Abstract
Goals of work
This is a prospective and observational study comparing the efficacy of risk-assessment models in patients with neutropenic fever in a reference treatment center. The meaning of the complex infection was evaluated.
Materials and methods
Patients were recruited throughout a 9-month period. Inclusion criteria were histologic diagnosis of malignancy, neutropenic febrile secondary to chemotherapy and/or radiotherapy (absolute neutrophil count of <500/µl and axillary temperature ≥38°C), and ≥18 years of age.
Main results
Fifty-three febrile neutropenic patients were included. Twenty one of them were classified as low risk by the Multinational Association of Supportive Care in Cancer (MASCC) risk-index score. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy of the MASCC risk-index scores were, respectively 87.9, 85.0, 90.6, 80.9, and 86.8%. None of the low-risk patients died, but four patients classified as low risk by the MASCC model developed serious medical complications during febrile neutropenic episodes. When we subtracted patients with complex infections from the group of patients with the MASCC risk-index score of ≥21, we got 15 patients that were classified as low risk by a proposed adjustment by complex infection (PACI) model. None of them developed serious medical complications. The sensitivity, specificity, PPV, NPV, and the accuracy of this new model were, respectively, 100, 75.0, 86.8, 100, and 90.6%.
Conclusion
The MASCC risk-index score had high sensitivity and specificity to predict the absence of complications, but the PACI model was better than MASCC for predicting the absence of complications in this febrile neutropenic patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fever in cancer patients with chemotherapy-induced neutropenia remains a life-threatening complication despite progress in our understanding and in the treatment of this event[11]. Nowadays, the accepted standard of care for such patients has been routine hospitalization for prompt administration of empiric, broad-spectrum antibiotics, and close monitoring for development of complications until fever resolution and neutropenia recovery [6]. Although the conduction of the treatment in the hospital environment is efficient, not all febrile neutropenic patients require intensive treatment, and this practice has been debated [3].
Febrile neutropenic cancer patients constitute a heterogeneous population with different risk of developing a serious infection-related complication [4, 13, 14]. Although a universally accepted criterion does not exist, currently, the most used model of prediction of complications is the Multinational Association of Supportive Care in Cancer (MASCC) risk-index scores [8].
This study was designed to validate the MASCC risk-index scores in an attempt to accurately predict, on presentation with febrile neutropenia, which cancer patients are at low or high risk of development of serious medical complications during the episode and to determine the importance of subtracting patients with complex infections from the group of patients with a MASCC risk-index score of ≥21.
Materials and methods
Study design
This single-center prospective and observational study was performed at the Departments of Medical Oncology and Internal Hematology of the Felicio Rocho Hospital, Minas Gerais, Brazil, from March 1, 2004 to December 30, 2004.
Patient selection
All consecutive febrile episodes occurring in patients meeting the following eligibility criteria were included: histologic diagnosis of malignancy, neutropenic febrile secondary to chemotherapy and/or radiotherapy [neutropenia was defined as absolute neutrophil count (ANC) < 500/µl, including polymorphonuclear leukocytes and band forms or ANC < 1,000/µl expected to fall below 500/µl within 24 h], fever (axillary temperature ≥38°C documented by the patient or the medical/nursing staff), and age ≥18 years.
This study was conducted in accordance with Good Clinical Practice and the Declaration of Helsinki and was approved by the local ethics committee, and all patients gave written informed consent for participation. It was possible to enroll patients several times.
Treatment and risk assessment
All patients underwent a detailed history taking and complete physical examination and were assessed by the MASCC score in the first 24 h of study admission. Patients with a score ≥21 were considered to be at low risk. In this group, we subtracted patients with complex infection and constructed a new model (Fig. 1). All included patients were followed daily by a study investigator until discharge from hospital, and those individuals that left the hospital and received oral antimicrobials were contacted by the same investigator at the end of the treatment by phone. The best predictive model does not initially classify a patient who will develop serious medical complications (as defined above) during the treatment of febrile neutropenic episode as low risk. The presence or absence of complex infection was assessed at presentation, and this analysis was prospectively planned.
Algorithm used to classify the febrile neutropenic episodes by PACI model. MASCC risk-index: burden of illness indicating absence of or mild symptoms (5 points), or indicating moderate symptoms (3 points, not cumulative); absence of hypotension (5 points); absence of chronic obstructive pulmonary disease (4 points); solid tumor or hematologic tumor with no previous fungal infections (4 points); outpatient status (3 points); absence of dehydration (3 points); age less than 60 years (2 points). The maximum value of the score is 26. MASCC Multinational Association for Supportive Care in Cancer; PACI model Proposed Adjustment by Complex Infection model
All patients received intravenous broad-spectrum antibiotics, including an antipseudomonal beta-lactam in combination with an aminoglycoside or monotherapy with a third-generation cephalosporin. Other antibiotics were administrated according to the guidelines of the Infectious Diseases Society of America (IDSA) [6]. Antibiotics were maintained until the ANC recovered to over 500/µl and the patient had remained afebrile for 48 consecutive hours and for a minimum of 5 days.
Defining complex infection
Complex infections were predefined as follows: infection of major organs (lungs, liver, kidneys, colon, bone, joints, veins, heart, and meninges), sepsis, soft-tissue wound infection (>5 cm in size if without necrosis; any size if with necrosis), or oral mucositis grade >2.
Oral mucositis was evaluated by the World Health Organization Index as follows: grade 0, no change; grade 1, soreness and erythema; grade 2, erythema, ulcers, and can eat solids; grade 3, ulcers and requires liquid diet only; and grade 4, alimentation is not possible.
Defining serious medical complications
Serious medical complications were considered if the patient developed at least one of the following predefined categories: (1) antibiotic treatment change secondary to recurrence or persistent fever (unexplained fever higher than 38°C for ≥5 days, or fever higher than 39°C persisting after 72 h of antibiotic therapy), development of a new clinical localization of infection, clinical deterioration, serious adverse effects related to antibiotics, or bacterial sensitivity profile; (2) clinical deterioration secondary to febrile neutropenic episode predefined as following: presence of arterial hypotension (systolic blood pressure <90 mmHg or need for medicine support to maintain blood pressure); respiratory failure (respiratory rate >24 breaths/min, arterial oxygen pressure less than 60 mmHg while breathing room air, or need for supplemental oxygen); confusion or altered mental status leading to diagnostic work-up; renal failure (requiring investigation and/or treatment with parenteral fluids, dialysis, or any other intervention); severe gastrointestinal disorders; or sepsis; (3) hospital readmission related to neutropenic episode; (4) dehydration requiring prolonged parenteral fluids replacement (>3 days); (5) hemorrhage resulting in blood transfusion; (6) platelet count <20,000/μl; (7) abnormal serum ions requiring urgent therapy; (8) persistence of positive blood cultures or breakthrough bacteremia; (9) intensive-care unit admission; (10) death; and (11) other abnormalities judged serious and clinically significant by the investigator (Table 1).
Dehydration was defined as volume depletion (blood urea/creatinine >20, serum sodium ≥146 μmol/l, or documentation of impaired oral intake by an investigator associated with a complaint of thirst and dry oral mucous membrane that improved after replacement of 500 ml of normal saline over 1 to 3 h).
Statistical considerations
For the analysis of the primary objective of the study, a comparative evaluation of the MASCC risk-index scores and the proposed adjustment by complex infection (PACI) model was carried out through an accuracy study, evaluating the positive and negative predictive values, sensitivity, and specificity. The Kappa’s index was used to assess majority agreement between the models and Landis and Koch’s criterion to interpret this index. In the quality analysis of the tests used to predict complications in febrile neutropenic patients, the covariate “serious medical complications” was used to compare the models.
Secondary end points were duration of fever, neutropenia, intravenous antibiotic therapy, and hospitalization.
Because allowing patients to be enrolled several times during successive febrile episodes could induce a covariance structure among outcome data and invalidate statistical comparisons, only the first febrile episode occurring in a patient during the study period was considered.
Results
Overall patient characteristics
Sixty episodes of neutropenia and fever were seen at our institution during the study period, which occurred in 53 patients and constituted the basis of this report. Patient characteristics were summarized in Table 2. The majority was women (62.3%) and had hematologic cancer (64.2%). The median time to defervescence was 2 days (range, 1–19 days), and the median duration of neutropenia was 4 days (range, 1–40 days). Twenty-three patients (43.4%) had their antibiotic regimen modified. The median in-patient stay was 7 days (range, 2–88 days), and only four patients had permanent subcutaneous venous access devices. Granulocyte colony-stimulating factor was administered in 34 patients. There were nine deaths, but only seven were related to neutropenic fever.
The type of infection noticed at time of study admission is shown in Table 3.
Fourteen patients had microbiological infection, and a gram-negative pathogen was the main etiologic agent. The antibiotics were changed due to the bacterial sensitivity profile in only three cases, and no new emergent infectious agents were observed.
Twenty-nine febrile neutropenic patients (54.7%) were classified as carrying complex infection. The median in-patient stay of these patients was 10 days, and they required a median of 14 days of antibiotics. Twenty-six of them had a poor Eastern Cooperative Oncology Group (ECOG) performance status (≥grade 2), and 17 patients were admitted to intensive-care units.
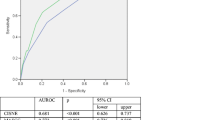
Comparative evaluation of the quality of the MASCC risk-index score and the PACI model
Table 4 shows the febrile neutropenic patients stratified by the MASCC risk-index score and by the PACI model. The sensitivity, specificity, predictive value, accuracy, and Kappa index of both models are reported.
Four patients classified as low risk by the MASCC score developed serious medical complications during febrile neutropenic episodes (“false” low risk). Three failures were due to respiratory distress (complication of bacterial pneumonia), and one patient developed dehydration requiring prolonged parenteral fluids (secondary oral mucositis >grade 2). The majority of serious medical complication started in the first 72 h of admission, and no deaths happened in this low-risk score. But the PACI model low-risk patients had no serious medical complications.
Discussion
The present study allows us to conclude that the exclusion of the patients with complex infection from the low-risk patients by the MASCC risk-index score determines significant improvement of the quality of this model in this population of febrile neutropenics. This modification determines sensitivity of 100% in the diagnosis of patients of low risk for complications, beyond keeping high levels of specificity, with a negative predictive value of 100%.
The MASCC risk-index score was the largest international collaborative study developed to allow a more precise and uniform selection of low-risk patient with neutropenic fever for predict the absence of complications [8]. This MASCC risk-index was validated prospectively in a small recent study. Low-risk neutropenic patients were identified with an accuracy of 98.3%, and there were no deaths reported in this group of patients [15].
Although the MASCC score addresses risk prediction instead of eligibility for an oral treatment or outpatient management, this risk assessment model has been used to identify low-risk patients for outpatient management with oral antibiotics [1, 12]. However, IDSA’ guideline doesn’t recommend routine outpatient treatment for low-risk febrile neutropenic patients [6]. Moreover, the MASCC risk-index score needs to be improved, in addition to being reproduced in other services, before it can be used in the practical clinic [7, 8, 10].
Escalante et al. [5] observed a high complication rate in low-risk febrile neutropenic patients (by MASCC risk-index score) with oral mucositis >grade 2 as they have poor capacity to ingest fluids and consequently have a higher possibility to develop complications like dehydration.
Another recent publication strengthens the necessity of improvement in the MASCC model. These authors observed that 15% of the patients classified as low risk developed serious complications and that 36% of these were not eligible for oral antibiotics [2].
The covariate evidence of infectious site was evaluated during the MASCC trial, but this did not present statistical significance in predicting complication. Nevertheless, as this clinical aspect was evaluated as presence or absence, different complexities of infection were analyzed in the same group, and consequently, it may have resulted in bias.
One recent trial evaluated the feasibility of withholding antibiotics and early hospital discharge in febrile neutropenic patients with low risk of bacterial infection. A risk-assessment model constructed on physical examination and IL-8 level was applied. Patients with signs of local bacterial infection, abnormal vital signs suggesting sepsis, or high IL-8 plasma levels were classified as high risk. Our study and this trial give support to active search for the source of infection in febrile neutropenic episodes to allocate risk groups [9].
The main limitations of our study were the small size of the sample. The unicentric aspect was another important limitation as this patient population had a very severe prognosis, and the overall rate of complications was very high.
Oral mucositis was evaluated by the World Health Organization Index, which gives a simple, overall rating of stomatitis, but limitations of this tool include the lack of reliability and validity data and the inability to capture the variety of oral changes that occur with cancer treatment.
In summary, this study allows us to conclude that the MASCC risk-index score had high sensitivity and specificity to predict the absence of serious medical complication, but the PACI model was better than MASCC model in this population of febrile neutropenic. The lack of validation jeopardizes the use of the PACI model in clinical practice, and this study does not have power to routinely recommend excluding patients with complex infections from the group of patients with a MASCC risk-index score of ≥21. However, this is a simple and easy adjustment that could determine better security, and it could keep the low rate of complications for further outpatient treatment study of low-risk neutropenic fever episodes in cancer patients.
References
Chamilos G, Bamias A, Efstathiou E et al (2005) Outpatient treatment of low-risk neutropenic fever in cancer patients using oral moxifloxacin. Cancer 103(12):2629–2635
Cherif H, Johansson E, Bjorkholm M et al (2006) The feasibility of early hospital discharge with oral antimicrobial therapy in low risk patients with febrile neutropenia following chemotherapy for hematologic malignancies. Haematologica 91(2):215–222
Donowitz GR, Maki DG, Crnich CJ, et al (2001) Infections in the Neutropenic Patient - New Views of an Old Problem. In: ANNUAL MEETING OF THE AMERICAN SOCIETY OF HEMATOLOGY, 43TH., 2001, Orlando. Education Program Book: Hematology (Am Soc Hematol Educ Program):113–139
Elting LS, Rubenstein EB, Rolston KV et al (1997) Outcomes of bacteremia in patients with cancer and neutropenia: Observations from two decades of epidemiological and clinical trials. Clin Infect Dis 25(2):247–259
Escalante CP, Weiser MA, Manzullo E et al (2004) Outcomes of treatment pathways in outpatient treatment of low risk febrile neutropenic cancer patients. Support Care Cancer 12(9):657–662
Hughes WT, Armstrong D, Bodey GP et al (2002) 2002 guidelines for the use of antimicrobial agents in neutropenic patients with cancer. Clin Infect Dis 34(6):730–751
Kern WV (2006) Risk assessment and treatment for low-risk patients with febrile neutropenia. Clin Infect Dis 42(4):533–540
Klastersky J, Paesmans M, Rubenstein EB et al (2000) The Multinational Association for Supportive Care in Cancer risk index: A multinational scoring system for identifying low-risk febrile neutropenic cancer patients. J Clin Oncol 18(16):3038–3051
Nijhuis CO, Kamps WA, Daenen SM et al (2005) Feasibility of withholding antibiotics in selected febrile neutropenic cancer patients. J Clin Oncol 23(30):7437–7444
Paesmans M (2000) Risk factors assessment in febrile neutropenia. Int J Antimicrob Agents 16(2):107–111
Sipsas NV, Bodey GP, Kontoyiannis DP (2005) Perspectives for the management of febrile neutropenic patients with cancer in the 21st century. Cancer 103(6):1103–1113
Rolston KV (2003) Oral antibiotic administration and early hospital discharge is a safe and effective alternative for treatment of low-risk neutropenic fever. Cancer Treat Rev 29(6):551–554
Rolston KV (1999) New trends in patient management: Risk-based therapy for febrile patients with neutropenia. Clin Infect Dis 29(3):515–521
Talcott JA, Finberg R, Mayer RJ et al (1988) The medical course of cancer patients with fever and neutropenia. Clinical identification of a low-risk subgroup at presentation. Arch Intern Med 148(12):2561–2568
Uys A, Rapoport BL, Anderson R (2004) Febrile neutropenia: a prospective study to validate the Multinational Association of Supportive Care of Cancer (MASCC) risk-index score. Support Care Cancer 12(8):555–560
Acknowledgement
We are indebted to all members of the Departments of Medical Oncology and Internal Hematology of the Felicio Rocho Hospital.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Souza Viana, L., Serufo, J.C., da Costa Rocha, M.O. et al. Performance of a modified MASCC index score for identifying low-risk febrile neutropenic cancer patients. Support Care Cancer 16, 841–846 (2008). https://doi.org/10.1007/s00520-007-0347-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-007-0347-3