Abstract
Goals of work
In gynecological oncology, there is growing interest in the use of complementary and alternative medicine (CAM) methods. The lack of data regarding side effects, the lack of any survival advantages, and the costs of these methods appear to have no influence on patients’ decisions on whether to use CAM. Our interest was to evaluate the association between CAM use and the patients’ quality of life/life satisfaction (QoL/LS).
Materials and methods
One thousand thirty women with breast cancer of gynecologic malignancies were asked to participate in this study, which included a questionnaire and a personal interview on CAM. User status was compared with the patient’s own description of her QoL/LS and with the cancer type.
Main results
CAM was used by 48.7% of all women (n = 502). Breast cancer patients stated that they used CAM in 50.1% and women with gynecological cancer in 44.0%. The use of mistletoe was widespread (77.3%) and was more often seen in breast cancer patients than in gynecological cancer patients (74.4% vs 67.0%). CAM users less frequently stated an overall deterioration of their health status (35.1%) compared to nonusers (50.1%). CAM use resulted in a stated improvement in family conditions (6%) in comparison with the nonusers (2%).
Conclusions
With regard to patients’ perception of health status, CAM use is associated with a better coping with their disease. Most other categories of LS are not affected by CAM use. Patient-oriented information comparing standard therapies with CAM methods should be made widely available, and patients’ expectations of CAM use should be discussed between the physician and the patient.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Outside the treatment guidelines and recommendations of conventional medicine, there are many approaches to most of the diseases from which mankind suffers. These treatments are summed up in the term “complementary and alternative medicine” (CAM). In the most recent representative survey of 31,044 adults conducted by the Centers for Disease Control in the USA, 36% reported current use of CAM. When megavitamins and prayer are included, the rate rises to 62% [2]. The use of CAM is common in patients with diseases, which set the patient at risk to experience a relapse or to suffer from sequelae of this disease or even to die. The percentage of users ranges from 10 to 98% [9, 10, 12, 19, 27]. In breast cancer patients, there have been studies reporting the range of use as 30–98% [5, 10, 22]. This large range can be explained by several circumstances. Several studies have shown that CAM users, for example, have a higher economic status, a higher educational status, and are younger and better informed about their disease [1, 5, 8, 13, 22]. As these and more confounders are known, this could effect on the reported user rate dependent on the population, which was investigated. In addition, the definition of CAM has changed in recent decades. The list of methods regarded as belonging to CAM is continually changing, as treatments that are proved to be safe and effective become adopted into conventional health care and as new approaches to health care emerge. This can result in different methods of questioning and, thus, lead to different user rates.
In the distinction made by the National Center for Complementary and Alternative Medicine, “complementary medicine” refers more to therapies that are used together with conventional medicine, while “alternative methods” are intended to be used instead of conventional therapies. However, this distinction depends on the local culture and the patient’s characteristics. Acupuncture, for example, is not regarded as a form of CAM in China. The range of use thus depends on the definition of CAM used and on the group of patients studied. Despite their common use, many CAM products and procedures have not been tested to determine their safety and efficacy. Even less is known about interactions of CAM interventions with chemotherapy and radiotherapy. Potential harm has been discussed [8, 11, 28].
In 1997, Americans spent an estimated $36–47 billion on CAM therapies [12]. In Germany (with 80 million inhabitants), the estimated expenditure amounted to €6.8 billion [21]. These are the costs of the drugs. Personnel costs and treatments such as acupuncture, massage, and other forms of therapy are not included in these calculations.
Another aspect also needs to be taken into consideration when evaluating the pros and cons of CAM therapy—namely, the patient’s quality of life (QoL) and life satisfaction (LS). Particularly in patients with lifetime-limiting and life-threatening diseases, QoL and LS are at least secondary objectives in almost all clinical trials. Less is known about this topic, as most studies are concerned with issues of efficacy, characterization of CAM users, and cost-effectiveness. Assessment of the QoL and LS is essential in the management and treatment of cancer patients. Particularly in patients with advanced disease, decisions about the treatment are often made first and foremost in relation to the patient’s QoL [16, 20]. Gynecological and breast malignancies, with 73,800 newly diagnosed cases per year, represent 37.9% of all cancers in women in Germany [3].
Approximately 17,600 women die every year due to breast cancer alone [3]. To investigate this group of patients particularly in relation to QoL and LS, we carried out a national multicenter study in order, firstly, to assess the patient reported changes in satisfaction during the course of the disease in relation to CAM use; secondly, to estimate differences in CAM use in patients with different types of cancer; and thirdly, to characterize CAM users in relation to their socioeconomic attributes.
In addition, the patients were asked about their reasons for either using or not using CAM, as well as the amount they were spending on CAM use and who was paying for it.
Materials and methods
Participants
The group of patients consisted of 1,030 women with gynecological or breast malignancies. The patients were recruited from different gynecology and obstetrics departments specializing in gynecological oncology in the area of Duesseldorf, Germany. They were randomly chosen and interviewed after providing verbal informed consent. Included in this study were only those patients who were considered to be aware of their disease, mentally able to understand the questions, and capable of the German language. Patients with breast cancer, endometrial cancer, cervical cancer, and ovarian cancer were included, regardless of the stage of their disease.
Assessment of QoL
To evaluate satisfaction, a questionnaire was drafted that precisely documented patient history, social, financial, and partnership aspects. This questionnaire on socioeconomic satisfaction as a part of QoL (SES-QoL) was filled in by the patient herself, with an interview afterwards so that any open questions could be completed. The SES-QoL consisted of two parts.
Part 1 included questions about the partnership situation, number of live births, age at menarche and menopause, religion, highest educational degree, highest degree of occupational education, occupation itself, family history of cancer, participation in cancer screening programs, participation in cancer follow-up programs, and further medical history, as well as nicotine or alcohol consumption.
Part 2 contained specific questions about satisfaction with the social, financial, and partnership situation, in a self-description by the patient. This part documented satisfaction with regard to occupation, accommodation, financial situation, partnership situation, familial support, recreational options, friendship situation, and sexual life. Statements about satisfaction in each category were also to be described for the time before the diagnosis of cancer and for the time of the interview after the diagnosis of cancer. After a temporary questionnaire had been designed, 50 patients were asked to complete the SES-QoL and to take part in an evaluation of whether the questions were able to mirror their satisfaction about topics related to their malignant disease. After this first evaluation, the SES-QoL was adjusted to the patients’ suggestions.
The SES-QoL is described in detail elsewhere [14].
A CAM module including 20 questions was also included in this survey. Detailed information was collected about existing experience with CAM use and motivation for CAM use. In addition, the patients were asked to name all types of CAM used and the period of time of use. Finally, the patients noted the amount they were spending each month on CAM. Table 1 lists the categories of named CAM therapies.
The interviews (n = 1,030) were completed between January 2000 and February 2002 and were conducted by medical personnel who had received training in interviewing techniques. The evaluation of the correct completion of the SES-QoL and the CAM module was reviewed by two persons (P. A. F. and K. N. M.).
Outcome measures and statistical methods
Satisfaction with regard to nine topics—health, leisure activities, sexual life, work, financial situation, partnership situation, family situation, housing situation, and friendship situation—was evaluated with regard to stated changes during the period of the disease. Changes were treated as events in terms of the analysis. Changes from “satisfied” to “not satisfied” were designated as deterioration and the opposite as improvement. Changes after the diagnosis of cancer were compared with statements about the time before the diagnosis and compared with the CAM status using contingency tables. To estimate the adjusted odds ratios (ORs), a logistic regression model was constructed, with CAM use as the dependent variable. Predictor variables included age, marital status (ever married/not married), disease stage status (disease-free/local recurrence and/or metastases), school qualifications as single covariates, occupational qualifications as single covariates, number of children, menopausal status, religion (active/not active), with medical certificate at the moment (yes/no), active participation in cancer surveillance programs, smoking status (smoker/nonsmoker), alcohol abuse (yes/no), end of partnership (yes/no), strengthened partnership (yes/no), and type of cancer (breast cancer, gynecologic cancer).
A stepwise, forward selection process was used to construct the model with variables, with significance set at P < 0.05. The Statistical Package for the Social Sciences program, version 12.0.1, was used (SPSS, Chicago, IL, USA).
Results
Study group
A total of 1,030 patients agreed to take part in the survey, 785 as hospital in-patients and 245 as outpatients. Table 2 shows the demographic and clinical characteristics of the patients. The most common disease was breast cancer (n = 796, 77.3%), followed by cervical cancer (n = 97, 9.4%), ovarian cancer (n = 97, 9.4%), and endometrial cancer (n = 40, 3.9%). Most of the patients had early-stage (not palliative) disease (n = 780, 76%). Metastatic disease was found in 250 patients (24%). On average, patients had 1.5 children, and 737 individuals (71.6%) had a partner. The median age was 53.6 years (range 20–92 years). The median interval between the interview and the time of diagnosis was 2.1 years (range 0.5–8.2 years). Patients from different social origins and professional groups were recruited. Most of the patients had either received a vocational education or had an academic degree (84.2%); 42.5% of the patients were in active jobs at the time of the interview. Table 2 summarizes the characteristics of the patients.
Is the use of CAM dependent on the type of cancer?
The two large tumor entities (breast cancer and gynecologic cancer) were compared in relation to CAM use. A total of 399 of the 796 breast cancer patients were CAM users (50.1%). Women with gynecologic cancer used CAM less often; 103 of 234 patients with either endometrial, cervical, or ovarian cancer used alternative or complementary methods as a treatment for their disease (44.0%). The chi-square test did not reveal any significant differences between the two groups (chi-square test 2.701; P = 0.058), although there was a trend suggesting a higher rate of use in the breast cancer group. The prevalence of CAM use for each type of cancer is shown in Table 3.
Is the use of a specific type of CAM dependent on the type of cancer?
The use of the different categories of CAM ranged from 19.1% for psychological therapy to 77.3% for the use of dietary supplements. In the two groups (breast cancer and gynecological cancer), dietary supplements were used most often (76.7% vs 79.6%). Statistically, the difference was not significant (P = 0.193). The second most used CAM in both groups was subcutaneous mistletoe therapy (74.4% vs 67%). The difference between the two groups was significant for mistletoe therapy (P = 0.028). All other CAM categories showed no significant differences (Table 4).
Does the use of CAM improve QoL/LS?
Changes in LS were measured by changes in statements regarding satisfaction in the categories: health status, leisure activities, working life, sexual life, financial situation, housing conditions, family conditions, and partnership situation. Regardless of the user status of CAM, almost all categories noted an overall deterioration (Fig. 1). A summation of the changes, with deterioration being recorded as −1, a situation of no change as 0, and improvement as +1, showed deteriorations in the categories of health status, leisure activities, working life, sexual life, and financial situation. Overall improvements were seen in relation to housing conditions, family conditions, and the partnership situation (Fig. 1).
Finally, with regard to the association of CAM use on the perception of LS, significant differences were only seen in two categories. The question of satisfaction with regard to health status showed an overall deterioration of 50.6% (52% deterioration vs 1.4% improvement) in the group of nonusers of CAM. With an overall deterioration of 35.1% (44.9% deterioration vs 9.8% improvement), patients who used CAM performed better (P < 0.001). The other category showing significant differences between the two groups was the family condition. In this study, as well, CAM users had better results (P = 0.024). While nonusers reported an overall improvement of 2% (0.7% deterioration vs 2.7% improvement), CAM users had an overall improvement of 6% (2.4% deterioration vs 8.4% improvement).
No significant differences were seen in the categories of leisure activities, sexual life, working life, housing conditions, financial situation, or partnership situation. CAM use appears to have no influence on the perception of LS in relation to these topics.
In the multivariate model, several markers were associated with CAM use. The adjusted OR for “end of partnership during disease” was 4.937 (95% confidence interval [95%CI], 1.085 to 22.463). Patients who stated a strengthened partnership had an OR of 0.611 (95%CI, 0.377 to 0.990), and patients with an unchanged partnership had an OR of 0.521 (95%CI, 0.345 to 0.788). Active participation in follow-up screening programs resulted in an OR of 3.127 (95%CI, 1.612 to 6.067). Other significant covariates are shown in Table 5.
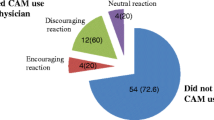
CAM users were asked who recommended CAM use to them. The recommendation came from the patient’s physician in 39.6% of cases; 3% were encouraged by their health insurance company regarding CAM use; and 49.3% stated that friends and family members had recommended CAM. Patients who did not use CAM had been dissuaded in 5% of cases by their physician and in 0.4% of cases by friends or family members.
Finally, the financial and health insurance aspects of CAM use were calculated. A total of 51.1% of patients reported that the full costs of CAM were refunded by their health insurance, while 23.4% were partly refunded. Only 13.3% financed their CAM use completely on their own. No support from health insurers had been sought by 7.7% of the patients, and 4.6% of the patients did not respond to this question. The costs amounted to 25/month in 20.4% of cases, to 50/month in 27.9%, 150/month in 26.1%, to 250/month in 5.1%, and 500/month or more in 5.2%. No response to this question was received from 15.2% of CAM users.
Discussion
This study documenting the use of CAM in a large group of patients with gynecological or breast malignancies analyzed patients’ self-stated degree of satisfaction with various aspects of their QoL/LS. Special attention was given to patients’ statements regarding changes in LS during the course of the disease in connection with the use of CAM. As treatment decisions for patients are based in part on QoL considerations, the association of CAM use with the patients’ statements is an important decision criterion.
The prevalence of CAM use in this study was in the usual range reported in previously published data [2, 9, 10, 12, 19, 27]. The sample size was sufficient to estimate differences in the prevalence of overall CAM use in the cohorts of cancer types. No significant differences with regard to overall use were seen. However, mistletoe was used significantly more often in patients with breast cancer. The reasons for this may lie in marketing strategies that take advantage of dissatisfaction with conventional Western medicine [2]. Commercial providers of these drugs may regard the larger market of breast cancer patients as being more promising than the market of gynecological cancer patients. Studies proving that the agents concerned have an anticancer effect are pending in both cases. Furthermore, active coping behavior was reported to be associated with CAM use with an OR of 1.65 [23]. Breast cancer patients in Germany are much better organized with regard to advocacy groups than gynecological patients, and the information about CAM, which is provided for those patients, is abundant. Thus, supply and demand could meet with regard to CAM.
Only a few studies have been concerned with QoL and LS as primary study objectives in patients using CAM. A case-control study that compared breast cancer patients in an anthroposophic hospital using complementary medicine with patients in another hospital who were receiving conventional care reported improvements in QoL in the group treated with complementary and anthroposophic care [6, 7]. However, the patients recruited for the study may not reflect an average group of cancer patients, and there may have been some selection bias, as care in a hospital with an anthroposophic approach is much more intensive, and the patients stated that they were seeking spiritual insight, which would be a specialized goal in treatment and medical care. A large study by Burstein et al. [5] assessed the health-related QoL in relation to the use of alternative medicine. The authors found that the use of alternative medicine was a marker of greater psychosocial distress and a poorer QoL 3 months after the diagnosis of breast cancer. The extent to which the use of complementary therapies in an attempt to alleviate physical or psychological symptoms may influence the results has also been examined [18]. The present study did not confirm that LS was any poorer. On the contrary, it documented better LS for CAM users in the areas of health status and familial conditions. Sexual satisfaction remained unaltered, whereas Burstein et al. [5] stated that sexual dissatisfaction was greater in women using CAM.
A strict assessment of the influence of CAM on QoL and LS is difficult. Response shift phenomena may lead to difficulties in longitudinal assessments [24, 25], and the QoL questionnaires used in clinical trials may not reflect patients’ self-stated QoL and LS [26]. In addition, studies that evaluate the QoL prospectively do not allow other noninvestigational anticancer drugs to be used. However, the effect that the use of CAM can contribute to an improvement in the patients’ physical or psychological well-being has been reported before [17].
An attempt was made in this study to solve this problem by using the status quo of satisfaction stated by the patient at the time of the interview. A retrospective statement regarding satisfaction before the diagnosis of cancer was compared with the statement given at the time of the interview, providing a subjective assessment of improvement or deterioration. The large sample size may minimize the influence of interindividual differences in adjusting to cancer [4, 15]. However, this effect on the results cannot be measured.
The high percentage of patients who are encouraged by their physicians to use unproven CAM treatments is surprising. One reason for this may be the high percentage of women receiving at least partial refunding for such treatments from their health insurance companies in Germany.
In the perception of gynecologic oncology patients, the disease has measurable negative or positive effects on QoL and LS. CAM use is associated less frequently with a decline in satisfaction relative to the main topic of health status. A significant group of patients are more satisfied with their health status, with a difference amounting to approximately 15%. On the one hand, efficacy data are lacking, and large placebo-controlled trials including QoL objectives have not been conducted; however, CAM use does have an effect on LS. Whether this effect is mediated by the CAM itself or by a mechanism that helps reduce psychological distress is a topic for further research.
References
Astin JA (1999) Use of alternative medicine by women with breast cancer. N Engl J Med 341:1156, author reply 1156–1157
Barnes PM, Powell-Griner E, McFann K, Nahin RL (2004) Complementary and alternative medicine use among adults: United States, 2002. Adv Data:1–19
Bertz J, Hentschel S, Hundsdörfer G, Kaatsch P, Katalinic A, Lehnert M, Schön D, Stegmaier C, Ziegler H (2004) Krebs in Deutschland (Cancer in Germany), 4th edn. Saarbrücken
Brennan J (2001) Adjustment to cancer-coping or personal transition?
Burstein HJ, Gelber S, Guadagnoli E, Weeks JC (1999) Use of alternative medicine by women with early-stage breast cancer. N Engl J Med 340:1733–1739
Carlsson M, Arman M, Backman M, Flatters U, Hatschek T, Hamrin E (2004) Evaluation of quality of life/life satisfaction in women with breast cancer in complementary and conventional care. Acta Oncol 43:27–34
Carlsson M, Arman M, Backman M, Hamrin E (2001) Perceived quality of life and coping for Swedish women with breast cancer who choose complementary medicine. Cancer Nurs 24:395–401
Cassileth BR, Deng G (2004) Complementary and alternative therapies for cancer. Oncologist 9:80–89
Chrystal K, Allan S, Forgeson G, Isaacs R (2003) The use of complementary/alternative medicine by cancer patients in a New Zealand regional cancer treatment centre. N Z Med J 116:U296
Cui Y, Shu XO, Gao Y, Wen W, Ruan ZX, Jin F, Zheng W (2004) Use of complementary and alternative medicine by Chinese women with breast cancer. Breast Cancer Res Treat 85:263–270
Drew AK, Myers SP (1997) Safety issues in herbal medicine: implications for the health professions. Med J Aust 166:538–541
Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompay M, Kessler RC (1998) Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. JAMA 280:1569–1575
Ernst E, Cassileth BR (1998) The prevalence of complementary/alternative medicine in cancer: a systematic review. Cancer 83:777–782
Fasching PA, Nicolaisen-Murmann K, Lux MP, Bani M, Thiel F, Bender HG, Beckmann MW, Ackermann S (2007) Changes in satisfaction in patients with gynecological and breast malignancies: an analysis with the Socio-Economic Satisfaction and Quality of Life (SES-QOL) questionnaire. Eur J Cancer Care (in press)
Ganz PA, Guadagnoli E, Landrum MB, Lash TL, Rakowski W, Silliman RA (2003) Breast cancer in older women: quality of life and psychosocial adjustment in the 15 months after diagnosis. J Clin Oncol 21:4027–4033
Ganz PA, Kwan L, Stanton AL, Krupnick JL, Rowland JH, Meyerowitz BE, Bower JE, Belin TR (2004) Quality of life at the end of primary treatment of breast cancer: first results from the moving beyond cancer randomized trial. J Natl Cancer Inst 96:376–387
Kappauf H, Leykauf-Ammon D, Bruntsch U, Horneber M, Kaiser G, Buschel G, Gallmeier WM (2000) Use of and attitudes held towards unconventional medicine by patients in a department of internal medicine/oncology and haematology. Support Care Cancer 8:314–322
Knobf MT, Pasacreta J (1999) Use of alternative medicine by women with breast cancer. N Engl J Med 341:1156–1157
Lee MM, Chang JS, Jacobs B, Wrensch MR (2002) Complementary and alternative medicine use among men with prostate cancer in 4 ethnic populations. Am J Public Health 92:1606–1609
Lutz S, Spence C, Chow E, Janjan N, Connor S (2004) Survey on use of palliative radiotherapy in hospice care. J Clin Oncol 22:3581–3586
Marstedt G, Moebus S (2004) Inanspruchnahme alternativer Methoden in der Medizin. Robert-Koch-Insitut, Berlin
Nicolaisen-Murmann K, Thiel F, Mohrmann S, Grünewald E, Ackermann S, Bender HG, Beckmann MW, Fasching PA (2005) Complementary and alternative Methods (CAM) in women with gynecologic and breast malignancies-a multicenter study estimating prevalence and motivation. Geburtshilfe Frauenheilkd 65:1–8
Sollner W, Maislinger S, DeVries A, Steixner E, Rumpold G, Lukas P (2000) Use of complementary and alternative medicine by cancer patients is not associated with perceived distress or poor compliance with standard treatment but with active coping behavior: a survey. Cancer 89:873–880
Sprangers MA (2002) Quality-of-life assessment in oncology. Achievements and challenges. Acta Oncol 41:229–237
Sprangers MA, Moinpour CM, Moynihan TJ, Patrick DL, Revicki DA (2002) Assessing meaningful change in quality of life over time: a users’ guide for clinicians. Mayo Clin Proc 77:561–571
Waldron D, O’Boyle CA, Kearney M, Moriarty M, Carney D (1999) Quality-of-life measurement in advanced cancer: assessing the individual. J Clin Oncol 17:3603–3611
Weiger WA, Smith M, Boon H, Richardson MA, Kaptchuk TJ, Eisenberg DM (2002) Advising patients who seek complementary and alternative medical therapies for cancer. Ann Intern Med 137:889–903
Werneke U, Earl J, Seydel C, Horn O, Crichton P, Fannon D (2004) Potential health risks of complementary alternative medicines in cancer patients. Br J Cancer 90:408–413
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fasching, P.A., Thiel, F., Nicolaisen-Murmann, K. et al. Association of complementary methods with quality of life and life satisfaction in patients with gynecologic and breast malignancies. Support Care Cancer 15, 1277–1284 (2007). https://doi.org/10.1007/s00520-007-0231-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-007-0231-1