Abstract
Goal of work
The aim of this study was to assess the impact of an aging US population on inpatient costs and resource utilization in cancer patients admitted for infection.
Materials and methods
From the Texas inpatient public use files (Texas Health Care Information Collection), which include all hospitals except federal institutions, we selected residents with cancer who also had a principal or admitting diagnosis of pneumonia, bacteremia/sepsis, or other documented infection in 2001. Selected admission records were directly adjusted by projected age-specific cancer prevalence totals for years 2006 and 2025 using surveillance epidemiology end results (SEER) and US census data. Charges were inflated to 2006 consumer price index for medical care then converted to costs using Texas Medicare cost-to-charge ratios.
Results
Over 9% of nearly 200,000 Texans admitted for infection in 2001 also had cancer. Projecting these results nationally, 318,000 discharges in cancer patients at a cost of $3.1 billion (B, 95% CI $2.8B, $3.4B) and 2.3 million (M) bed days would have been attributed to infections in 2006. By the year 2025, adjusting only for the aging population, costs could increase 45% to $4.5B (95% CI $4.1B, $4.9), with 27% more (3.4 M) hospital bed days occupied.
Conclusions
Consequent to an aging population and the resulting increase in cancer prevalence, the healthcare burden of managing hospital admissions for infection in the vulnerable cancer population could be greatly magnified unless risk-based treatment and preventive strategies such as appropriate immunizations and infection control measures are implemented.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Many have speculated that the aging of the “baby boomer” generation will affect healthcare reimbursement systems and out-of-pocket health expenditures. These speculations are fueled by projections that by 2025, the US population will total nearly 360 million, with 64 million (18% of total) older than age 65, an increase of 73% in this age group [15]. Aging poses increased risks for a number of conditions, including cancer, and an increased susceptibility to infection. Thus, elders battling malignancy and its effect on their immune system are doubly disadvantaged with respect to infection risk [20]. Increasing survival among elders with cancer will result in corresponding increases in this cancer population at risk for an infection requiring hospital admission [14, 28]. It is quite likely that utilization of healthcare resources and healthcare costs will escalate as a result of managing infections among elders with cancer [7]. Microorganisms’ increasing resistance to existing therapies and a relative absence of new pharmaceuticals in the pipeline also will increase both the human and economic burdens of these infections [26].
The severity of infectious complications in cancer patients has long been known and explored [2]. Likewise, the challenges of preventing and treating infections in cancer patients have been well documented particularly among those undergoing chemotherapy who become neutropenic [3, 9–11, 25]. Costs associated with emergency and inpatient care of the neutropenic cancer patient have been estimated and infection in that group has been well documented [9]. Since not all infections in this population are serious and hospital admission for some is precautionary, the implementation of risk-based treatment in tandem with appropriate preventive and infection control measures could reduce infection-related hospitalizations [17]. Savings realized by this risk-based treatment approach has been reported for neutropenic patients and, if appropriately utilized, could likely yield similar savings for the senior cancer patient population [12]. The literature lacks information on the effect that the aging of the population will have on overall costs of inpatient admissions for infection in those with cancer. This is an important gap in the literature because these hospitalizations among the ever-increasing number of elders with cancer could overwhelm an already overtaxed government insurance program (Medicare) and overburdened healthcare system as well as compromise the financial health of retirees living on a fixed income.
In this study, we examine the effect of the aging population on cancer prevalence totals and then focus on one potential consequence of cancer, hospital admission principally for infection among this group in the USA. Our objectives were to: (1) estimate a baseline frequency of inpatient admissions for infection among those with cancer; (2) describe resource utilization and costs associated with those admissions; (3) examine the economic and resource impact of the aging US population on future hospital admissions for infection in patients with cancer; (4) provide global cancer prevalence estimates and projections; and (5) discuss infection prevention strategies for those with cancer.
Materials and methods
Data sources
Hospital admissions for infection among cancer patients were selected from the Texas inpatient public use file for 2001, which consists of information reported from every non-federal hospital and includes the number of days and the total amount charged for each hospital stay. This database is one component of the Texas Health Care Information Collection and is compiled and maintained by the Center for Health Statistics, Texas Department of State Health Services [29]. Hospital discharge records with a principal or admitting ICD-9-CM diagnosis of bacteremia, pneumonia, fever of unknown origin (FUO) or other documented infection (ODI) among Texas residents with any cancer were selected. The ICD-9-CM codes for infections and cancer are listed in Table 1. Age-specific future cancer prevalence was estimated for 2006 and 2025 using US Census Bureau population projection totals for the US and Texas (based on the 2000 US census) for those years [15] and limited duration 28-year cancer prevalence totals for 2003 from the US National Cancer Institute’s surveillance epidemiology and end results (SEER) program SEER*Stat 6.2 [28].
Global cancer prevalence and population estimates for developed and developing areas of the world were retrieved from the International Agency for Research on Cancer’s Globocan 2002 database and used to project cancer prevalence for the year 2025 [14].
Statistical analysis
To estimate the impact of the aging population on medical admissions for infection among cancer patients in the USA, we first established a baseline of age-specific frequencies and associated mean total charges and days stayed by 5-year age group from the identified medical admissions for infection among cancer patients in Texas. To reflect the perspective of the provider, reported charges were inflated to 2006 US dollars according to the consumer price index for medical care [8] and reported as a surrogate measure of cost [4] by converting charges using the 2006 Medicare cost-to-charge ratio for Texas [13]. Cancer prevalence totals from the most recently compiled national cancer data (SEER) at study time was directly adjusted by 5-year age groups to the 2006 and 2025 projected census populations for Texas and the USA.
To estimate numbers of inpatient admissions for infection among cancer patients in the USA, we directly adjusted the Texas baseline data to the projected cancer prevalence totals for the USA by 5-year age groups for the years 2006 and 2025. The baseline mean cost and length of stay data was then multiplied by the estimated number of age-specific US cancer patients with a medical admission for infection for each of the years, 2006 and 2025. Since many coexisting medical conditions contribute to infection risk, comorbidity was assessed using the Romano method of adapting the Charlson score to administrative data [24] and reported as a patient characteristic.
Similar to the method described above for the USA, we estimated global cancer prevalence for the group aged 65 and over for 2002 (the most recent year available at study time) and projected for 2025. All analyses were performed using SPSS 12.0 [27].
Results
In 2001, of the 18,012 hospitalizations for serious infections that occurred among Texas residents with cancer, more than half were for pneumonia (51%), while FUO and bacteremia/sepsis were responsible for 23% and 2% of the admissions, respectively. The remaining 24% included any other documented infection, of which 11% were wound infections (ICD-9-CM = 681.xx–682.xx). Using the 2001 estimated average cost per stay of $9,561 for elderly Texas patients estimated nationally for that year, the total bill for 172,246 senior infection-related hospitalizations would have been over $1.5 billion.
The distribution of cancer site and type of infection within each site is depicted in Fig. 1. Of the major cancer sites, infection-related admissions were predominately among those with hematologic malignancy (27%). The primary site of cancer in those with a solid tumor was lung or respiratory tract for 18%, breast for 10%, colon/rectum for 6%, and prostate for 6%. The group categorized as “other” included 32% of the admissions in patients with cancer and comprised solid tumors of the digestive system (34%), urinary tract (15%), and female genital sites (11%), while 9% were sarcomas of various sites.
The majority of pneumonia admissions (29%) were observed in lung/respiratory cancer patients, while hematologic patients were the primary group admitted for fever of FUO or bacteremia/sepsis with (42%) and (38%), respectively. Of the 2,011 wound infections, the majority occurred in breast and hematologic cancer patients with 23% and 20%.
Table 2 describes the distribution of patient characteristics of age and coexisting medical conditions along with resource utilization in terms of costs and length of stay for these Texas cancer patients. Pneumonia contributed to over half of the total costs for and total bed days utilized by these patients with 70% older than age 65 at admission. Collectively, nearly 60% of medical admissions for infection were among those older than 65.
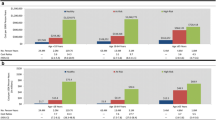
Derived from the Texas inpatient data and projected to the years 2006 and 2025, national estimates of hospitalizations for infections among cancer patients are illustrated in Fig. 2. Projecting the results nationally for 2006, 318,000 discharges in cancer patients at a cost of $3.1 billion (B) (95% CI $2.8B, $3.4B) and 2.3 million (M) bed days would have been attributed to serious infections. By the year 2025, adjusting only for the aging population, costs could increase 45% to $4.5B (95% CI $4.1B, $4.9B) with 27% more (3.4M) hospital bed days occupied. The most notable increases are in the 65 and older age groups. By the year 2025, medical admissions for infection-related conditions in people aged 65 and older adjusted only for population aging are projected to increase by 70% over 2006 totals and will exceed 300,000. Figure 3 depicts the projected and estimated resource utilization in bed days with corresponding costs for 2006 and 2025. Again, adjusted only for the aging of the population, the most notable increases in costs and resource utilization are observed in the group aged 65 to 84. For only those aged 65 and older, costs will nearly double, approaching expenditures of $3 billion. Measured in bed days, utilization will increase by 60% with over two million days used for these patients.
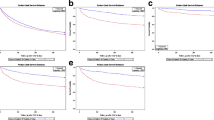
Globally, relative to the US aging population, Fig. 4 illustrates estimated cancer prevalence totals for those aged 65 and older for developing and developed areas of the world as reported by the IARC [14] for 2002 and projected to 2025. Trend lines indicate the proportion of elders in the total population for each of the 2 years by world location. The developing countries indicate a potential increase of 68% in the portion older than 65, compared to a 55% and 57% increase for the developed countries and the USA alone. The corresponding cancer prevalence in these elders is estimated to more than double in the developing countries, with percent increases of 49% and 77% in developed countries and the USA alone, respectively.
Discussion
We hypothesized that aging of the population could burden the healthcare and government reimbursement programs as a result of substantial increases in inpatient admissions due to infections among elders with cancer. To examine this issue, we projected annual costs of hospitalizations among elderly cancer patients for 2025, adjusting for the aging of the population. Our projected estimate of costs of hospitalization in this group for the year 2025 reflect the amount Medicare is projected to pay in 2025 based on the Medicare reimbursement rate in Texas in 2006, which would have equaled approximately $8,887 per person. Our method of limiting our study group to those admitted specifically for infection assumes that the total reported charges are related to the infection at admission.
While utilized as a fairly accurate measure of the direct cost of providing care [4], using the Medicare reimbursement model captures only part of the financial burden of inpatient care. This method of reporting costs does not account for patient deductibles and other non-covered expenses [21]. This model is also dependent on the Medicare reimbursement level set for each year. The importance of this is reflected in the decreased Medicare reimbursement rate in 2006 compared to that for 2001, which resulted in the appearance of a lower 2006 mean cost of $8,887 compared to $9,561 calculated for 2001 [13]. The significance of this finding to both health care providers and seniors is that this reduction does not represent a decrease in the cost of providing care, but rather a decrease in the amount that will be paid by Medicare and an increase in the amount that will have to be paid through other means or claimed as a loss by the health provider. The portion of the bill the patient is responsible for will place an additional strain on the nation’s elderly who live on a fixed income.
Furthermore, our estimates are computed using mean Texas costs, and when the 2006 Texas estimate of $8,887 per person is compared to $13,110 from cost estimates for 2005 reported by the Healthcare Cost and Utilization Project [30], our overall estimated $3 billion is low and would likely be in excess of $4 billion.
If national admissions for infection-related conditions among elderly cancer patients mirror those in Texas, most will be due to pneumonia for which the longest hospital stays and highest costs are observed both in this study and previously [7]. To reduce costs and resource utilization associated with pneumonia and other infection-related hospitalizations in cancer patients, we suggest a two-tier approach. First, adopt a standard policy of application of prevention measures. Secondly, if infection results in spite of such efforts, employ risk assessment procedures to identify those at lower risk for complication who could be treated with less expensive treatment modalities.
Preventive measures
A strategy combining measures from published reports is presented in Table 3. Incorporated are provisions whereby healthcare providers are guided to ensure that their patients with cancer have received appropriate immunizations, are screened for exposure to or early signs of infection during office visits, and are offered prophylaxis if warranted and/or prompt pre-emptive treatment [10, 19, 22]. Cancer patients, their family members, caregivers, and close contacts should be advised on signs and symptoms of common infections to be vigilant of and offered specific instructions on how to proceed if infections are detected. Close contacts should be educated about the cancer patient’s increased susceptibility to infection and measures they can take to decrease likelihood of infection, including receiving appropriate immunizations, avoiding contact when ill, or employing infection control precautions such as masks and gloves as appropriate [1, 5, 9, 25].
Risk-based care
Despite conscientious efforts, experience in cancer patients undergoing treatment reveals that some infections evade preventive efforts [23]. In such instances, risk assessment of potential complications based upon the Multinational Association for Supportive Care in Cancer (MASCC) risk index will allow individualized treatment regimens that could offer safe and cost-effective alternatives to conventional management of these infections [18]. Among the factors to consider when determining a treatment program are: the type of suspected infection, the type of cancer, and patient compliance. Even if neutropenic, many infections such as FUO, urinary tract infections (UTIs), and wound infections particularly in solid tumor patients may not require hospitalized care, but could be treated with oral antibiotics in an outpatient setting [12, 18, 22, 23]. Further, Cherif et al. [6] has demonstrated that neutropenic patients with hematologic cancer, who are assessed to be at low risk for complication, fare well and enjoy savings after early inpatient discharge resulting from oral versus intravenous antibiotic therapy. Elting et al. [12] concluded that outpatient versus inpatient treatment in those at lower risk of complications proved to be effective and fiscally advantageous. Avoiding hospitalization has other benefits to the patient, including evading potential nosocomial infection. Our current study reports that during a single year in Texas, 31% (5,584) of the admissions were in solid tumor patients with a less severe documented infection (UTI, wound infection, etc.) or FUO. Such patients would be prime candidates for risk-based care.
Although the savings potential is impressive, our results should be interpreted keeping the following limitations in mind. We used claims data for our study and there are inherent limitations in these data stemming from coding errors. Potentially, another diagnosis could be coded principally instead of infection, which would lead to an underestimate in the number of admissions for infections among cancer patients. The inverse is equally as likely and the effect of this bias on our estimates would be minimal, resulting in estimates that reliably reflect the numbers of admissions among cancer patients that are due to infection. Further, since coding rules are uniform, the results we report could be easily reproduced and the method of identifying cases employed in our study could be applied to other administrative databases and the same limitations would apply. Our intent was to identify those whose principal reason for being hospitalized was infection and group into type of infection. The low number of cancer patients in the bacteremia/sepsis group is likely due to the fact that it is typically diagnosed after admission, often following admission for pneumonia or another infection, and as such would be less apt to be coded as a principal or admitting diagnosis. As well, ours was a conservative estimation of costs, including only select infectious conditions more common among cancer patients. Costs associated with hospitalization for the year 2025 are extremely likely to be underestimated if medical costs continue to rise as sharply as they have in the past decade. Projected estimates are solely based on the effect the changing dynamic of aging will have on the prevalent cancer population at risk for being admitted for infection. As such, corresponding increases in comorbid conditions related to aging have not been accounted for in our cost and resource use estimates. As seen in Table 2, more than half of the Texas cancer patients admitted for the most common infection, pneumonia, had more than one comorbid condition when admitted. Should escalation of coexisting conditions play a role in increased susceptibility to infection, additional admissions could be realized, which would further contribute to an underestimate in our reported costs and resources.
As well, patterns of costs and bed days utilized reflect those observed in Texas in 2001. No adjustments were made for variation by geographic region or for variation in effectiveness of therapy provided. Should increases in antibiotic-resistant strains of bacteria and limited addition of effective pharmaceuticals be realized, our estimates would be considered conservative. Conversely, addition of more efficient or effective infection treatment could decrease length of stay and potentially render our reported estimates as overstated.
This study describes the impact of increases in inpatient admissions for infection in the cancer population in the USA that could be realized as our population ages. Clearly, the portion of elders worldwide is expected to increase, as those in even the developing countries are living longer. The staggering potential healthcare resources and expenditures due to the aging of the population estimated for the USA in this study could potentially be realized globally. This should be of particular concern to developing countries where healthcare resources are particularly scarce. In the USA, the economic burden could amount to $3–4 billion in costs charged to Medicare and an added resource load of millions of hospital bed days to healthcare facilities. Initiating preventive and risk-based measures will liberate scarce medical resources for use elsewhere.
References
American Cancer Society (2007) Infections in people with cancer: what are infections and who is at risk? Available at http://www.cancer.org/docroot/ETO/content/ETO_1_2X_Infections_in_People_with_Cancer.asp Accessed January 14, 2008
Bodey GP, Buckley M, Sathe YS, Freireich EJ (1966) Quantitative relationships between circulating leukocytes and infection in patients with acute leukemia. Ann Intern Med 64(2):328–340
Bodey GP (1985) Overview of the problem of infections in the immunocompromised host. Am J Med 79(5B):56–61
Brown ML, Riley GF, Schussler N, Etzioni R (2002) Estimating health care costs related to cancer treatment from SEER-Medicare data. Med Care 40(8 Supplement):IV–104–IV-117
Chehata S, Grira C, Legrand P, Pautas C, Maury S, Kuentz M, Carlet J, Cordonnier C (2006) Applying the concept of healthcare-associated infections to hematology programs. Haematologica 91:1414–1417
Cherif H, Johansson E, Bjorkholm M, Kalin M (2006) The feasibility of early hospital discharge with oral antimicrobial therapy in low risk patients with febrile neutropenia following chemotherapy for hematologic malignancies. Haematologica 91(2):215–222
Cooksley CD, Avritscher EB, Bekele BN, Rolston KV, Geraci JM, Elting LS (2005) Epidemiology and outcomes of serious influenza-related infections in the cancer population. Cancer 104(3):618–628 doi:10.1002/cncr.21203
Consumer Price Index for Medical Care. http://data.bls.gov/cgi-bin/surveymost accessed March 5, 2007
Courtney DM, Aldeen AZ, Gorman SM, Handler JA, Trifilio SM, Parada JP, Yarnold PR, Bennett CL (2007) Cancer-associated neutropenic fever: clinical outcome and economic costs of emergency department care. Oncologist 12:1019–1026 doi:10.1634/theoncologist.12-8-1019
Cullen M, Steven N, Billingham L, Gaunt B, Hastings M, Simmonds P, Stuart N, Rea D, Bower M, Fernan I, Huddart R, Gollins S, Stanley A (2005) Antibacterial prophylaxis after chemotherapy for solid tumors and lymphomas. N Engl J Med 353:988–998 doi:10.1056/NEJMoa050078
Elting LS, Rubenstein EB, Rolston KV, Bodey GP (1997) Outcomes of bacteremia in patient with cancer and neutropenia: observations from two decades of epidemiological and clinical trials. Clin Infect Dis 25:247–259 doi:10.1086/514550
Elting LS, Lu C, Escalante CP, Giordano SH, Trent JC, Cooksley C, Avritscher EB, Shih YC, Ensor J, Bekele BN, Gralla RJ, Talcott JA, Rolston K (2008) Outcomes and cost of outpatient or inpatient management of 712 patients with febrile neutropenia. J Clin Oncol 26:606–611 doi:10.1200/JCO.2007.13.8222
Federal Register/Vol. 70, No. 155/Friday, August 12, 2005/Rules and Regulations
Ferlay J, Parkin DM, Bray F, Pisani P (2005) Cancer incidence, mortality and prevalence worldwide. Globocan 2002, Version 1.0. Descriptive Epidemiology Group International Agency for Research on Cancer
Hollmann FW, Mulder TJ, Kallan JE (2000) Methodology and Assumptions for the Population Projections of the United States 1999 to 2100. Population Division Working Paper No. 38. Washington, DC. January 13, 2000. Available at http://www.census.gov/ipc/www/usinterimproj/ accessed March 1, 2007
Hogg W, Gray D (2007). The costs of preventing the spread of respiratory infection in family physician offices: a threshold analysis. BMC Health Services Research 7:181 article URL http://www.biomedcentral.com/1472-6963/7/181. Accessed 11/27/2007
Hughes WT, Armstrong D, Bodey GP, Bow EJ, Brown AE, Calandra T, Feld R, Pizzo PA, Rolston KVI, Shenep JL, Young LS (2002) 2002 guidelines for the use of antimicrobial agents in neutropenic patients with cancer. Clin Infect Dis 34:730–751 doi:10.1086/339215
Klastersky J, Paesmans M, Rubenstein EB, Boyer M, Elting L, Feld R, Gallagher J, Herrstedt J, Rapoport B, Rolston K, Talcott J (2000) The Multinational Association for Supportive Care in Cancer risk index: a multinational scoring system for identifying low-risk febrile neutropenic cancer patients. J Clin Oncol 18:3038–3051
Li, Zhongmin, and Mohanty P. Hospitalization in Texas, 2001. Austin (TX): Texas Health Care Information Council, February 2003. Revised March 7, 2003. THCIC Publication No. 87-11648
Morrison VA (2005) An overview of the management of infection and febrile neutropenia in patients with cancer. Support Cancer Ther 2:88–94 doi:10.3816/SCT.2005.n.002
Riley GF, Potosky AL, Lubitz JD, Kessler LG (1995) Medicare payments from diagnosis to death for elderly cancer patients by stage at diagnosis. Med Care 33(8):828–841 doi:10.1097/00005650-199508000-00007
Rolston KV, Manzullo EF, Elting LS, Frisbee-Hume SE, McMahon L, Theriault RL, Patel S, Benjamin RS (2006) Once daily, oral, outpatient quinolone monotherapy for low-risk cancer patients with fever and neutropenia: a pilot study of 40 patients based on validated risk-prediction rules. Cancer 106(11):2489–2494 doi:10.1002/cncr.21908
Rolston KV (2008) Risk assessment and the management of neutropenia and fever. In: Internal medical care of cancer patients. Hamilton, Ontario, Canada: BC Decker Inc.
Romano PS, Roos LL, Jollis JG (1993) Charlson comorbidity score adapted to administrative data. J Clin Epidemiol 46:1075–1079 doi:10.1016/0895-4356(93)90103-8
Sipsas NV, Bodey GP, Kontoyiannis DP (2005) Perspectives for the management of febrile neutropenic patients with cancer in the 21st century. Cancer 103:1103–1113 doi:10.1002/cncr.20890
Spellberg B, Guidos R, Gilbert D, Bradley J, Boucher HW, Scheld WM, Bartlett JG, Edwards J Jr (2008) Infectious Diseases Society of America. The epidemic of antibiotic-resistant infections: a call to action for the medical community from the Infectious Diseases Society of America. Clin Infect Dis 46(2):155–164 doi:10.1086/524891
SPSS for Windows Rel. 12.0.0. (2003). Chicago: SPSS Inc.
Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: Incidence—SEER 9 Regs Limited-Use, Nov 2006 Sub (1973–2004), National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics Branch, released April 2007, based on the November 2006 submission
Texas Hospital Inpatient Discharge Public Use Data File 2001. Texas Health Care Information Council, Austin, Texas
United States Department of health & Human Services Agency for Healthcare Research and Quality, Health Care Utilization Project HCUP Net http://hcupnet.ahrq.gov/ accessed 1/7/2008
Acknowledgments
This work was funded in part by the William Randolph Hearst Foundations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cooksley, C.D., Avritscher, E.B.C., Rolston, K.V. et al. Hospitalizations for infection in cancer patients: impact of an aging population. Support Care Cancer 17, 547–554 (2009). https://doi.org/10.1007/s00520-008-0520-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-008-0520-3