Abstract
Goals of work
To explore the major factors important in decision making for whole-brain radiotherapy (WBRT) for patients with brain metastases and their caregivers.
Patients and methods
Two parallel qualitative studies, one for patients and one for caregivers of patients with newly diagnosed brain metastases, were conducted. Semistructured interviews were conducted and audiotaped with each participant. Content analysis and theme extraction of the transcripts were undertaken to identify recurring themes and relational patterns.
Results
Twenty patients and 19 caregivers (including eight patient and caregiver pairs) were recruited into the study. Four major factors were identified to influence decision making of whole-brain radiation: hope, knowledge, expectations of radiation therapy, and current symptoms. Analysis reveals that patients generally focus on current informational needs, while caregivers want more information about the future (e.g., life expectancy and anticipated symptoms). Caregivers expressed frustration when unable to explore future needs because patients were unprepared to discuss prognostic issues. Participants expressed substantial relief when offered WBRT after the diagnosis, but WBRT is often considered the only available plan rather than an informed choice.
Conclusions
Given the importance of caregivers in the care of patients with brain metastases, fulfilling their unique informational needs appears to require more attention. The blurred boundary between hopes and expectations for WBRT creates unique challenges in joint treatment decision making for patients with brain metastases and their caregivers.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
About 25% of cancer patients are diagnosed with brain metastases [43]. Brain metastases can be the initial presentation of an incurable illness, or it can present during the trajectory of a malignancy previously thought to be curable. The diagnosis of brain metastases is often a sudden one, following an event such as hemiplegia, seizure activity, severe headaches, nausea, and vomiting. Depending on the primary site, life expectancy is almost uniformly limited to less than 6 months [11, 12].
For selected patient groups with solitary metastases, aggressive interventions are available. These include surgery [30, 33–35], stereotactic radiotherapy [22, 41], and whole-brain radiotherapy (WBRT), where there are good data to support survival benefit and improved local control. For the vast majority of patients, however, where there are multiple metastases and active systemic disease, the outlook is poor. The Radiation Therapy Oncology Group (RTOG) prognostic grouping describes patients with life expectancy ranging from 2 to 6 months, depending on prognostic factors. WBRT represents the major treatment modality available to these patients and typically consists of 20–30 Gy in five to ten fractions of daily radiation therapy given over 1–2 weeks [2, 3, 8, 16, 17, 24, 32, 38]. For these patients, dealing with the psychological and physical impact of brain metastases presents unique challenges to patients and their families in terms of coping and treatment decision making.
There have been no previous studies addressing the informational needs and decision making of patients with brain metastases. Leavitt et al. found that patients with brain tumors required more information with regard to the side effects of radiation and symptom management, and support groups were valuable sources of information for patients [26]. Lantz and Fox identified the importance of information being delivered to those patients in ways that are easy to comprehend [25].
Caregivers are important partners in the care of patients with brain metastases, having to take more significant roles than in many other advanced cancer situations. For example, decision-making capacities (e.g., appreciation, reasoning, and the ability to express a consistent choice) may be impaired in seriously ill patients [4, 7, 29, 36], especially in those with cognitive impairment, as is commonly seen in patients with brain metastasis. In taking on such roles, caregivers project their own values onto the decision-making process, which may differ from patient values. The following are factors that need to be considered when optimizing the care of patients with brain metastases: how caregivers handle decision making, whether they themselves are aware of potential discrepancies, and how decisions may impact on the patient–caregiver relationship and their relationship with the health care team.
The purpose of this paper is to describe major factors important in decision making for WBRT for patients and caregivers at the time of radiation consultation. The result of this study provides useful information for health care professionals in helping patients and caregivers adopt more realistic hope and make informed treatment decisions.
Patients and methods
Qualitative descriptive methods have been used to guide study development [27, 39]. Two parallel qualitative studies, one for patients and one for caregivers of patients, were conducted. The University Health Network Research Ethics Board reviewed and approved this study. Purposeful sampling was used to select the participants. Individuals were selected for their ability to articulate their experience with brain metastases.
Inclusion criteria were patients or caregivers of patients who were diagnosed with brain metastases from solid tumors within the past 2 months and were assessed for consideration of brain radiotherapy during that time. Exclusion criteria were language barriers precluding an interview, and patients or caregivers of patients with a life expectancy of more than 1 year or with primary brain tumors as those patients may be eligible for more aggressive therapies.
Data were collected by a single, open-ended, semistructured interview to fully explore the perspectives of patients and caregivers about their experiences with brain metastases. The interview was scheduled within 2 weeks of each patient’s initial consultation for consideration of radiotherapy and was conducted during their treatment course. All patients interviewed subsequently received WBRT treatments. This consisted of 400 cGy given daily for 5 days for a total of 2,000 cGy. Prompts used in the interviews are listed in Table 1. Patients’ medical charts were also reviewed to further verify information about medical status. The length of the interview was 30–90 min, and it was tape-recorded and transcribed. Content analytic techniques were used for data analysis. An iterative process by which new patterns and themes emerge with contributions from new participants was used [27]. A sample size of 20 patients and caregivers, or when the data reach the point of thematic saturation, was planned. Our sample size is not intended to provide sufficient power to provide estimates in regard to the generalizability of the identified themes in the general population. Investigators read and independently coded based on the first six interviews. The initial coding was applied to subsequent interviews with ongoing revisions to incorporate new patterns. The codes were divided into categories and further condensed and organized into themes. Regular team debriefing and independent coding and analysis assessed credibility of the study. Interrater reliability of the study was maintained through discussing and reexamining coding discrepancies to ensure consistency. Analysis was continued until no new information was identified.
Results
Between November 2003 and July 2004, a total of 39 patients and caregivers (20 patients and 19 caregivers), including eight patient and caregiver pairs, were recruited into the study (Tables 2 and 3). Patients were generally older than the caregivers in this sample. The median age of patients and caregivers were 62 and 42 years, respectively. There was a higher portion of male patients (75% male) and a predominance of female caregivers (89% female). The primary tumors of the patients were 13 (65%) lung, 3 (15%) renal, 2 (10%) melanoma, 1 (5%) colon, and 1 (5%) mesothelioma. Fifty-five percent of patients had an ECOG (Eastern Cooperative Oncology Group) performance status of 1, and 35% had an ECOG performance status of 2. In the 19 caregivers, there were 8 (42%) daughters, 7 (37%) wives, 2 (11%) sisters, and 2 (11%) husbands.
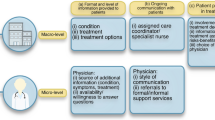
Four major factors were identified to influence decision making of whole-brain radiation: hope, knowledge, expectations of radiation therapy, and current symptoms (Fig. 1). Descriptions of the four themes with quotes to illustrate the factors are included below.
Hope
Hope is a major factor that influences the expectations of radiation therapy among patients and caregivers. Hope is generally defined as “a desire accompanied by expectation of or belief in fulfillment/success” (Merriam-Webster OnLine;http://www.m-w.com/dictionary.htm). In the health care setting, hope is defined as “a multidimensional dynamic life force characterized by a confident yet uncertain expectation of achieving a future good which, to the hoping person, is realistically possible and personally significant”[10]. The nature of hope varies depending on the participants. Their responses about hope fell into four categories: (1) cure, (2) increased life expectancy, (3) improved symptom management, and (4) acceptance. The categories were organized based on decreasing level of expectations for treatment. In the fourth category, participants acknowledged that treatment may not provide benefits.
Hope for cure
Cure was defined by participants as the eradication of all tumors. As one patient in this category said,
-
1.
Patient: I will continue to improve, I believe. Confidently.
-
2.
Interviewer: Do you think the tumors will go away completely, resolve part way?
-
3.
Patient: I think completely for me.
Caregivers expressed that they wanted to maintain the patient’s hope for cure because they feared their loved ones would become desperate or not be able to cope with the news of death. A sister explained,
Well, I haven’t... We haven’t told her that she’s going to die. We’ve told her everything but. We’ve told her she’s got cancer and where it is, and that she’s very ill. But I’ve told the doctors that this is a person who’s always lived in fear and depression, and I didn’t want to end her life that way. (Caregiver)
Generally however, patients were aware of the imminence of death.
One daughter stated, “And usually cancer to her means you’re going to die automatically... I mean she keeps telling me she’s not afraid to die, and that she’s not in any pain. So she knows”. (Caregiver) In our study sample, 16 of 20 patients said that end-of-life issues were on their minds and generally welcomed invitations from family members to discuss them.
Hope for increased life expectancy
The second category of what participants hope for is increased life expectancy. Both patients and caregivers expressed the importance of the fact that there were treatments available to deal with the situation and provided an opportunity to extend life. They experienced substantial relief when WBRT was offered. One patient described,
I’m just glad that they didn’t say to me: I’m sorry ... , there’s nothing more we can do. I mean at least with radiation therapy I’ve got some hope that I’ve got more time. I mean I honestly thought on Sunday they were going to say: There’s nothing we can do. You’ve got weeks. I really did. So this is a little bit of hope. (Patient)
Another caregiver stated,
We are given a life expectancy of six months to a year, but that could change. I’m sure it can be two years, three years, maybe even ten years. But I just would like to know if the cancerous cell didn’t go anywhere else. And this way maybe check on that before it arises. This way if we catch it maybe we can treat that too. (Caregiver)
Patients and caregivers demonstrated the great therapeutic benefit they felt by just receiving treatment. They expressed the belief that they would improve and were continuing their cancer fight. As one patient stated, “But I mean I’ll fight. I’ll fight. And, you know, somebody wants to fight with me, I’ll go right along with it”. In oncology care, especially with a curative intent, the analogy of a battle with cancer is used to motivate patients to continue treatments and cope with the side effects. Cancer is considered the enemy that can be beaten with the patients’ effort and medical treatments. However, there were concerns expressed about whether the analogy of battle with cancer remains appropriate for brain metastases patients. This analogy can lead to great suffering if patients or caregivers felt they were losing their fight with cancer. One patient said, “I mean I know like having cancer is a bit like being an alcoholic—you got to kind of be looking over your shoulder, but I really thought I’d won. And I wasn’t winning”.
Patients and caregivers with responses in the first two categories of hope typically requested more investigations to follow disease progression and to rule out or treat other metastasis elsewhere in the body. One spouse stated, “I think knowing that it went to the brain ... maybe she should be told to get a CT scan on the body. Just to see”. (Caregiver)
Hope for improved symptoms
The third category that participants hope for is improved symptom management. Areas of control important to patients included pain, cognitive ability, and body function. These factors influence the patients’ independence and quality of life. Participants expressed the importance of preserving one’s capacity to cope with the situation. Patients and caregivers experienced a loss of direction, hopelessness, and great suffering when they no longer felt in control. Below are quotes to illustrate this category.
Pain: A patient indicated, “Yes. I don’t mind dying either. I don’t mind dying in peace ... But to go with pain and suffering...it’s too much”.
Cognitive ability: A caregiver shared the importance of the patient “feeling more himself, not feeling as confused. I think if he feels more himself, he’ll be much happier”.
Independence: A patient described, “So if I can stand downstairs and do a little more woodworking... It makes me feel functional. It makes me feel like I have some purpose. Right now I just hang around and feel innate”.
Acceptance
The fourth category of hope is acceptance, which occurs when participants acknowledge that treatment may not give benefits. Below are quotes to illustrate this category. A patient explained, “You have to sort of accept what you have and whatever it’s going to dish out. That’s where I am”. Another patient said, “With the brain now I hope it’ll be stopped for maybe a few years. I’m thinking that. But if not, well, my number’s come up. That’s the way I look at it. I’m prepared one way or the other”.
Patients explained that because the future is so unpredictable and unknown, they prefer taking things 1 day at a time. As one patient explained,
It’s the sort of thing that you have to take one step at a time, to see how it goes, without making major decisions, because we don’t know what this cancer is doing to me, and how far it’s progressed, or how it’s going to affect me as we go through treatment, etc. And when you’re dealing with something like this here, you can’t make too long-range plans. You can think about them, but you have to see how things turn out before you do anything. (Patient)
Patients in this category generally felt very fortunate and believed they had lived a good life. With the acceptance of death, patients were open to prepare for the end of life. Caregivers expressed that it was easier to accept the patient’s illness if they felt that the patient had a good life, was dying of old age, or if the patient would have relief from their sufferings. This lady explained,
When you reach a certain age... not that you’re supposed to die when you reach a certain age, but it’s more understood. When you reach like eighty-two years old, you start wondering are they going to last to the next year or two. You know, ‘cause that’s the way life is. (Caregiver)
When comparing patients and caregivers, it is noted that pairs may not necessarily be operating in the same categories of hope. Below is a quote from a patient describing the disappointment she had because her children had not accepted the severity of her illness.
Over the last few years I’ve felt like they [children] were more or less in denial of the whole thing. Of course no one wants to lose their mom, and it’s easier just to pretend that it’s not something serious. But I think that now this has happened... I directly told them that this is very serious ... and if there isn’t a lot of time, we should make the best use of the time. Like don’t deny it anymore ... I would love more support from my daughter, but I don’t really get it. My son is very good, but I just find that he doesn’t want to accept the reality. (Patient)
Knowledge
Another factor that influences the expectation of radiation therapy among patients and caregivers is knowledge. Patients and caregivers had different information needs. Patients generally wanted to focus more information on the present, while the caregivers wanted more information about the future.
Both patients and caregivers generally felt the need to be proactive about asking questions. One daughter described,
I just wish that the doctors were more direct in answering, or at least providing information, because as a patient you don’t always have the right questions to ask ... When I received the news that my mom had cancer, it was hard, and I wasn’t able to think ... At that time I didn’t have questions. And I think the doctors should have taken the proactive step to say: Okay, well, this is what’s going to happen. Like explain it more in detail. Or be more direct in what to expect for the future. But you just can’t think. It’s very serious. It’s very serious. And that’s it ... I didn’t have any more information, so I was left to conclude it with my own thoughts. Like I had to read in between the lines of what they were saying. So I don’t think that was fair. (Caregiver)
However, there are some patients (2/20) and caregivers (1/19) who do not want such information. As this patient said, “I didn’t even read what was wrong with me because I didn’t want to know, I know whatever they’re curing but I didn’t want to know much”. In this circumstance it is important to explore the patients’/caregivers’ anxieties and support them in making the most informed choice they are capable of making at the time.
Consistent with decision making in other cancer patients [9, 14], while some patients want more information, others have less need for knowledge to facilitate their decision making, preferring instead to defer to the knowledge of their doctors.
Well, I totally trust my medical doctors. I don’t see any other way ... There’s two things I believe in—my medical treatment and my belief in God ... I just believe that. I think that nowadays the doctors are right on the upper levels of knowing what they know, and I should trust them. (Patient)
Caregivers expressed the importance of anticipatory guidance, which is defined in this paper as instructions or descriptions provided to help patients and caregivers prepare for progression of the disease. One daughter said, “You know, I can’t stay indefinitely off work. I can’t project what will happen or what I’m going to do”. This husband described,
This way if you give them a life expectancy, I guess you can do a lot of things too. Like maybe if there’s something that she wanted to do that she feels comfortable talking with me about that. I can maybe do that for her and make that dream happen.
Caregivers expressed frustration when unable to explore future needs because patients were unprepared to deal with prognostic issues. Below are two caregivers sharing their thoughts:
I need to know life expectancy. I need to know what’s going to happen as this progress. What can I do? What should I do? And what should I be expecting to do? Like right now my main concern was that if he gets better, can he travel?
I know my mom just doesn’t want to know too much right now. She is in a minute-by-minute, hour-by-hour battle just to keep her spirits up and quell her own anxiety. So I don’t want to ask too many questions when my mom is there because... for fear that I might be forcing information upon her that she’s not ready right now to receive.
Expectations of radiotherapy
The two factors, hope and knowledge, direct expectations of radiation therapy, which in turn influences the decision-making process.
Hope
A wife explained,
He’s a strong man. He’s healthy. He wants to live. And that’s why, I think, this is so devastating, ‘cause he wants it so badly. He doesn’t want to die. And I keep hoping beyond hope ... that radiotherapy is going give us more time. (Caregiver)
Knowledge
A daughter said,
Without radiation he’s getting three to six months. With radiation he’s given three to six months. So the only thing the doctor said it will change is the way of life. Like more or less the symptoms are gone. So he’s got better quality of life within those three to six months. (Caregiver)
Some patients paradoxically exhibited both a knowledge of their prognosis and hope that is inconsistent with that knowledge. Patients were able to acknowledge the terminal nature of their illness and still remain hopeful for a cure or remission. One lady said, “I’ll be around for another ten years. This brain tumor is going to be cured. It’s going to be shrunk to nothin”. However, when asked regarding the prognosis of her disease she said, “Well it’s not curable disease”. At times, there appeared to be a tension between a patient’s hope for cure and a suppressed realization of their true prognosis.
The process of decision making
Generally, patients and caregivers did not see the acceptance of WBRT as a choice but rather the only option available to them because supportive care was not viewed as a real alternative. A patient said, “And when you’re told that’s pretty much the only chance you have, side effects be damned. You’re going to do it, right”? A wife explained, “We choose WBRT because that was our only option... It wasn’t a difficult choice at all. It was that or nothing, and I’m glad we had something”. (Caregiver)
Some caregivers strongly believe in the need to protect patients from distressing information, and that the caregivers should make the treatment decisions. This daughter said,
... in terms of her thinking that she only have five cycles of radiation left ... so she should be getting better at some point. That’s just (to) make her hopeful... And going through the process of radiation. If she knew she was going to die, she wouldn’t go through radiation. (Caregiver)
However, caregivers may feel burdened with the responsibility of the decision if they make treatment decisions in isolation. A wife described, “I’m afraid that... I don’t want to feel guilty afterwards that I’ve talked him into doing something and then it’s made him feel worse or whatever”. (Caregiver)
Current symptoms
Current symptoms is an important factor that contributes to decision making. If the symptoms were considered intolerable, patients were more likely to choose radiotherapy.
-
1.
Interviewer: Were you concerned about any side effects?
-
2.
Caregiver: Can’t get a lot worse than it already is.
-
3.
Interviewer: What do you mean by that?
-
4.
Caregiver: He’s very sick. He’s very, very sick. I mean, try anything. That’s his attitude. He feels very strongly about it.
Discussion
Treatment decision making for brain metastasis patients and their caregivers poses unique challenges given its profound potential impact on life expectancy and cognitive ability. Our study identified hope, knowledge, expectations of radiotherapy, and current symptoms as important factors in the process of decision making.
When exploring what patients and caregivers hope for as treatment outcome, there was a great variability ranging from cure, better symptom control, to acceptance. Kirk et al. identified the importance of hopeful messages provided by health professionals. Both our study and Kirk et al. identified that patients and caregivers expressed “compartmentalised awareness”, concurrently recognizing the terminal nature of the illness, while retaining a need for a sense of hope [20]. Patients appear to oscillate between a state of continuing to live and plan and a state of preparing for death [5]. Recognizing this duality and helping patients reframe hope is highly beneficial. Realistic hope has been identified by studies to provide considerable support for patients [18, 23, 31, 37, 42]. Unrealistic hopes can be destructive because they impede patients’ ability to make appropriate treatment decisions, lead to ineffective use of patients’ remaining time, and promote strategies to delay dealing with difficult issues [28].
Gaps between patient’s expectations and their actual circumstances are a major determinant of quality of life [6]. Calman’s model suggests that realistic goals can improve quality of life by reducing disappointments from unrealistic expectations. Our participants have emphasized the importance of providing honest information but leaving the door open to hope for miracles. One approach that health care professionals can use is to encourage patients to “hope for the best and prepare for the worst”. This approach may help patients and caregivers create a treatment plan that is receptive to various potential outcomes for the patient [5]. If this approach is taken, it is important to explore the patient’s hopes and begin the work of reframing hope when appropriate.
We found that many patients and caregivers have limited knowledge about their prognosis even after the radiotherapy consultation. Many also expressed the need to be proactive about asking questions to obtain information. Even with direct request from patients for survival estimates, physicians have reported that they will provide frank estimate of life expectancy only 37% of the time [40]. Participants expressed distress, frustration, and uncertainty when they perceived having insufficient information. Health care providers can enhance communication by proactively asking patients about what they know about their illness and what they want to know. The use of a simple form between patients and physicians that includes specific information such as diagnosis, prognosis, stage of the illness, treatment goals, and options and contact information can be an effective communication tool [13] and a starting point in the radiation consultation. The form can create a framework for a comprehensive discussion between health care workers and patients/caregivers and provide a written record for patients about their diseases [13, 15].
There is an average age gap of approximately 20 years between the patients and caregivers. However, we did not observe any major discrepancies in the values and perspectives that may have arisen from this. In this study, the only area where there is a gap between the needs of the patients and the caregivers lies in the need for anticipatory guidance. Caregivers described a greater need to know what the future holds, while patients may prefer to avoid this information. The reason for this is unlikely to be due to the age difference, but rather, likely relates to the fact that caregivers have an absolute need to be able to handle the future given their capacity as the caregiver, while patients could, with their caregiver by their side, take a more passive role. Both Kirk et al. [20] and our study found that patients require more information about managing current symptoms, while caregivers need more information about prognosis and anticipatory guidance for future care needs. Information exchange on those latter topics may be limited if patients are not prepared or are perceived as not prepared to handle longer-term information. Providing opportunities for caregivers to obtain additional information may be important in the treatment decision-making process. It is recommended that time be set aside, if the patient agrees, in which a health care worker and the caregiver can discuss concerns alone. Provision of additional resources through electronic media, including online resources that include clips of interviews with patients and short stories can be useful complementary strategies to facilitate anticipatory guidance [19].
Radiation consultation occurs within days to weeks after the diagnosis of brain metastases. This is a very short time for patients and their caregivers to absorb distressing information. While intense information exchange may occur at the treatment-decision stage, the opportunity to fulfill informational needs may be greatest at the conclusion of the treatment, when the pressure for treatment decision making has been alleviated. Participants have also indicated that learning about the experiences of others would be a comfort and a reassurance to them. More longitudinal information provision through an ongoing and continual education process with the family physician and/or palliative care doctors may be useful in providing knowledge to patients and caregivers when they are less overwhelmed.
Our participants did not see the acceptance of WBRT as a choice but rather as the only option. Practically, alternative options include delaying radiation therapy with steroid therapy alone to manage symptoms and, for selected patients, systemic chemotherapy such as temozolomide may be offered. But more significantly, the importance of realigning their expectations to what is realistic as well as adequate pain and symptom management cannot be overemphasized. Patients appear to have difficulty considering symptom management as a feasible option compared to radiotherapy, implying the need for more education for both health care professionals and patients in this domain. Similarly, Koedoot and de Haes [21] found that patients accepted chemotherapy because they perceived it as the only remaining option. Medical oncologists generally provide only one explanatory sentence to supportive care, and the nature and consequence of that option were not explained [21]. Accepting aggressive treatment was thought to provide both patients and physicians with a sense of control over the disease [21]. It may be beneficial for health care workers to devote more time to receptive patients and caregivers to discuss the nature of supportive care, including providing adequate pain and symptom management, living as normally as possible, and strengthening the relations with loved ones [1, 21].
One limitation of this study is that only patients with better performance status were able to participate. All participants had elected to receive radiotherapy. It is probable that sicker patients, those who are not radiotherapy candidates, or those that declined radiotherapy may have different perspectives.
Conclusions
The process of decision making in patients and caregivers with brain metastases brings unique complexity. Both hope and factual information contribute to forming the expectation of radiotherapy treatments. It is thought that the paradox of hoping for a miracle and realizing the terminal nature of their illness is a way patients and caregivers initially cope at a time of crisis. As health care workers, respecting the need for hope while simultaneously helping patients prepare for the dying process can help them gradually adjust to the diagnosis of brain metastases rather than triggering a violent confrontation with reality. Proactively providing disease information and the goals of radiation therapy to receptive patients and spending more time explaining alternative options can help patients recognize their lost autonomy. Issues uncovered in this study will facilitate a better understanding of the factors influencing treatment decision making in patients with brain metastases. This would pave the way to improving joint treatment decision making for patients and their families with this devastating complication of cancer.
References
Benzein E, Norberg A, Saveman BI (2001) The meaning of the lived experience of hope in patients with cancer in palliative home care. Palliat Med 15:117–126
Borgelt B, Gelber R, Larson M et al (1981) Ultra-rapid high dose irradiation schedules for the palliation of brain metastases: final results of the first two studies by the Radiation Therapy Oncology Group. Int J Radiat Oncol Biol Phys 7:1633–1638
Borgelt BB, Gelber R, Brady LW et al (1981) The palliation of hepatic metastases: results of the Radiation Therapy Oncology Group pilot study. Int J Radiat Oncol Biol Phys 7:587–591
Breitbart W, Bruera E, Choichinov H et al (1995) Neuropsychiatric syndromes and psychological symptoms in patients with advanced cancer. J Pain Symptom Manage 10:131–141
Brody JD (2003) Hope for the best, and prepare for the worst. Ann Intern Med 139:791–792
Calman KC (1984) Quality of life in cancer patients—an hypothesis. J Med Ethics 10:124–127
Casarett DJ (2003) Assessing decision-making capacity in the setting of palliative care research. J Pain Symptom Manage 25:S6–S13
Chatani M, Matayoshi Y, Masaki N et al (1994) Radiation therapy for brain metastases from lung carcinoma. Prospective randomized trial according to the level of lactate dehydrogenase. Strahlenther Onkol 170:155–161
Degner LF, Kristjanson LJ, Bowman D (1997) Information needs and decisional preferences in women with breast cancer. JAMA 277:1485–1492
Dufault K, Martocchio BC (1985) Hope: its spheres and dimensions. Nurs Clin North Am 20:379–391
Gaspar L, Scott C, Rotman M et al (1997) Recursive partitioning analysis (RPA) of prognostic factors in three Radiation Therapy Oncology Group (RTOG) brain metastases trials. Int J Radiat Oncol Biol Phys 37:745–751
Gaspar LE, Scott C, Murray K et al (2000) Validation of the RTOG recursive partitioning analysis (RPA) classification of brain metastases. Int J Radiat Oncol Biol Phys 47:1001–1006
Gaston CM, Mitchell G (2005) Information giving and decision-making in patients with advanced cancer: a systematic review. Soc Sci Med 61:2252–2264
Gattelari M, Butow P, Tattersall MH (2001) Sharing decisions in cancer care. Soc Sci Med 52:1865–1878
Grandinetti D (1999) “Ethical hope”—a lifeline for sick patients. Med Econ 76:118, 121–122, 127–128
Haie-Meder C, Pellae-Cosset B, Laplanche A et al (1993) Results of a randomized clinical trial comparing two radiation schedules in the palliative treatment of brain metastases. Radiother Oncol 26:111–116
Harwood AR, Simpson WJ (1977) Radiation therapy of cerebral metastases: a randomized prospective clinical trial. Int J Radiat Oncol Biol Phys 2:1091–1094
Hileman JW, Lackery NR (1990) Self identified needs of patients with cancer at home and their home caregivers: a descriptive study. Oncol Nurs Forum 17:907–913
Jones J, Nyhof-Young J, Friedman A et al (2001) More than just a pamphlet: development of an innovative computer-based education program for cancer patients. Patient Educ Couns 44:271–281
Kirk P, Kirk I, Kristjanson LJ (2004) What do patients receiving palliative care for cancer and their families want to be told? BMJ 328:1343
Koedoot N, de Haes H (2003) Patient centered decision making in palliative cancer treatment: a world of paradoxes. Patient Educ Couns 50:43–49
Kondziolka D, Patel A, Lunsford LD et al (1999) Stereotactic radiosurgery plus whole brain radiotherapy versus radiotherapy alone for patients with multiple brain metastases. Int J Radiat Oncol Biol Phys 45:427–434
Kramer J, Links M (1994) Breaking bad news: realistic versus unrealistic hopes. Support Care Cancer 2:91–93
Kurtz JM, Gelber R, Brady LW et al (1981) The palliation of brain metastases in a favorable patient population: a randomized clinical trial by the Radiation Therapy Oncology Group. Int J Radiat Oncol Biol Phys 7:891–895
Lantz C, Fox S (1998) The brain tumor experience and quality of life: a qualitative study. J Neurosci Nurs 30:245–252
Leavitt M, Lamb S, Voss B (1996) Brain tumor support group: content theme and mechanisms of support. Oncol Nurs Forum 23:1247–1256
Lincoln YS, Guba EG (1994) Competing paradigms in qualitative research. In: Denzin NK, Lincoln YS (eds) Handbook of qualitative research. Sage, Newbury Park, pp 105–117
Links M, Kramer J (1994) Breaking bad news: realistic versus unrealistic hopes. Support Care Cancer 2:91–93
Massie MJ, Holland J, Glass E (1983) Delirium in terminally ill cancer patients. Am J Psychiatry 140:1048–1050
Mintz AH, Kestle J, Rathbone MP et al (1996) A randomized trial to assess the efficacy of surgery in addition to radiotherapy in patients with a single cerebral metastasis. Cancer 78:1470–1476
Mok E, Martinson I, Wong TK (2004) Individual empowerment among Chinese cancer patients in Hong Kong. West J Nurs Res 26:59–75
Murray KJ, Scott C, Greenberg HM et al (1997) A randomized phase III study of accelerated hyperinfractionation versus standard in patients with unresected brain metastases: a report of the Radiation Therapy Oncology Group (RTOG) 9104. Int J Radiat Oncol Biol Phys 39:571–574
Noordijk EM, Vecht CJ, Haaxma-Reiche H et al (1994) The choice of treatment of single brain metastasis should be based on extracranial tumor activity and age. Int J Radiat Oncol Biol Phys 29:711–717
Patchell RA, Tibbs PA, Regine WF et al (1998) Postoperative radiotherapy in the treatment of single metastases to the brain: a randomized trial. JAMA 280:1485–1489
Patchell RA, Tibbs PA, Walsh JW et al (1990) A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med 322(8):494–500
Pereira J, Hanson J, Bruera E (1997) The frequency and clinical course of cognitive impairment in patients with terminal cancer. Cancer 79:835–842
Popp F, Sauer R (1988) Dealing with cancer—conversations with radiotherapy patients. Strahlenther Onkol 408–414:164
Priestman TJ, Dunn J, Brada M et al (1996) Final results of the Royal College of Radiologists’ trial comparing two different radiotherapy schedules in the treatment of cerebral metastases. Clin Oncol (R Coll Radiol) 8:308–315
Sandelowski M (1994) Notes on transcription. Res Nurs Health 17:311–314
Sculco L, Coyle N (2003) Communication and the patient/physician relationship: a phenomenological inquiry. J Support Oncol 1:206–215
Sperduto PW (2003) A review of stereotactic radiosurgery in the management of brain metastases. Technol Cancer Res Treat 2:105–110
Twycross RG, Lack SA (1990) Therapeutics in terminal cancer, 2nd edn. Churchill Livingstone, Edinburgh
Young B, Johnson JD (1996) Demographics of brain metastasis. Neurosurg Clin N Am 7(3):337–344
Acknowledgement
This study was generously supported by the Allan Kerbel Fund in Symptom Control.
Author information
Authors and Affiliations
Corresponding author
Additional information
The content of this manuscript has been presented in part at the 16th International Symposium Multinational Association of Supportive Care in Cancer.
Rights and permissions
About this article
Cite this article
Sze, J., Marisette, S., Williams, D. et al. Decision making in palliative radiation therapy: reframing hope in caregivers and patients with brain metastases. Support Care Cancer 14, 1055–1063 (2006). https://doi.org/10.1007/s00520-006-0032-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-006-0032-y