More worry after the GC could trigger further intrusion and avoidance. On the other hand, the highest levels of intrusion and avoidance were seen before the assessment of worry, indicating that worry may be the result of intrusion and avoidance, and these reactions could be two sides of the same issue. Regardless of the direction of the influence, this one-item scale may in the future serve as a suitable and time-saving screening tool to identify subjects who might need extra psychological follow-up. Before this single item scale may be used as a screening tool in a clinical setting, more rigorous testing is needed in order to fully validate this question against other measures of worry.
Third, the “cancer status” was also related to both a lower level of intrusion (cancer diagnosis of a first-degree relative) and of avoidance (the subject’s own cancer diagnosis). Surprisingly, the presence of one’s own cancer diagnosis was related to less avoidance. In other words, it seems like having a cancer diagnosis protected the subjects. However, previous studies are equivocal about the effects of a cancer diagnosis on distress. Codello et al. [10] found that distress, measured as anxiety, was significantly higher in disease-free subjects undergoing GC for hereditary breast and ovarian cancer compared to those with a cancer diagnosis. In contrast, others have found that women with cancer have a significantly higher level of intrusion and avoidance before genetic testing than those with no cancer diagnosis [29]. The mixed linear model for avoidance showed that “having cancer themselves” interacted significantly with time and that this effect was strongest at baseline (T1) and 6 months after GC (T5). In a previously published study examining anxiety and depression related to GC, we found that anxiety was also significantly higher at these two assessment times [6]. At baseline, the data were collected from the subjects at the same time that they received a letter scheduling their appointment with the department of medical genetics. Just before data collection, 6 months after GC, the subjects who had performed gene tests were receiving their results, and almost all subjects who were included in surveillance program had been to their first check-up. All these situations might contain stressful events and could have reminded the subjects of the diseases in their family and their own increased risk of developing cancer. In order to draw a firm conclusion, we need to scrutinize the psychological and social characteristics in the context for these assessment points.
Our findings that “a first-degree relative with cancer” was related to a lower level of intrusion was also in contrast with other studies showing that having a first-degree relative with cancer is associated with an increased level of distress [27, 31]. Intuitively, one might consider that having a first-degree relative with cancer is a burden that should increase the probability of intrusive thoughts and feelings. However, this may give the subjects an opportunity to work through the emotional aspects related to the risk of getting cancer, which should help prepare the individual to cope with the anticipated challenges connected to GC for hereditary cancer (at T1) and the feedback from the genetic testing. If so, this implies that those with an affected first-degree relative may have already accepted that cancer runs in their family, and this may have reduced the probability of experiencing the troublesome thoughts that characterize intrusion.
We found that a higher level of social support protected against avoidance. Perceived social support is considered a general resource in a subject’s life, and our finding shows that this general resource also plays an important role in how the person copes with specific life events such as cancer in the family. Our earlier studies suggested that social support may be a buffer against depression and anxiety related to GC [6].
Limitations and strengths of the study
The subjects seemed to be resourceful in the sense that they had high level of social support, had high GC-specific self-efficacy, had good physical functioning, were satisfied with the counseling session, and had a low level of worry after GC. We cannot rule out the possibility that the high level of self-referral in this sample introduced a selection bias toward a well-functioning sample.
Two of the subscales of the satisfaction with genetic counseling scale, procedural and instrumental satisfaction, had rather low alpha value. Cronbach’s alpha is sensitive to the number of items, and because these subscales only had three items each, this might explain the low reliability. Conclusions regarding the procedural and instrumental satisfaction must be drawn with caution since the two subscales had rather low reliability.
We collected the main dataset at four different times and must consider the statistical phenomenon of regression to the mean as a possible explanation of the decreases in IES-I and IES-A scores. On the other hand, one could argue that the multiple data collection and the longitudinally perspective are a strength of the study.
Conclusion
Most of the research within the field of GC has focused on subjects with monogenetic diseases present in their families, e.g., BRCA1/2 mutations [40]. As our understanding of molecular genetics continues to accelerate and includes polygenetic and multi-factorial influences on cancer, interpreting the results of genetic testing, and providing GC offers new and increasingly complex challenges [33, 40]. Thus, it is important to monitor changes in subjects undergoing GC to understand the process and to be prepared to offer the needed support.
We found a moderate mean level of intrusion and avoidance, although a significant number of participants had scores indicating a severe level of intrusion. Subjects undergoing GC for hereditary cancer with a low level of GC-specific self-efficacy at baseline and a high level of worry immediately after GC seem to be vulnerable to both intrusion and avoidance. These findings should be tested further using specialized interventions in randomized and controlled studies.
References
American Psychiatric Association (1997) Diagnostiske kriterier fra DSM-IV, 4th edn. Pilgrim Press, Oslo
Baider L, Ever-Hadani P, Kaplan De-Nour A (1999) Psychological distress in healthy women with familial breast cancer: like mother, like daughter? Int J Psychiatry Med 29:411–420
Bandura A (1997) Self-efficacy: the exercise of control. Freeman, New York
Berglund G, Liden A, Hansson MG, Oberg K, Sjoden PO, Nordin K (2003) Quality of life in patients with multiple endocrine neoplasia type 1 (MEN 1). Fam Cancer 2:27–33. doi:10.1023/A:1023252107120
Berkenstadt M, Shiloh S, Barkai G, Katznelson MB, Goldman B (1999) Perceived personal control (PPC): a new concept in measuring outcome of genetic counseling. Am J Med Genet 82:53–59. doi:10.1002/(SICI) 1096-8628(19990101) 82:1<53::AID-AJMG11>3.0.CO;2-#
Bjorvatn C, Eide GE, Hanestad BR, Havik OE (2008) Anxiety and depression among subjects attending genetic counseling for hereditary cancer. Patient Educ Couns 71:234–243. doi:10.1016/j.pec.2008.01.008
Bjorvatn C, Eide GE, Hanestad BR, Oyen N, Havik OE, Carlsson A, Berglund G (2007) Risk perception, worry and satisfaction related to genetic counseling for hereditary cancer. J Genet Couns 16:211–222. doi:10.1007/s10897-006-9061-4
Chung MC, Berger Z, Rudd H (2008) Coping with posttraumatic stress disorder and comorbidity after myocardial infarction. Compr Psychiatry 49:55–64. doi:10.1016/j.comppsych.2007.08.003
Claes E, Evers-Kiebooms G, Denayer L, Decruyenaere M, Boogaerts A, Philippe K, Legius E (2005) Predictive genetic testing for hereditary breast and ovarian cancer: psychological distress and illness representations 1 year following disclosure. J Genet Couns 14:349–363. doi:10.1007/s10897-005-1371-4
Condello C, Gesuita R, Pensabene M, Spagnoletti I, Capuano I, Baldi C, Carle F, Contegiacomo A (2007) Distress and family functioning in oncogenetic counselling for hereditary and familial breast and/or ovarian cancers. J Genet Couns 16:625–634. doi:10.1007/s10897-007-9102-7
Eide H, Graugaard P, Holgersen K, Finset A (2003) Physician communication in different phases of a consultation at an oncology outpatient clinic related to patient satisfaction. Patient Educ Couns 51:259–266. doi:10.1016/S0738-3991(02) 00225-2
Esplen MJ, Madlensky L, Aronson M, Rothenmund H, Gallinger S, Butler K, Toner B, Wong J, Manno M, McLaughlin J (2007) Colorectal cancer survivors undergoing genetic testing for hereditary non-polyposis colorectal cancer: motivational factors and psychosocial functioning. Clin Genet 72:394–401
Geirdal AO, Reichelt JG, Dahl AA, Heimdal K, Maehle L, Stormorken A, Moller P (2005) Psychological distress in women at risk of hereditary breast/ovarian or HNPCC cancers in the absence of demonstrated mutations. Fam Cancer 4:121–126. doi:10.1007/s10689-004-7995-y
Gueorguieva R, Krystal JH (2004) Move over ANOVA: progress in analyzing repeated-measures data and its reflection in papers published in the Archives of General Psychiatry. Arch Gen Psychiatry 61:310–317. doi:10.1001/archpsyc.61.3.310
Hall JA, Dornan MC (1990) Patient sociodemographic characteristics as predictors of satisfaction with medical care: a meta-analysis. Soc Sci Med 30:811–818. doi:10.1016/0277-9536(90) 90205-7
Horowitz M, Wilner N, Alvarez W (1979) Impact of Event Scale: a measure of subjective stress. Psychosom Med 41:209–218
Jackson JL, Chamberlin J, Kroenke K (2001) Predictors of patient satisfaction. Soc Sci Med 52:609–620. doi:10.1016/S0277-9536(00) 00164-7
Jadoulle V, Rokbani L, Ogez D, Maccioni J, Lories G, Bruchon-Schweitzer M, Constant A (2006) Coping and adapting to breast cancer: a six-month prospective study. Bull Cancer 93:E67–E72
Kasparian NA, Wakefield CE, Meiser B (2007) Assessment of psychosocial outcomes in genetic counseling research: an overview of available measurement scales. J Genet Couns 16:693–712. doi:10.1007/s10897-007-9111-6
King KB, Reis HT, Porter LA, Norsen LH (1993) Social support and long-term recovery from coronary artery surgery: effects on patients and spouses. Health Psychol 12:56–63. doi:10.1037/0278-6133.12.1.56
Koopman C, Butler LD, Classen C, Giese-Davis J, Morrow GR, Westendorf J, Banerjee T, Spiegel D (2002) Traumatic stress symptoms among women with recently diagnosed primary breast cancer. J Trauma Stress 15:277–287. doi:10.1023/A:1016295610660
Mehnert A, Koch U (2007) Prevalence of acute and post-traumatic stress disorder and comorbid mental disorders in breast cancer patients during primary cancer care: a prospective study. Psychooncology 16:181–188. doi:10.1002/pon.1057
Moller P, Evans G, Haites N, Vasen H, Reis MM, Anderson E, Apold J, Hodgson S, Eccles D, Olsson H, Stoppa-Lyonnet D, Chang-Claude J, Morrison PJ, Bevilacqua G, Heimdal K, Maehle L, Lalloo F, Gregory H, Preece P, Borg A, Nevin NC, Caligo M, Steel CM (1999) Guidelines for follow-up of women at high risk for inherited breast cancer: consensus statement from the Biomed 2 Demonstration Programme on Inherited Breast Cancer. Dis Markers 15:207–211
Neville K (1998) The relationships among uncertainty, social support, and psychological distress in adolescents recently diagnosed with cancer. J Pediatr Oncol Nurs 15:37–46
Nordin K, Liden A, Hansson M, Rosenquist R, Berglund G (2002) Coping style, psychological distress, risk perception, and satisfaction in subjects attending genetic counselling for hereditary cancer. J Med Genet 39:689–694. doi:10.1136/jmg.39.9.689
Pigott C, Pollard A, Thomson K, Aranda S (2008) Unmet needs in cancer patients: development of a supportive needs screening tool (SNST). Support Care Cancer 17:33–45
Rabin C, Rogers ML, Pinto BM, Nash JM, Frierson GM, Trask PC (2007) Effect of personal cancer history and family cancer history on levels of psychological distress. Soc Sci Med 64:411–416. doi:10.1016/j.socscimed.2006.09.004
Reichelt JG, Dahl AA, Heimdal K, Moller P (1999) Uptake of genetic testing and pre-test levels of mental distress in Norwegian families with known BRCA1 mutations. Dis Markers 15:139–143
Reichelt JG, Heimdal K, Moller P, Dahl AA (2004) BRCA1 testing with definitive results: a prospective study of psychological distress in a large clinic-based sample. Fam Cancer 3:21–28. doi:10.1023/B:FAME.0000026820.32469.4a
Ringdal GI, Ringdal K, Jordhoy MS, Kaasa S (2007) Does social support from family and friends work as a buffer against reactions to stressful life events such as terminal cancer? Palliat Support Care 5:61–69. doi:10.1017/S1478951507070083
Rini C, Jandorf L, Valdimarsdottir H, Brown K, Itzkowitz SH (2008) Distress among inflammatory bowel disease patients at high risk for colorectal cancer: a preliminary investigation of the effects of family history of cancer, disease duration, and perceived social support. Psychooncology 17:354–362. doi:10.1002/pon.1227
Rodriguez-Bigas MA, Boland CR, Hamilton SR, Henson DE, Jass JR, Khan PM, Lynch H, Perucho M, Smyrk T, Sobin L, Srivastava S (1997) A National Cancer Institute Workshop on Hereditary Nonpolyposis Colorectal Cancer Syndrome: meeting highlights and Bethesda guidelines. J Natl Cancer Inst 89:1758–1762
Sanderson SC, Michie S (2007) Genetic testing for heart disease susceptibility: potential impact on motivation to quit smoking. Clin Genet 71:501–510. doi:10.1111/j.1399-0004.2007.00810.x
Schlich-Bakker KJ, Warlam-Rodenhuis CC, van Echtelt J, van den Bout J, Ausems MG, ten Kroode HF (2006) Short term psychological distress in patients actively approached for genetic counselling after diagnosis of breast cancer. Eur J Cancer 42:2722–2728. doi:10.1016/j.ejca.2006.05.032
Sheldrick R, Tarrier N, Berry E, Kincey J (2006) Post-traumatic stress disorder and illness perceptions over time following myocardial infarction and subarachnoid haemorrhage. Br J Health Psychol 11:387–400. doi:10.1348/135910705X71434
Shiloh S, Avdor O, Goodman RM (1990) Satisfaction with genetic counseling: dimensions and measurement. Am J Med Genet 37:522–529. doi:10.1002/ajmg.1320370419
Sundin EC, Horowitz MJ (2002) Impact of Event Scale: psychometric properties. Br J Psychiatry 180:205–209. doi:10.1192/bjp. 180.3.205
Thewes B, Meiser B, Hickie IB (2001) Psychometric properties of the Impact of Event Scale amongst women at increased risk for hereditary breast cancer. Psychooncology 10:459–468. doi:10.1002/pon.533
Tjemsland L, Soreide JA, Malt UF (1998) Posttraumatic distress symptoms in operable breast cancer III: status one year after surgery. Breast Cancer Res Treat 47:141–151. doi:10.1023/A:1005957302990
Vadaparampil ST, Ropka M, Stefanek ME (2005) Measurement of psychological factors associated with genetic testing for hereditary breast, ovarian and colon cancers. Fam Cancer 4:195–206. doi:10.1007/s10689-004-1446-7
van der Kolk BA (2001) The psychobiology and psychopharmacology of PTSD. Hum Psychopharmacol Clin Exp 16:49–64. doi:10.1002/hup. 270
van Oostrom I, Meijers-Heijboer H, Duivenvoorden HJ, Brocker-Vriends AH, van Asperen CJ, Sijmons RH, Seynaeve C, Van Gool AR, Klijn JG, Tibben A (2007) The common sense model of self-regulation and psychological adjustment to predictive genetic testing: a prospective study. Psychooncology 16:1121–1129. doi:10.1002/pon.1178
Vasen HF, Mecklin JP, Khan PM, Lynch HT (1991) The International Collaborative Group on Hereditary Non-Polyposis Colorectal Cancer (ICG-HNPCC). Dis Colon Rectum 34:424–425. doi:10.1007/BF02053699
Vasen HF, Watson P, Mecklin JP, Lynch HT (1999) New clinical criteria for hereditary nonpolyposis colorectal cancer (HNPCC, Lynch syndrome) proposed by the International Collaborative group on HNPCC. Gastroenterology 116:1453–1456. doi:10.1016/S0016-5085(99) 70510-X
Ware JE, Kosinski M, Gandek B et al (2000) SF-36 health survey : manual & interpretation guide. QualityMetric, Lincoln, RI
Aalfs CM, Oort FJ, de Haes JC, Leschot NJ, Smets EM (2007) A comparison of counselee and counselor satisfaction in reproductive genetic counseling. Clin Genet 72:74–82. doi:10.1111/j.1399-0004.2007.00834.x
Acknowledgments
The authors are grateful for the assistance with data collection provided by the Centre of Medical Genetics and Molecular Medicine, Haukeland University Hospital, Bergen, Norway, and the Centre of Medical Genetics, St. Olav Hospital, Trondheim, Norway. We are also grateful to Professor Cathrine Himberg, California State University, for linguistic advice. This project was funded by the Norwegian Research Council, Functional Genome Project (FUGE) no. 155757/510.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bjorvatn, C., Eide, G.E., Hanestad, B.R. et al. Intrusion and avoidance in subjects undergoing genetic investigation and counseling for hereditary cancer. Support Care Cancer 17, 1371–1381 (2009). https://doi.org/10.1007/s00520-009-0594-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-009-0594-6