Abstract
Goals of work
The purpose of this study was to better understand various variables related to food intake and eating problems in children with cancer during their chemotherapy.
Patients and methods
Twenty-two consecutively admitted children, diagnosed with cancer and undergoing chemotherapy, participated in this study. Twenty-one of them, their parents and attending nurses participated in semi-structured interviews. Ten of the children underwent a taste acuity test, and recognition thresholds for the four basic tastes were determined.
Main results
The shared view of both children and parents was that altered taste was the predominant cause of the eating problems. In contrast, the nurses perceived that nausea was the most important cause of the children’s eating problems. In addition, psychological aspects such as learned food aversions and negative attitudes towards hospital food were regarded as important by children, parents and nurses. The taste test showed that the patients had higher thresholds for bitter taste and made more taste recognition errors compared to controls.
Conclusions
Changes seem to exist both in the primary gustatory sense as well as in food perception in paediatric cancer patients undergoing chemotherapy. Single solutions, such as efforts to serve “tasty food”, do not suffice alone. A more effective solution may be to combine different strategies and combinations of oral, enteral and parenteral nutrition should be considered to prevent malnutrition.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several food-related problems are present in children with cancer during chemotherapy, for example, mucositis, nausea and loss of appetite [29]. Studies have confirmed the clinical impression that paediatric cancer patients undergoing chemotherapy have considerably lower oral energy and nutrient intakes than age-based recommendations [12, 19, 20, 37]. A child under treatment may become at risk of malnutrition [29]. Prevention of malnutrition is important, since it impairs specific defence mechanisms and increases morbidity and mortality due to infection [32]. Malnutrition may also result in altered pharmacokinetics, impaired drug metabolism, increased drug toxicity and altered response to treatment [24].
In a previous study, we confirmed that Swedish children undergoing chemotherapy had an average daily energy intake below that recommended for healthy children and a negative weight development after initiation of chemotherapy [33]. Improved mealtime routines were therefore instituted on the ward studied. We presumed that flexibility with regard to the menu and serving hours as well as food enrichment would give the children an opportunity to increase their energy and protein intake during their hospital stay. The improved routines included for example that a nursing assistant was assigned to the kitchen on the ward to prepare meals at short notice and that foods typically preferred by children and adolescents, energy dense snacks and a variety of commercial liquid nutritional supplements were easily available. However, a follow-up study performed after the establishment of these new mealtime routines showed that the energy intake was still below that recommended, and the weight development was still negative, despite efforts to serve tasty food on demand on the ward [34]. Furthermore, interviews with the parents indicated that both physiological factors, such as altered taste, and psychological factors, e.g. ward environment, may be important factors in poor food intake in these children [35].
The main hypotheses underlying this study were that both physiological and psychological aspects contribute to the eating problems and that changes in taste sensations may play a significant role in altered food intake in children undergoing chemotherapy. The goals of the work were (1) to assess the children’s own perception of the magnitude and nature of their eating problems, food preferences and aversions during hospitalisation after initiation of chemotherapy; (2) to assess the attitudes of parents and nurses regarding the nature of the child’s eating problems, food preferences and aversions; (3) to assess taste alteration by means of a taste acuity test and (4) to assess nutritional status by means of weight and height development up to 3 months after initiation of chemotherapy.
Participants and methods
Participants
Approval for the study was obtained from the Ethics Committee of the Faculty of Medicine and Odontology, Umeå University. The inclusion of children, their parents and nurses was carried out at the Paediatric Haematology and Oncology Unit, Umeå University Hospital. The unit is one of six paediatric oncology centres in Sweden and is a referral unit for Northern Sweden.
Consecutively admitted children aged 2 years or older at diagnosis, beginning their first chemotherapy during the period from September 2002 up to the first week of June 2004, were eligible for inclusion in the study. Initially, the families of these children received an information letter and were subsequently contacted by telephone to agree on the date and time of the interview, which was to take place at the time of a planned admission for therapy. In all, 27 children met the inclusion criteria. Of these 27 children, 22 (81%) agreed to participate. For more information and description of the children, see Table 1.
Only parents whose children participated in the study were interviewed. In many cases, both the mother and the father stayed with the child during hospitalisation, and the parents were allowed to decide which one of them would be interviewed. In total, 17 mothers and 12 fathers (median age 31 years, range 24–51) participated, and, in eight cases, both parents were interviewed.
To a great extent, both nurses and nursing assistants (later collectively referred to as nurses) take equally active parts in communication about food and eating with the patients, their parents and attending paediatric oncologists. Out of 23 attending nurses, 17 (2 males and 15 females, median age 41, range 23–64) were interviewed. Twelve were registered nurses and five were nursing assistants. The median years of experience in paediatric oncology were 7 years, with a range from 1 to 33 years.
Pharmacological treatment
The patients were treated according to current national or Nordic standard protocols [26], which included anti-mitotic drugs and various adjuvants, in many cases, delivered simultaneously according to the protocols. At the time of the interviews and taste acuity tests, the children were in different phases of their respective protocols. Among the chemotherapy drugs used, doxorubicin and methotrexate are associated with taste changes [9], ifosfamide, cytarabine and procarbazine/dacarbazine are emetogenic [3] and cisplatin and cyclophosphamide are associated with taste changes and are also highly emetogenic [3, 9]. Most children, especially those with acute lymphatic leukaemia, received corticosteroids in doses that may increase the appetite [28]. Anti-emetic drugs, primarily 5-HT3-receptor antagonists (e.g. ondansetron), were given in scheduled doses in relation to chemotherapy administration.
Ten patients received parenteral nutrition during certain periods during the treatment. Two children received enteral nutrition via gastrostomy shortly after treatment started. For two other children, gastrostomy and nasogastric tube, respectively, were considered, but were never used.
Interviews
The interviews were intended to capture information about experiences over time. Thus, it was desirable that the children were in various phases of active treatment. All interviews were performed by the same person (IS). The child and the parent/s were interviewed separately on the same day. The families of 18 children were interviewed either at the ward or in the child’s room in the ward, depending on the child’s age and condition. Three children had continued their treatment at the local hospital, and they as well as their parents were interviewed at their local hospital on a regular appointment. All of the interviewed nurses had cared for all of the interviewed children, and they were interviewed close in time to when the interviews with the children and parents were conducted.
The interviews were semi-structured and included open-ended questions, which allowed the participants to bring up matters they judged to be important. The main study questions were “What was your/your child/the child’s food intake like during the hospital stay following initiation of chemotherapy?” and “Are there any foods you/your child/the child liked or disliked after the initiation of chemotherapy?” This question was followed by “If so, what kind of food items in particular?” In addition, follow-up questions were asked to elucidate relevant aspects. The interviews, which lasted 15–90 min, were performed, transcribed verbatim and coded by the first author (IS) in accordance with content analysis [21]. The coding involves a systematic analysis of the person’s verbal responses. Sentences that contained information relevant to the interview questions were grouped into mutually exclusive categories, as described elsewhere [35]. A category answers the question “What?” [21] and can include several subcategories at varying levels of abstraction. The boundaries and the central characteristics of each main category and subcategory were discussed by the first (IS) and fourth (U-K KH) authors until a consensus was reached.
Taste acuity test
Ten of the older patients (Table 1) and an age- and sex-matched control group consisting of ten healthy non-nicotine-using volunteers from the same community participated. The test was performed between two chemotherapy cycles. The participants were presented with the taste stimulus in order for them to determine if the solution had a taste, and if it did, what taste it was. Taste recognition thresholds, the lowest concentration of a taste solution at which the taste can be correctly identified [30], were determined for sweet (sucrose), salty (sodium chloride), sour (citric acid) and bitter (quinine hydrochloride) solutions. The concentrations increased in nine steps and ranged from 3.90–88.4 mmol/l (millimoles per litre) for sucrose, 1.95–1,000 mmol/l for sodium chloride, 0.02–7.8 mmol/l for citric acid and 0.001–0.49 mmol/l for quinine hydrochloride. Deionised water served as a blank [25]. The up–down staircase method was applied [10]. Each participant was first acquainted with the different taste solutions by rinsing the mouth with the strongest solution of each taste. Ten millilitres of each test solution was then served in a clean glass beaker. The test solutions were presented in random order and in increasing concentrations. Between presentations, the participants rinsed their mouth with deionised water.
Questionnaire
At the time of the taste acuity test, the participants filled out a questionnaire with instructions to the patients to recall their experiences after start of chemotherapy. The questions with primarily “yes” or “no” alternatives concerned alterations in appetite, taste and smell and avoidance of certain foods. In addition, they were asked to write a description of the sensation in their own words.
Anthropometry
The patients were weighed to the nearest 100 g, and height was measured to the nearest 0.5 cm according to the routines at the ward. Weight and height data, collected at admission and then weekly during the first 6 weeks and at 3 months after start of treatment, were analysed and related to the Swedish growth charts [1] and expressed as standard deviation scores (SD).
Results
Interviews
Based on the interviews with the children, their parents and the nurses, two main categories could be identified: (1) causes of eating problems and (2) altered food choice.
Causes of eating problems
The subcategories altered taste, learned food aversions, nausea and vomiting, pain, loss of appetite, feeling ill, altered smell were identified in the statements of children, parents and nurses. The subcategory ward environment was identified in statements of the parents and nurses, while gaining control and protest against the situation were identified only in the statements of the nurses. Selected subcategories are presented below. Number (percentage) of children, parents and nurses contributing at least one statement to each subcategory are presented in Table 2.
Children
The most frequently mentioned cause of eating problems and decreased food intake was altered taste, which included statements by three children aged 4–11 years and six children aged 14–17 years, indicating that familiar and previously popular food items tasted different or lacked taste after initiation of chemotherapy. For example, red meat (three children), hot dogs and chicken (two children) tasted strange, water had an unpleasant taste (one child), sweets did not taste good any longer (two children), and potatoes and rice were perceived as tasteless (one child). One 15-year-old boy described an altered taste sensation for meat and salty foods:
I used to like popcorn. The popcorn was flavoured with cheese and it suddenly had no taste. But there was a change over time. Sometimes I could taste the salty taste, but it was a very strong salty taste! Hamburgers were disgusting. They tasted meaty and raw. French fries didn’t taste salty at all. They tasted like flour.
Learned food aversions, which can be allocated to psychological causes, were the second most frequently mentioned cause of eating problems. Food aversions were said to develop towards food or snacks that had become distasteful or had been consumed in close relation to chemotherapy that was followed by nausea. A 16-year-old girl described her experience:
Once I ate ice cream after I got my chemotherapy. After I had the medicine, I felt nauseous and vomited, so I can’t eat ice cream any longer.
Nausea and vomiting and pain from blisters in the mouth and abdomen were also mentioned as important causes. None of the children mentioned the impact of the ward environment, which was specified by the parents, or food refusal as a way of gaining control over the situation, or as a protest against the situation, which was mentioned by the nurses.
Parents
The parents also stated that, in their opinion, altered taste was the most important cause of the child’s decreased food intake. The parents of young children described mealtime situations, in which the child had begun to eat a certain food item, but then stopped eating and asked for another food item, or seemed dissatisfied and did not finish the meal. The mother of a child aged 3 years at initiation of chemotherapy, related the following:
He wanted something to eat. He took a bite but seemed dissatisfied, and asked for another food item. He didn’t finish his meals. He seemed frustrated. I wondered whether his taste had changed. He was too young to be able to tell me.
The parents perceived that nausea and vomiting and pain due to mucositis, or in the extremities, abdomen or throat, were important causes. Learned food aversions were perceived to develop secondary to nausea and the administration of chemotherapy. The mother of a 4-year-old child related the following:
She developed aversions to certain foods. She associated them with the treatment and avoided chocolate, because we gave her that during her first chemotherapy.
Altered smell refers to statements that the child was sensitive to the smell of food or any odour and/or to the smell of medicine when administered. The smell made the child feel nauseous. Ward environment included statements that the hospital environment had a negative impact on the child’s mood and affected food intake negatively. The mother of a child, who was 4 years old when chemotherapy was initiated, related the following:
As soon as she comes through the door to the ward, she loses her appetite. She becomes apathetic.
Nurses
The nurses perceived nausea and vomiting as the most important causes of poor food intake and a problem in spite of the scheduled administration of anti-emetics in association with chemotherapy. Anticipatory nausea, that is, nausea occurring before the administration of chemotherapy, was mentioned by two nurses. It was perceived as being triggered by the sight of the equipment used for drug administration. “Feeling ill” refers to statements about the effects of medication such as infections, fever and constipation. Psychological aspects were also perceived as important. The negative impact of the ward environment was the third most frequently mentioned cause. “Gaining some control over the situation” refers to statements that food refusal was perceived as a way for the child to gain some influence over the routines on the ward that governed most aspects of the child’s daily life while in hospital. “Protest against the situation” refers to statements indicating that teenagers in particular were refusing food as a protest against the situation of being ill and the feeling of being confined to the ward.
Altered choice of food
Children
Most of the children said that their choice of food changed after initiation of chemotherapy. The subcategory preferred foods was formed. Examples of preferred foods were pancakes, pasta, potato dishes, taco shells, rice and salty snacks like potato strips and popcorn. A few children also liked fried chicken, hot dogs and fried fish. Follow-up questions showed an initial satisfaction with the regular hospital food and the dishes composed upon request by the central kitchen. The older children said that they wanted their parents to purvey food for them. Thus, purveyed food was generally better tolerated than hospital food.
Parents
The parents related that the child’s food preferences generally became limited and that the child alternated between a few food items after initiation of chemotherapy. The parents perceived the altered food preferences as related to taste preferences. The parents of three children said that the child wanted salty foods most of all. The parents of three other children said that spicy and sour foods such as tomato soup, pickles and olives were preferred. Eighty-five percent of the parents said that they purveyed food for their child. They bought ingredients and cooked for the child and/or bought food to be consumed by the child on the ward. The parents of five children stated that they paid no attention to whether the food they purveyed was nutritious. Being flexible and providing food the child asked for was of greater importance. The mother of a 12-year-old boy described her ambition to purvey food that was acceptable to her child:
When he ate, it was mostly junk food. He could suddenly ask for a certain brand of French fries. It was during that time we learned where to find the fast-food stands that were open at night. His food preferences became very different. I paid no attention to whether the food was nutritious.
Nurses
A majority of the nurses said that most of the food the child actually consumed was purveyed by the parents. Three nurses believed that providing food was a crucial parental task and an important part of their coping strategy. It relieved anxiety and was also a way for the family to maintain some autonomy on the ward.
Parents may feel powerless on the ward, because the possibility for them to have any influence is so limited. By being busy with the child’s food, they may experience some autonomy.
Several food items became less well tolerated after initiation of chemotherapy. Therefore the subcategory disliked/avoided foods was formed.
Disliked/avoided foods
Children
Disliked/avoided foods were red meat, hot dogs and chicken, which were avoided by eight children (38%). Sweets were avoided by six children (29%), and chocolates were avoided by two. The avoided food items were perceived as having a strange taste or were associated with nausea that had been experienced close to the time chemotherapy was administered.
The older children, aged 8–17 years, were generally negative towards the regular hospital food. Seven children (33%) criticized how the food was prepared and the selection of dishes. The food was perceived as “disgusting”. Furthermore, four children in this age group said that they only drank water while in hospital. They avoided all kinds of food, including food purveyed by the parents and meals and snacks prepared by the nurses on the ward, because it was perceived as disgusting. One 17-year-old boy said:
I find everything on the ward disgusting. I never eat when I’m here. I hardly ever drink water.
According to the routines on the ward, oral nutrition support was offered by means of enriching selected dishes with cream and butter and beverages with glucose polymeres. In addition, commercial energy-dense drinks were available in a variety of flavours.
Six children, aged 8–17 years, said that commercial energy-dense drinks were provided during periods of poor eating. However, these drinks were generally not well accepted by the children. A 15-year-old boy described his perception of these drinks:
They offered me a lot of them. I did not want them. They tasted strong, like acid. Even if you try one with chocolate flavour, the taste is still disgusting.
Only one 17-year-old boy said that he agreed to consume these drinks, but this was only because he thereby avoided nasogastric tube feeding.
Parents
The parents of 11 children (52%) expressed a negative view of the hospital food. These criticisms concerned how the food was prepared, which food items were available and the lack of flexibility with respect to the shifting needs of the child. Parents of older children indicated that any food or beverage served on the ward became aversive. The mother of a 12-year-old boy said that her child’s rejection of a brand-named previously accepted beverage was based on the idea that the beverage was “contaminated” when it was served on the ward. The same beverage, when bought outside the hospital, was accepted by the child.
The parents of ten children said that commercial energy drinks were offered during periods of poor eating. All but one said that they were not accepted by the child. Instead, the parents of four children enriched dishes with butter and cream and beverages with tasteless and odourless glucose polymeres as prescribed by the dietician. The mother of a 3-year-old child described her own strategy:
The dietician told me about the energy drinks. But my child didn’t like them. Instead I made a mixture of milk, cream and cocoa. Then I add enrichment powder. In this way I can hide its taste.
Nurses
The statements made by nine (45%) nurses indicated that especially the older children generally avoided the regular hospital food. It was the nurses’ perception that by rejecting the hospital food, the child may want to manifest his/her autonomy.
Nine nurses said that commercial energy drinks were suggested as the first choice for nutrition support during periods of poor food intake. Most of them emphasised the importance of how the drink was presented to the child. Acceptance would be better if it was served in an attractive way, thereby avoiding the association with “medicine” or “hospital food”, and one of the nurses reported:
The drinks would be better accepted if they were served in a fancy way, for example in a nice glass.
Taste acuity test
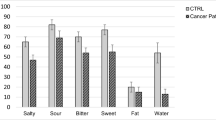
There was a significant difference (Mann–Whitney, p<0.05) in recognition thresholds for bitter taste between the groups, where the patients were less sensitive compared to controls, median (range) 0.015 mmol/l (0.002–0.06) and 0.004 mmol/l (0.002–0.06), respectively. There were no significant differences in recognition thresholds for salt, although the median (range) recognition threshold for salt was 62.5 mmol/l (7.8–250) for the patient group and 15.6 mmol/l (3.9–125) for the control group. No significant differences between the groups were found in recognition thresholds for sweet or sour, where both median and range were the same between the groups: 22.0 mmol/l (15.6–62.5) for sweet and 0.24 mmol/l (0.03–1.95) for sour.
Interestingly, the taste acuity test also showed that significantly more patients made taste recognition errors, the incorrect identification of a taste, compared to the controls (chi-square, p<0.05). Table 3 shows that the most common taste recognition errors made by the patients were that they reported a bitter taste when another tastant or water was presented. Further analysis, comparing the type of error for type of stimulus between the groups, revealed that the patients incorrectly reported bitter taste at a higher rate compared with the controls (Mann–Whitney, p<0.05), while there were no differences between the groups for the other incorrect reports (sweet, salty, sour and “don’t know”).
Questionnaire
Seventy percent of the patients who filled out the questionnaire reported alterations in taste since the start of chemotherapy. Examples of statements indicating this include “many things taste stronger”, “it has less taste and sometimes no taste”, “meat has a strange taste” and “food tastes bitter”. None of the healthy, age- and sex-matched controls reported any such observations.
Anthropometry
Initially, the median (range) SD for weight in the whole patient group was +0.25 (−1.8–1.8) as judged by the national reference for age and sex [1]. Three months after initiation of chemotherapy, the median (range) SD for the study group was ±0.0 (−1.3–1.4). Although there was an average weight reduction up to 3 months after the initiation of chemotherapy, it was statistically significant only when measured 1 week after the initiation of chemotherapy (Wilcoxon’s signed rank test for paired data, p<0.004). Furthermore, in relation to the reference data, height development was significantly retarded at 3 months after initiation of chemotherapy, −0.03 SD, (range −1.6–1.2), compared with the initial height, +0.20 SD (range −1.3–1.3) (Wilcoxon’s signed rank test for paired data, p<0.001).
Discussion
This study, in examining various aspects of food-related problems after initiation of chemotherapy in children with cancer, tries to identify some of the problems regarding food intake in these children. It should be noted that paediatric cancer is not very common, and the patient group is small and heterogeneous with respect to ages and diagnoses. This may have consequences for the possibility of drawing general conclusions. However, the children in the study are representative of paediatric oncology patients in the region covered by Umeå University Hospital (encounting approximately 10% of the Swedish population).
Based on the interviews, both children and parents perceived that altered taste was the predominant cause of the eating problems in these children. The children also viewed learned food aversions, nausea and pain as important causes, while the parents perceived nausea, pain, food aversions and altered smell as significant factors. The nurses reported nausea, feeling ill and the negative effect of the ward environment as important causes of the eating problems. The nurses also judged food refusal as a protest and a way for the child to gain some control over the situation. These discrepancies between the children and their parents on one side, and the nurses on the other, indicate that the nurses may focus on more easily managed causes and underestimate perceived altered taste sensation. Altered taste perception is not a life threatening side effect of cancer treatment and may therefore be overlooked by caregivers.
The taste test showed that the children with cancer under chemotherapy had higher recognition thresholds for bitter and that they made more recognition errors than the controls. None of the patients actually complained of any bitter background taste, although they, in several cases, answered “bitter” when they were presented with very low concentrations of sweet, salty and sour solutions as well as for the blank (water). Even if these findings do not account for all of the abnormal taste of food and changes in food preferences reported by the children, they do indicate the existence of some physiological taste dysfunction. This latter aspect is also supported by the analysis of the questionnaires. The physiological dysfunction seems to be especially related to the perception of bitterness and raises the question of whether there is a phantom taste, a distortion where a taste is perceived but there is no stimulation [16], of bitterness present in many of the patients. Theoretically, if that is the case, this phantom taste of bitterness may affect some of these children so that they avoid certain foods and prefer spicy and strong tastes. Furthermore, it cannot be ruled out that the existence of this kind of dysfunction in some cases also can affect taste thresholds, since the participant has to detect other stimuli with a phantom taste present.
Very few taste acuity tests have been performed in children undergoing chemotherapy, and the results that have been published are not totally in agreement. In children with leukaemia, Wall and Gabriel [36] reported significantly higher recognition thresholds for all four tastes, while Barale and co-workers [2] found that the threshold for salt recognition was significantly increased. The discrepancy between the results of the present study and these previous studies are, at least to some extent, probably a consequence of heterogeneity with respect to diagnoses and timing of the taste acuity test in relation to initiation of chemotherapy. However, the results suggest that providing a variety of “tasty” food in the hospital setting to improve food intake does not suffice for many paediatric cancer patients because they also suffer from altered taste sensations. There are probably various mechanisms behind taste alteration in cancer patients. One interesting hypothesis by Berteretche and co-workers [6], who studied taste sensitivity in adult cancer patients, describes how some of these changes related to chemotherapy may develop. During chemotherapy, the renewal of taste cells is considerably decreased, which, in turn, can affect taste sensitivity. At the end of the treatment, a significantly larger number of taste cells are synchronously renewed and have to make new contacts with taste nerve fibres. If this mapping between taste cells and nerve fibres is disturbed in some way, it may change the coding of taste.
As a group, the children were not underweight on admission. However, there was an average weight loss up to 3 months after initiation of chemotherapy as well as a retarded height development, indicating that the energy requirements were not achieved in many of these children. The small number of participants in each diagnosis group did not allow for subgroup analysis regarding, for example, weight development in relation to corticosteroid dosage.
Learned food aversions were commonly reported in the interviews, and aversive food included, for example, red meat, ice cream and chocolate. Protein rich food and food with a strong flavour, such as chocolate, easily become targets for aversions [5]. This is unfortunate because red meat, for example, is energy-dense food and is also nutritionally significant in terms of protein and iron intake. In the present study, children, parents and nurses reported that nausea strongly contributed to the eating problems. The prevention of nausea is important in paediatric cancer treatment, because nausea plays a potent role in the development of learned food aversions [4, 27]. Although 5-HT3-receptor antagonists were given in scheduled doses in association with chemotherapy administration, complete control of symptoms was obviously not achieved in all patients. The efficacy of anti-emetics is influenced by patient characteristics such as sex, age, prior history of motion sickness, high anxiety levels and poorly controlled nausea in previous chemotherapy cycles [31]. This may explain why paediatric cancer patients continue to suffer from chemotherapy-induced nausea in spite of powerful anti-emetics [17]. Hopefully, more effective and individually tailored medical treatment for managing nausea and vomiting will be able to reduce these problems in the future.
The older children were generally more negative than the younger children towards the regular hospital food. The children criticized its taste, preparation and lack of variation. It was rejected in favour of foods purveyed by the parents. Furthermore, some of the older children refused food, since they found all foods served on the ward disgusting. Disgust has a strong affective component, indicating that there are objections to sensory characteristics related to the taste, smell, texture or appearance of the food [14]. In the interview, some nurses believed that another reason for rejecting the hospital food was that the child wanted to express autonomy and gain some control over the situation. Food carries a social and cultural meaning and is of significance regarding individual identity [15], and life in hospital causes patients to lose control and their autonomy becomes subordinated to hospital routines [18]. When loss of control occurs, the child may strive to maintain control in any way possible. Rejection of hospital food can serve as a demonstration of such control. Food purveyed by the parents may represent the identity of the child, the family and life outside the hospital and may therefore be better accepted.
Although the hospital menu provided well-known dishes, food neophobia may play an important role for the reported food rejection in this study. Neophobia is a known manifestation in the avoidance of unfamiliar food [7]. Food does not even have to be a new product to be perceived as unfamiliar. For example, a new brand of a previously well-known food can be perceived as unfamiliar [23]. This, as well as changed taste perception may contribute to making hospital food both more unfamiliar and aversive. Another important aspect related to problems with food is that when eating pattern change for a child with cancer, parents have been reported to feel helpless and to have become preoccupied with their child’s eating [11, 19, 22]. Parents also experience high levels of anxiety, depression, loneliness and physical and psychological distress [8]. Furthermore, paediatric cancer patients have been reported to be coaxed more by their parents during mealtimes compared to healthy children [36]. Coercion can sometimes decrease food intake [7]. It is therefore possible that in some cases, the parents, who are anxious to increase the child’s food intake, unintentionally exacerbate the eating problems.
All variables discussed above are probably contributing factors in the frequent avoidance of, for example, the commercial liquid supplements served on the ward. It can also be concluded that energy enrichment, especially by means of hospital food, does not always make sufficient nutritional contributions to a child on chemotherapy with food-related problems. It should be noted that several other factors may as well affect food-related behaviour and food intake in paediatric cancer patients. Changed social circumstances, depression, and loneliness all have an impact on the food intake of the individual [13]. In conclusion, the present study shows that the requirements for energy and nutrients are difficult to meet by food intake for many children undergoing chemotherapy for malignant disease, and at least part of the explanation is that there are changes both in the primary gustatory sense as well as in the perception of food and eating behaviour in these children.
Implications for nursing
The nurse plays a vital role in the daily assessment of the child’s nutritional status and can, in close collaboration with the parents, identify factors that interfere with the child’s food intake. Nutritional screening should include a history of decreased or unusual food intake, an estimation of energy intake in relation to calculated needs and expected weight and height development. Nausea plays a potent role in the development of food aversions. Without effective prophylaxis, nausea and vomiting and, consequently, learned food aversions become debilitating and impair the quality of life of the patient. To cope more successfully to the situation, parents should be informed early in the treatment about common problems that interfere with food intake, such as alteration in taste and learned food aversions. The child’s individual food preferences and aversions should be considered, and combinations of oral, enteral and parenteral nutrition support should be used. Spicy foods may be served when appropriate, since spices may mask possible phantom taste. Elimination of odours that adversely affect appetite in smell-sensitive patients should be taken into account in food preparation and presentation. The overall goals of nutritional care are to prevent and correct nutritional deficiencies and to minimize weight loss to the benefit of treatment success.
References
Albertsson Wikland K, Luo ZC, Niklasson A, Karlberg J (2002) Swedish population-based longitudinal reference values from birth to 18 years of age for height, weight and head circumference. Acta Paediatr 91:739–754
Barale K, Aker SN, Martinsen CS (1982) Primary taste thresholds in children with leukemia undergoing marrow transplantation. J Parenter Enteral Nutr 6:287–290
Berde CB, Billett AL, Collins JJ (2002) Symptom management in supportive care. In: Pizzo PA, Poplack DG (eds) Principles and practice of pediatric oncology. Lippincott Williams & Wilkins, Philadelphia, pp 1302–1332
Bernstein IL (1978) Learned taste aversions in children receiving chemotherapy. Science 200:1302–1303
Bernstein IL (1999) Taste aversion learning: a contemporary perspective. Nutrition 15:229–234
Berteretche MV, Dalix AM, dÓrnano AM, Bellisle F, Khayat D, Faurion A (2004) Decreased taste sensitivity in cancer patients under chemotherapy. Support Care Cancer 12:571–576
Birch LL (1999) Development of food preferences. Annu Rev Nutr 19:41–62
Boman KK, Viksten J, Kogner P, Samuelsson U (2004) Serious illness in childhood: the different threats of cancer and diabetes from a parent perspective. J Pediatr 145:373–379
Comeau TB, Epstein JB, Migas C (2001) Taste and smell dysfunction in patients receiving chemotherapy: a review of current knowledge. Support Care Cancer 9:575–580
Cornsweet TN (1962) The staircase-method in psychophysics. Am J Psychol 75:485–591
Davies CM, Noll RB, Davies WH, Bukowski WM (1993) Mealtime interactions and family relationships of families with children who have cancer in long-term remission and controls. J Am Diet Assoc 93:773–776
Delbecque-Boussard L, Gottrand F, Ategbo S, Nelken B, Mazingue F, Vic P, Farriaux JP, Turck D (1997) Nutritional status of children with acute lymphoblastic leukemia: a longitudinal study. Am J Clin Nutr 65:95–100
Drewnowski A (1997) Taste preferences and food intake. Annu Rev Nutr 17:237–253
Fallon AE, Rozin P, Pliner P (1984) The child’s conception of food: the development of food rejections with special reference to disgust and contamination sensitivity. Child Dev 55:566–575
Fischler C (1988) Food, self and identity. Soc Sci Inform 27:275–293
Hawkes CH (2002) Smell and taste complaints. Butterworth Heinemann, Amsterdam, pp 123–179
Hockenberry M (2004) Symptom management research in children with cancer. J Pediatr Oncol Nurs 21:132–136
Holm L, Smidt S (1997) Uncovering social structures and status differences in health systems. Eur J Public Health 7:373–378
Holm L, Smidt S, Michaelsen KF (1996) Socio-psychological significance of hospital meals—the impact of the introduction of a new catering system in a children’s cancer ward. Scand J Nutr 40:6–10
Kennedy DD, Tucker KL, Ladas ED, Rheingold SR, Blumberg J, Kelly KM (2004) Low antioxidant vitamin intakes are associated with increases in adverse effects of chemotherapy in children with acute lymphoblastic leukaemia. Am J Clin Nutr 79:1029–1036
Krippendorf K (1980) Content analysis. An introduction to its methodology. Sage Publications, Beverly Hills
Kvist SB, Rajantie J, Kvist M, Siimes MA (1991) Perceptions of problematic events and quality of care among patients and parents after successful therapy of the child’s malignant disease. Soc Sci Med 33:249–256
Lee K (1989) Food neophobia: major causes and treatments. Food Technol 43:62–73
Murry DJ, Riva L, Poplack DG (1998) Impact of nutrition on pharmacokinetics of anti-neoplastic agents. Int J Cancer 11:48–51
Nilsson H, Holm AK (1983) Taste thresholds, taste preferences and dental caries in 15-year-olds. J Dent Res 62:1069–1072
Nordic Society of Pediatric Haematology and Oncology (NOPHO) (2004) Childhood cancer in the Nordic countries. Report on epidemiologic and therapeutic results from registries and working groups. NOPHO Annual Meeting, Odense
Pelchat ML, Rozin P (1982) The special role of nausea in the acquisition of food dislikes by humans. Appetite 3:341–351
Reilly JJ, Brougham M, Montgomery C, Richardson F, Kelly A, Gibson BE (2001) Effect of glucocorticoid treatment on energy intake in children treated for acute lymphoblastic leukemia. J Clin Endocrinol Metab 86:3742–3745
Sala A, Pencharz P, Barr RD (2004) Children, cancer and nutrition—a dynamic triangle in review. Cancer 100:677–687
Schiffman SS (1997) Taste and smell losses in normal aging and disease. JAMA 278:1357–1362
Schnell FM (2003) Chemotherapy-induced nausea and vomiting: the importance of acute antiemetic control. Oncologist 8:187–198
Scrimshaw NS (2003) Historical concepts of interactions, synergism and antagonisms between nutrition and infection. J Nutr 133:316–321
Skolin I, Axelsson K, Ghannad P, Hernell O, Wahlin YB (1997) Nutrient intake and weight development in children during chemotherapy for malignant disease. Oral Oncol 33:364–368
Skolin I, Hernell O, Wahlin YB (2001) Energy and nutrient intake and nutritional status of children with malignant disease during chemotherapy after the introduction of new mealtime routines. Scand J Caring Sci 15:82–91
Skolin I, Hursti UK, Wahlin YB (2001) Parents’ perception of their child’s food intake after the start of chemotherapy. J Pediatr Oncol Nurs 18:124–136
Wall DT, Gabriel LA (1983) Alteration of taste in children with leukemia. Cancer Nurs 6:447–452
Williams R, Virtue K, Adkins A (1998) Room service improves patient food intake and satisfaction with hospital food. J Pediatr Oncol Nurs 15:183–189
Acknowledgements
This study was financed by the Children’s Cancer Foundation in Sweden and by the Gunnar Nilsson Cancer Foundation. The authors wish to thank the patients, parents and staff at the Paediatric Haematology and Oncology Unit at Umeå University Hospital. Special thanks to Siv Inger Eliasson for the medical records’ review, Margareta Holmgren for carrying out the taste acuity tests and Lena Carling for providing the software program for the anthropometry analysis. We are indebted to Dr. Gregory Neely and Gareth Morgan for valuable comments on the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Skolin, I., Wahlin, Y.B., Broman, D.A. et al. Altered food intake and taste perception in children with cancer after start of chemotherapy: perspectives of children, parents and nurses. Support Care Cancer 14, 369–378 (2006). https://doi.org/10.1007/s00520-005-0904-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-005-0904-6