Abstract
Background
The psychological difficulty of accepting a mastectomy for locally advanced breast cancer (LABC) justifies the use of chemotherapy as neoadjuvant primary treatment. The aim of this prospective study was to assess the efficacy of the doxorubicin/paclitaxel (AT) schedule neoadjuvantly administered in terms of response rates and survival in patients with LABC, with a special focus on cardiac toxicity.
Patients and method
All patients were treated by doxorubicin (60 mg/m2 i.v.) bolus followed by paclitaxel (200 mg/m2) as a 3-h infusion. Treatment was repeated every 3 weeks for four or six courses and followed by surgery, radiotherapy, and hormonotherapy for patients with positive hormonal receptors. Patients with significant cardiovascular history or ECG abnormalities were not eligible for the study. Measurements of left ventricular ejection fraction (LVEF) were performed at baseline and at the end of chemotherapy.
Results
From 1998 to 2001, 34 consecutive patients followed up in our institution were entered into this study. Median age was 49 years (range, 32–68 years). Seventeen patients had stage IIB, 5 patients stage IIIA, and 12 patients stage IIIB disease. Twenty-one patients underwent conservative surgery, 7 radical surgery, and 6 patients no surgery due to metastatic disease occurring during treatment. An objective clinical response was noted in 22 (65%) of 34 patients (6 patients with histological complete response, 10 patients with rare malignant cells, and 6 patients with a partial response), 6 patients presented a progressive disease, and 8 patients a stable disease. Twenty-four patients have kept normal cardiac function, 7 patients had a cardiac toxicity as defined by the institution [4 (24%) of 17 patients received 360 mg/m2 of doxorubicin (A), 2 of 4 presented congestive heart failure (CHF), and 3 (21%) of 14 patients received 240 mg/m2 of A without CHF]. Three patients did not receive four or six cycles as initially planned due to the progressive disease during the chemotherapy courses. These patients were excluded from the final analysis, particularly cardiac toxicity analysis. At time of median follow-up (42 months), 28 of 34 patients were alive (one death due to CHF, five others due to progressive disease).
Conclusion
The AT regimen in neoadjuvant treatment for LABC remains efficient, but cardiac toxicity reported in this study underlies the necessity to optimize the schedule of AT combination.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most common cancer affecting women in the USA and Europe, and 8–9% of women will develop breast cancer during their lifetime. Every year more than 250,000 new cases are diagnosed in Europe and approximately 175,000 new cases in the USA, with incidence increasing steadily. Locally advanced breast cancer (LABC) is a heterogenous disease accounting for approximately 10–15% of all newly diagnosed breast cancers [1]. LABC usually comprises a combination of relatively indolent tumors, rapidly growing cancers, and inflammatory breast cancers. Overall, patients with LABC are at higher risk of local recurrence and distant metastases and therefore have a poorer survival outcome. Unlike early primary breast cancer, surgery in the form of either breast conservation or mastectomy is often not a feasible treatment at least initially because of tumor size and involvement of the overlying skin and/or chest wall [2]. Other modalities such as chemotherapy, radiotherapy, and hormone therapy when used alone usually do not result in permanent local control. The management of LABC has evolved over the past few decades to the currently popular multimodal approach with neoadjuvant chemotherapy, surgery, radiotherapy, and adjuvant hormone therapy, all given up front [3, 4]. Although this approach may improve initial local control, each of these modalities has associated morbidity and it is unclear whether all patients with LABC will benefit from initial treatment with a combination of all these therapies, particularly given the heterogeneity of the tumors. The last step in this direction has been to submit patients with otherwise operable cancers to neoadjuvant chemotherapy to increase the proportion of those amenable to breast conservation in order to avoid the psychological difficulty of accepting a mastectomy [5–7]. The application of anthracycline-based neoadjuvant chemotherapy has resulted in response rates ranging from 72 to 97%, clinical complete responses of 12–52%, and pathologic complete responses of 4–33%. The use of anthracycline-based neoadjuvant chemotherapy in the treatment of LABC is thus now firmly established [8]. Research in the treatment of LABC is needed to further define the optimal method of local therapy and the role of new agents such as taxanes. Paclitaxel has well-established single-agent activity in the first-line treatment of women with advanced and metastatic breast cancer, with response rates for standard dose therapy ranging from 25 to 29%. Of note, higher activity has been reported in first-line therapy in combination with doxorubicin, with response rates ranging from 46 to 94%, depending on the administered dose and whether the patient has previously received chemotherapy [9–12], but severe cardiac toxicities were described in 18% of the patients receiving doxorubicin in combination with paclitaxel [13–15].
The aim of this prospective study was to assess for the first time the efficacy of a doxorubicin/paclitaxel (AT) schedule neoadjuvantly administered in terms of response rates and survival in patients with LABC, with special focus and attention on cardiac toxicity due to previous relatively cardiac toxicities described by Gianni et al. [13] 3 years ago before starting this study.
Materials and methods
Patient characteristics
Between August 1998 and January 2001, 34 consecutive patients followed up in our institution were entered into this prospective study. The prestudy evaluation included medical history, physical examination, tumor measurements (by chest X-ray), abdominal ultrasound (or computed tomography scan and bone scan), cardiac function analysis, and other examinations as clinically indicated. All patients had histologically proven breast cancer, primary operable breast cancer (stage IIB, IIIA, and IIIB), and no metastatic disease. Patients with inflammatory breast cancer could be possibly enrolled in this study. Staging of the primary tumor was performed according to the criteria of the fifth edition of the American Joint Committee on Cancer (AJCC) Staging Manual for breast cancer published in 1997 by Lippincott-Raven. Inclusion criteria were the following: age less than 70 years, World Health Organization (WHO) performance status of 2 or less, adequate hematological, renal, and hepatic functions. No prior chemotherapy or radiotherapy was allowed; all were treatment-naive patients. Patients with significant cardiovascular history or ECG abnormalities were not eligible for the study. Measurements of left ventricular ejection fraction (LVEF) were performed at baseline and at the end of chemotherapy. The criteria to evaluate cardiotoxicity were as follows: more than 20% absolute decrease from baseline even if within normal range (>50%), more than 10% decrease below the lower limit of normal as defined by the institution (<50%), or clinical signs and symptoms of congestive heart failure (CHF) associated with a decrease in LVEF. Patients 50 years old or younger were considered to be premenopausal, and those older were deemed postmenopausal. The histological grade was scored according to previously published classification. Cytosolic estrogen receptors (ERs) and progesterone receptors (PRs) were estimated by cytosolic immunoassay. Positivity or negativity was determined according to the scoring systems used by the individual institution. All patients gave informed consent before entering the trial; this study was approved by the ethic local committee.
Treatment
All patients were treated with doxorubicin (Adriblastine) 60 mg/m2 i.v. bolus (day 1) followed in 30 min by paclitaxel (Taxol) 200 mg/m2 i.v. over 3 h (day 1). Treatment was repeated every 3 weeks for four or six courses and followed by surgery (mastectomy or breast-conserving surgery), radiotherapy, and hormonotherapy. All patients who underwent breast-conserving therapy received irradiation of the whole breast; for patients who had radical total surgery, radiotherapy was performed according to international guidelines. Two tangential photon fields were used for the chest wall or the breast, for a total International Commission on Radiation Units and Measurements (ICRU) dose of 50 Gy. The supraclavicular and internal mammary nodes were treated with a mixed beam (1/3 photons and 2/3 electrons) for a total ICRU dose of 50 Gy. All patients were treated 5 days per week, 2 Gy per fraction, for 5 or 6 weeks. In the case of a conservative treatment, a 12-Gy electron boost was added to the tumoral bed. Patients received tamoxifen 20 mg daily for 5 years regardless of their ER status.
Response to treatment
Tumor assessments were repeated every 6 weeks and at the end of the study. The response to chemotherapy was assessed physically, radiographically, and sonographically. Pathological response rate was evaluated on the intention-to-treat population (those receiving one or more cycles of chemotherapy) and on the evaluable population (those receiving one or more cycles of chemotherapy with surgery after the last cycle). Response was considered complete if there was no evidence of the primary breast tumor by the assessment method. Response was considered complete according to WHO criteria if there was a total disappearance of the tumor. Pathological response was considered complete if there was no evidence of primary breast tumor or carcinoma in situ and nodes were negative. Response was considered partial if there was a reduction of more than 50% in the product of the two largest perpendicular diameters of the tumor. If the tumor area showed a reduction of less than 50% or an increase of less than 25%, no change was considered to have occurred and was considered as stable disease. Progression was defined by an increase of more than 25% in the products of the two largest diameters.
Statistical analysis
Overall survival was computed between the date of diagnosis and the date of the clinical event (recurrence or death) or the date of the last visit for alive patients. Concerning the impact of the administration of AT regimen on pretreatment and posttreatment LVEF values, the paired sample t test was used. Statistical significance was set at p<0.05. Statistical analyses were drawn up on BMDP software (BMDP Statistical Software, Inc., Los Angeles, CA, 1991).
Results
Characteristics of the patients
From August 1998 to September 2001 there were 34 consecutive patients with LABC followed up in our institution who were entered into this study. A description of the population is given in Table 1. Median age was 49 years (range, 32–68 years). Median pretreatment tumor size was 4.5 cm (range, 2.5–8 cm). Clinically positive lymph nodes were noted in 12 patients (35%) (3 N1, 5 N2, and 4 N3), 17 patients had stage IIB, 5 patients stage IIIA, and 12 patients stage IIIB disease (for more details about clinical tumor and lymph node status see Table 2). Estrogen receptors were positive in 19 patients (56%). Ductal invasive carcinoma was present in 30 patients (88%). Twenty-eight patients (82%) had undergone tumor resection with axillary lymph node dissection: 21 patients (62%) underwent conservative surgery (tumorectomy) and 7 patients (21%) radical surgery (mastectomy). A locoregional treatment by radiotherapy associated with surgery was given to 22 patients (65%). Adjuvant chemotherapy was administered to 6 patients (18%) and adjuvant hormonotherapy by tamoxifen was given to 19 patients (56%). Six patients had no surgery due to metastasis disease occurring during treatment.
Cardiac toxicity and compliance to chemotherapy
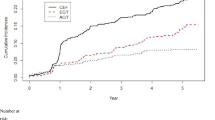
Seventeen patients received six cycles (360 mg/m2) and 14 patients received four cycles (240 mg/m2) of A. Three patients did not receive four or six cycles as initially planned due to progressive disease during the chemotherapy courses. These patients were excluded from the final analysis, particularly cardiac toxicity analysis. LVEF value before treatment ranged from 50 to 75% (mean, 65.5%; median, 64.2%). This range of LVEF distribution, as well as the mean and median values, compares well to population with good performance status. LVEF value after chemotherapy ranged from 40 to 75% (mean, 61.5%; median, 59.2%). LVEF value significantly decreased after AT administration (Fig. 1; paired sample t test, p=0.01); the mean decrease in LVEF value was 11.1%. Twenty-four patients kept normal cardiac function but 7 patients fulfilled the institutional criteria for cardiac toxicity. Three patients had a more than 10% decrease of LVEF below the lower limit of normal as defined by the institution and 4 patients experienced an LVEF reduction of >20% ejection fraction points from baseline.
Table 3 summarizes cardiotoxicities in 31 patients according to clinical and pathological treatment characteristics. Four of 17 patients (24%) received 360 mg/m2 of A; 2 patients presented CHF (one patient died in the intensive care unit due to CHF), whereas 3 (21%) of 14 patients received 240 mg/m2 of A without CHF. Due to the small number of cardiac events, it was impossible to provide any meaningful data.
More importantly, there were no cases of cardiotoxicity during the posttreatment follow-up period, and 6 of the 7 patients restored their initial LVEF. For the other patients we did not observe long-term cardiac disorders. Only one case of cardiac failure was finally observed.
Response and disease control
An objective clinical response was noted in 22 (65%) of 34 patients (16 patients with a histological complete response and 6 patients with a partial response), 5 patients presented a progressive disease, and 7 patients presented a stable disease.
At time of analysis the median follow-up of the study population was 42 months. Three-year survival rates for overall survival was 76%. Twenty-eight of the 34 patients were alive at last follow up (one death due to CHF, five others due to progressive disease). A search to predict responder patients was not performed due to the low number of patients included in the present study.
Discussion
Neoadjuvant chemotherapy is used increasingly in the treatment of primary breast cancer [2]. Doxorubicin, as monotherapy or in combination, is effective and widely used in the treatment of advanced or metastatic breast cancer. The taxanes have also gained prominence as an effective treatment for breast cancer [12, 16]. Whatever the neoadjuvant chemotherapy regimen, this treatment gives high clinical objective response rates (70–98%) and can result in a pathological complete response in a subgroup of patients (3–34%). In addition, this treatment leads to fewer mastectomies compared to primary surgery (13–33% vs 28–40%) while providing an equivalent survival outcome. However, a proportion (2–30%) of patients receiving neoadjuvant treatment will fail to respond to treatment [17–19]. It is important to note that the ability to identify nonresponders early during treatment would enable the use of alternative therapies that would be more beneficial [2]. In the present study, similar results were observed in term of response rates, survival, and conservative breast treatment. Pierga et al. reported in a large French series the major role of clinical response after neoadjuvant treatment as a prognostic factor for survival [19]. Unfortunately, the small series of patients in the present study does not allow us to individualize clinical or biological markers of responsiveness, but high complete response rates (47%) could offer interesting survival results more demonstrative with a longer follow-up. With regard to clinical efficacy, AT regimen in neoadjuvant treatment for LABC remains efficient, and the present study confirms the role already described of this chemotherapy combination in a metastatic disease setting. However, the cumulative dose of doxorubicin that can be given is limited by dose-related cardiotoxicity, and the taxane paclitaxel seems to exacerbate the cardiac toxicity of anthracyclines [20]. Gianni et al. reported the results of the association doxorubicin (60 mg/m2) followed by 15 min of i.v. paclitaxel (125–200 mg/m2). Thirty-five patients with a nonpretreated metastatic breast cancer were included in this study and objective rates of response of 94%, including 41% of complete response, were reported. However, a significant rate of cardiac toxicity was noted: 6 patients (18%) developed CHF after a median cumulative dose of 480 mg/m2 of doxorubicin [13]. Interaction of a pharmacokinetic type exists between the doxorubicin and the paclitaxel and could be partly explained by a mechanism of competition on the level of biliary elimination. Experimental and clinical arguments establish the origin of the inhibition of the p-glycoprotein by cremophor as the basis of the pharmacokinetic interaction between paclitaxel and anthracyclines. The elimination of doxorubicin is slowed by paclitaxel, resulting in prolonged exposure to drug. This could partly explain the increased incidence of cardiac insufficiency to an accumulated dose higher than 380 mg/m2 of doxorubicin [21]. Gianni et al. reported the incidence of cardiac toxicity in 657 patients with metastatic breast cancer treated by a combination of doxorubicin (50–60 mg/m2) and paclitaxel (175–220 mg/m2). The cardiac toxicity rate was 25% when the doxorubicin was managed with a total amount greater than 440 mg/m2, whereas it was lower than 5% when the amount was less than 380 mg/m2 [22]. In order to specify the effect of the interval between administration, a pharmacokinetic study compared the rates of paclitaxel, doxorubicin, and doxorubicinol according to this time interval [23]. In group A the perfusions were separated by 30 min and in group B by 24 h. The peaks of concentration of doxorubicin and doxorubicinol were very significantly increased in group A compared with group B. Moreover, an increase in the area under the curve (AUC) in group A of 30% and 80% for doxorubicin and doxorubicinol, respectively, was observed. In the present study, 21% of patients treated neoadjuvantly by AT regimen developed cardiac toxicity, with a toxic death due to severe irreversible CHF. Doxorubicin recommended dose was not reached and there was no significant correlation observed between doxorubicin dose (240 vs 360 mg/m2). Giordano et al. concluded that when the doxorubicin dose exceeds 360 mg/m2, the combination of bolus doxorubicin and paclitaxel presents an unacceptable cardiac risk. Similarly, in the present study, a cardiac toxicity in 18.3% of patients has been observed but most of them could be explained by the excessive dose of doxorubicin [15].
The study of Amadori et al. on 19 patients showed that a “washout” of 16 h between A and T drugs did not alter the efficacy of treatment with an objective rate of 78% [20]. The principal toxicity observed was neutropenia and the LVEF never decreased below 50% in absolute value. In the same way, in the study of Jassem et al., the interval between the administration of doxorubicin and paclitaxel was 24 h and no cardiac toxicity was reported [10]. It seems reasonable to propose a 24-h interval minimum between the administration of the AT in order to avoid any pharmacokinetic interaction. Maybe in the present study the washout between A and T administration was not sufficient.
Other strategies make it possible to avoid or limit cardiac toxicity, such as use of epirubicine as anthracycline or a cardio-guard like dexrazoxane (currently in controversy) or a liposomal doxorubicin [24–26].
For clinicians prescribing drugs with high potential risks of cardiac toxicity, a need of biological marker could be of real help. In rats, plasma troponin levels have been shown to correlate well with anthracycline dose [27]. However, in humans there are many confounding factors that can increase troponin concentrations, including kidney failure, pulmonary embolism, recent surgery, cholecystitis, and the presence of rheumatoid factor. In addition, a recent analysis of about 170 samples found no significant association between the incidence of anthracycline-induced cardiotoxicity and troponin I levels [28]. Hence, this assay does not appear to offer a promising predictor of drug-induced cardiac damage.
Currently, therefore, there are no assays of suitable sensitivity and specificity for diagnosing clinically relevant levels of chemotherapy-induced cardiotoxicity [29]. A new approach based on gene expression data specially dedicated to prediction of future cardiac damage derived from DNA microarray analysis could offer a particular efficacy tool for clinicians [30].
To conclude, AT regimen in neoadjuvant treatment for locally advanced primary breast cancer remains efficient, but cardiac toxicity reported in this study underlies the necessity to optimize the schedule of AT combination in the future and to define an algorithm to avoid cardiac problems before the beginning of treatment based on clinical and biological parameters [31].
References
Botha JL, Bray F, Sankila R, Parkin DM (2003) Breast cancer incidence and mortality trends in 16 European countries. Eur J Cancer 39:1718–1729
Smith IC, Miller ID (2001) Issues involved in research into the neoadjuvant treatment of breast cancer. Anti-cancer Drugs 12:25–29
Jones AL, Smith IE, O’Brien ME et al (1994) Phase II study of continuous infusion fluorouracil with epirubicin and cisplatin in patients with metastatic and locally advanced breast cancer: an active new regimen. J Clin Oncol 12:1259–1265
Powles TJ, Hickish TF, Makris A et al (1995) Randomized trial of chemoendocrine therapy started before or after surgery for treatment of primary breast cancer. J Clin Oncol 13:547–552
Kaufmann M, von Minckwitz G, Smith R et al (2003) International expert panel on the use of primary (preoperative) systemic treatment of operable breast cancer: review and recommendations. J Clin Oncol 21:2600–2608
Bonadonna G, Valagussa P, Brambilla C et al (1998) Primary chemotherapy in operable breast cancer: eight-year experience at the Milan Cancer Institute. J Clin Oncol 16:93–100
Fisher B, Bryant J, Wolmark N et al (1998) Effect of preoperative chemotherapy on the outcome of women with operable breast cancer. J Clin Oncol 16:2672–2685
Wolmark N, Wang J, Mamounas E, Bryant J, Fisher B (2001) Preoperative chemotherapy in patients with operable breast cancer: nine-year results from National Surgical Adjuvant Breast and Bowel Project B-18. J Natl Cancer Inst Monographs 30:96–102
Dombernowsky P, Gehl J, Boesgaard M et al (1996) Doxorubicin and paclitaxel, a highly active combination in the treatment of metastatic breast cancer. Semin Oncol 23:23–27
Jassem J, Pienkowski T, Pluzanska A et al (2001) Doxorubicin and paclitaxel versus fluorouracil, doxorubicin, and cyclophosphamide as first-line therapy for women with metastatic breast cancer: final results of a randomized phase III multicenter trial. J Clin Oncol 19:1707–1715
Mamounas EP, Sledge GW Jr (2001) Combined anthracycline–taxane regimens in the adjuvant setting. Semin Oncol 28:24–31
Hortobagyi G, Willey J, Rahman Z et al (1997) Prospective assessment of cardiac toxicity during a randomized phase II trial of doxorubicin and paclitaxel in metastatic breast cancer. Semin Oncol 24:S17–S68
Gianni L, Munzone E, Capri G et al (1995) Paclitaxel by 3-hour infusion in combination with bolus doxorubicin in women with untreated metastatic breast cancer. High antitumor efficacy and cardiac effects in a dose-finding and sequence-finding study. J Clin Oncol 13:2688–2699
Martin M, Lluch A, Ojeda B et al (1997) Paclitaxel plus doxorubicin in metastatic breast cancer preliminary analysis cardiotoxicity. Semin Oncol 24:17–26
Giordano SH, Booser DJ, Murray JL et al (2002) A detailed evaluation of cardiac toxicity: a phase II study of doxorubicin and one- or three-hour-infusion paclitaxel in patients with metastatic breast cancer. Clin Cancer Res 8:3360–3368
Nabholtz JMA (2003) Docetaxel–anthracycline combinations in metastatic breast cancer. Breast Cancer Res Treat 79:3–9
Amat S, Bougnoux P, Penault-Llorca F et al (2003) Neoadjuvant docetaxel for operable breast cancer induces a high pathological response and breast-conservation rate. Br J Cancer 88:1339–1345
Ganem G, Tubiana-Hulin M, Fumoleau P et al (2003) Phase II trial combining docetaxel and doxorubicin as neoadjuvant chemotherapy in patients with operable breast cancer. Ann Oncol 14:1623–1628
Pierga JY, Mouret E, Laurence V et al (2003) Prognostic factors for survival after neoadjuvant chemotherapy in operable breast cancer: the role of clinical response. Eur J Cancer 39:1089–1096
Amadori D, Frassinetti GL, Zoli W et al (1996) Phase I/II study of sequential doxorubicin and paclitaxel in the treatment of advanced breast cancer. Semin Oncol 23:16–27
Minotti G, Saponiero A, Licata S et al (2001) Paclitaxel and docetaxel enhance the metabolism of doxorubicin to toxic species in human myocardium. Clin Cancer Res 7:1511–1515
Gianni L, Dombernowsky P, Sledge G et al (2001) Cardiac function following combination therapy with paclitaxel and doxorubicin: an analysis of 657 women with advanced breast cancer. Ann Oncol 12:1067–1073
Gianni L, Bigano L, Locatelli A et al (1997) Human pharmacokinetic characterization and in vitro study of the interaction between doxorubicin and paclitaxel in patients with breast cancer. J Clin Oncol 15:1906–1915
Sparano JA, Winer EP (2001) Liposomal anthracyclines for breast cancer. Semin Oncol 28:32–40
Esposito M, Venturini M, Vannozzi MO et al (1999) Comparative effects of paclitaxel and docetaxel on the metabolism and pharmacokinetics of epirubicin in breast cancer patients. J Clin Oncol 17:1132–1140
Gennari A, Salvadori B, Donati S et al (1999) Cardiotoxicity of epirubicin/paclitaxel-containing regimen: role of cardiac risk factors. J Clin Oncol 17:3596–3602
Herman EH, Zhang J, Lipshultz SE et al (1999) Correlation between serum levels of cardiac troponin-T and the severity of the chronic cardiomyopathy induced by doxorubicin. J Clin Oncol 17:2237–2243
Ferrari E, Talbodec A, Ferrari P et al (1999) Is troponin I of prognostic value in the detection of anthracycline cardiac toxicity? Eur Heart J 83:94
Ciotti R, Ucci G, Belotti G et al (2001) Prospective evaluation of anthracycline-related early cardiac damage: how do we monitor it? J Clin Oncol 19:4269–4270
West M, Blanchette C, Dressman H et al (2001) Predicting the clinical status of human breast cancer by using gene expression profiles. Proc Natl Acad Sci U S A 98:11462–11467
Ferrero JM, Magné N, Foa C, Largillier R, Namer M (2003) Cardiac tolerability of the combination paclitaxel–anthracyclines in the context of the management of cancer of the breast. Bull Cancer 90:219–226
Acknowledgements
Results presented in part during the 2002 meeting of the European Society of Medical Oncology (ESMO). The authors acknowledge Mrs. I. Van Ackere for technical assistance and particularly for the translation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Magné, N., Largillier, R., Marcy, PY. et al. Cardiac toxicity assessment in locally advanced breast cancer treated neoadjuvantly with doxorubicin/paclitaxel regimen. Support Care Cancer 13, 819–825 (2005). https://doi.org/10.1007/s00520-005-0804-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-005-0804-9