Abstract
This was a cross-sectional study to examine the association between anxiety, depression and quality of life and the use of complementary and alternative medicine. Anxiety and depression was measured using the Hospital Anxiety and Depression Scale (HADS), and quality of life was measured using the global quality of life subscale selected from the European Organization for Treatment and Research of Cancer (EORTC) quality of life core questionnaire (QLQ-C30). In all, 177 breast cancer patients were studied, and 32% (n=57) reported that they used or were using complementary medicine. Users and nonusers did not differ significantly in almost all variables studied, with the exception of duration of their diagnosis. The most commonly used complementary medicine was prayer and spiritual healing (n=45, 73.8% of responses). Performing the logistic regression analysis controlling for age, marital status, educational level, knowledge of diagnosis, time since diagnosis, global quality of life, depression, and anxiety scores, the results indicated that the use of complementary medicine among breast cancer patients was associated with sever depression (odds ratio 2.49, 95% CI 1.06–5.89, P 0.04). The other variables studied did not show any significant results. The study findings confirm that the use of complementary medicine is more common among depressed breast cancer patients and might be a marker of greater psychological distress in this group of patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of complementary and alternative medicine is becoming increasingly common among cancer patients, especially breast cancer patients [3]. There is evidence that users of complementary medicine differ in some characteristics from nonusers; for example, reporting greater psychological distress and worse quality of life. Studies have shown that the use of alternative therapies among cancer patients in general and in breast cancer patients in particular was associated with depression, anxiety, fear of recurrence of cancer, and lower mental health [2, 4, 11]. This study sought to compare psychological distress between breast cancer users and nonusers of complementary and alternative medicine.
Material and methods
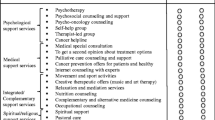
As part of a study on the use of complementary medicine among cancer patients in Iran, a survey of breast cancer patients was conducted to examine the association between anxiety, depression, and overall quality of life and the use of complementary medicine. To indicate the use of complementary and alternative medicine, each patient was asked whether they had ever used or were using complementary and alternative medicine. If the answer was positive, then they were asked to identify therapies they had used or were using. Anxiety and depression was measured using the Iranian version of the Hospital Anxiety and Depression Scale (HADS) [10]. The HADS contains 14 items and consists of two subscales: anxiety and depression. Each item is rated on a four-point scale giving maximum scores of 21 for anxiety and depression. Scores of 11 or more on either subscale are considered to be a significant “case” of psychological morbidity while scores of 8–10 represent “borderline” and 0–7 “normal”. Quality of life was measured using the global quality-of-life subscale selected from the European Organization for Treatment and Research of Cancer (EORTC) quality-of-life questionnaire, the EORTC QLQ-C30 Iranian version [9]. The global quality of life subscale contains two items, and each item is rated on a seven-point scale. A linear transformation was performed to standardize the row scores. Scores ranged from 0 to 100, and the higher values indicated a higher (better) level of global quality of life. To analyze data, descriptive statistics were obtained using the chi-square and t tests. In addition, logistic regression was performed to predict variables that contributed to the use of complementary and alternative medicine.
Results
In all, 177 breast cancer patients were studied, and 32% (n=57) reported that they used or were using complementary medicine. Users and nonusers did not differ significantly in almost all variables studied, with the exception of duration of diagnosis (P 0.007). Characteristics of breast cancer patients as broken down into users and nonusers are shown in Table 1. The most commonly used complementary medicine was prayer and spiritual healing (n=45, 73.8% of responses). The frequency of complementary and alternative therapies used is shown in Table 2. Overall, sever anxiety and depression was reported by 32% and 29% of the patients respectively, and the mean global quality-of-life score was 54.7 (SD 15.7). Performing the logistic regression analysis controlling for age, marital status, educational level, knowledge of diagnosis, time since diagnosis, global quality of life, depression, and anxiety scores, the results indicated that the use of complementary medicine among breast cancer patients was associated with sever depression (odds ratio 2.49, 95% CI 1.06–5.89, P 0.04). The other variables studied did not show any significant results. The results are shown in Table 3.
Discussion
This study did not intend to evaluate the efficacy and safety of the complementary and alternative medicine but to report the present situation in Iran and to investigate the relationship between patients’ psychological status and the use of complementary medicine. Although it is anticipated that in the future there would be a closer and more positive relationship between mainstream cancer care and nonconventional therapies [7], it is argued that the label “unproven” is inappropriate for such therapies, and it is time to assert that many alternative cancer therapies have been “disproven” [15].
The study findings indicated that prayer and spiritual healing was the most commonly used method of complementary therapies, and the other methods were used rarely. Considering the Iranian culture, one should make a distinction between spiritual healing and prayer as it relates to complementary/alternative therapies, and spiritual practice and prayer that relate to one’s religious duties. Based on one’s wishes, the former could take several formal or informal practices whereas the latter can be defined as compulsory religious duties that one should practice every day or at special times. Another explanation for such observation might relate to cost consideration where other methods of alternative therapies could be regarded as expensive whereas patients do not have to pay for spiritual healing and prayer. To our knowledge, some forms of spiritual healing or prayer, such as going to shrines, is very expensive and thus this could not be the case. However, one might argue this is a true reflection of the patients’ culture where prayer and spiritual believes are part of people’s everyday life.
Thus it is possible to say that, unlike in Western countries, the use of common complementary therapies among Iranian breast cancer patients was rare. Most studies from Western countries have reported that a large proportion of breast cancer patients use at least one complementary and alternative therapy. e.g., [1]. Thus, as suggested, it is important that physicians and others involved in cancer patient care and management are informed and educated about complementary and alternative therapies and their use among their cancer patients [13].
Our study findings showed that with regard to the most variables studied, there were no significant differences between users and nonusers of complementary methods. Studies have shown that age and education are associated with the use of complementary medicine [6, 8]. However, after performing logistic regression, only depression was identified as a significant predicting factor. With regard to statistical significance for depression in multivariate analysis but not in bivariate analysis, one might argue that even in bivariate analysis (Table 1), the results indicated that users showed a higher proportion of probable cases of sever depression (39% for users versus 25% for nonusers). This is very similar to the findings from other studies on the topic, indicating that depressed breast cancer patients are more likely to use complementary medicine as compared to patients with normal psychological status [5]. Evidence suggests that users of alternative therapies receive less hope of cure from their physicians or show passive coping behavior [12, 14] and thus the use of complementary medicine among breast cancer patients associated with mental distress and depression [2, 11].
In conclusion, considering the study limitations, the results from this descriptive investigation suggest that the use of complementary and alternative medicine among Iranian breast cancer patients is unpopular. However, the study findings confirm that the use of complementary medicine is more common among depressed breast cancer patients and might be a marker of greater psychological distress in this group of patients.
References
Ashikaga T, Bosompra K, O’Brien P, Nelson L (2002) Use of complimentary and alternative medicine by breast cancer patients: prevalence, patterns and communication with physicians. Support Care Cancer 10:542–548
Burstien HJ, Gelber S, Gundagnoil E, Weeks JC (1999) Use of alternative medicine by women with early-stage breast cancer. N Engl J Med 340:1733–1739
Cassileth BR, Schraub S, Robinson E, Vickers A (2001) Alternative medicine use worldwide. Cancer 91:1390–1393
Correa-Velez I, Clavarino A, Barnett AG, Eastwood H (2003) Use of complementary and alternative medicine and quality of life: changes at the end of life. Palliative Med 17:695–703
DiGianni LM, Garber E, Winer EP (2002) Complementary and alternative medicine use among women with breast cancer. J Clin Oncol 20 [Suppl 18]: 34s-38 s
Henderson JW, Donatelle RJ (2004) Complementary and alternative medicine use by women after allopathic treatment for breast cancer. Altern Ther Health Med 10:52–57
Kolstad A, Risberg T, Bremnes Y, et al (2004) Use of complementary and alternative therapies: a national multicentre study of oncology health professionals in Norway. Support Care Cancer 12:312–318
Lengacher CA, Bennett MP, Kip KE, Keller R, LaVance MS, Smith LS, Cox CE (2002) Frequency of use of complementary and alternative medicine in women with breast cancer. Oncol Nurs Forum 29:1445–1452
Montazeri A, Harirchi I, Vahdani M, Khaleghi F, Jarvandi S, Ebrahimi M, Haji-Mahmoodi M (1999) The EORTC Quality of Life Questionnaire: translation and validation study of the Iranian version. Support Care Cancer 7:400–406
Montazeri A, Vahdaninia M, Ebrahimi M, Jarvandi S (2003) The Hospital Anxiety and Depression Scale (HADS): translation and validation study of the Iranian version. Health and Quality of Life Outcomes 1:14 [http://www.hqlo.com/content/1/1/14]
Risberg T, Jacobsen BK (2003) The association between mental distress and the use of alternative medicine among cancer patients in North Norway. Qual Life Res 12:539–544
Risberg T, Kaasa S, Wist E, Melsom H (1997) Why are cancer patients using non-proven complementary therapies? Eur J Cancer 33:575–580
Sibbritt D, Adams J, Easthope G, Young A (2003) Complementary and alternative medicine (CAM) use among elderly Australian women who have cancer. Support Care Cancer 11:548–550
Sollner W, Maislinger S, DeVries A, Steixner E, Rumpold G, Lukas P (2000) Use of complementary and alternative medicine by cancer patients is not associated with perceived distress or poor compliance with standard treatment but with active coping behavior: a survey. Cancer 89:873–888
Vickers A (2004) Alternative cancer cures: ‘unproven’ or ‘disproven’. CA Cancer J Clin 54:110–118
Author information
Authors and Affiliations
Corresponding author
Additional information
The preliminary results of this study was presented at the 4th European Breast Cancer Conference, Hamburg, Germany, 16–20 March 2004
Rights and permissions
About this article
Cite this article
Montazeri, A., Sajadian, A., Ebrahimi, M. et al. Depression and the use of complementary medicine among breast cancer patients. Support Care Cancer 13, 339–342 (2005). https://doi.org/10.1007/s00520-004-0709-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-004-0709-z