Abstract
A significant proportion of cancer patients experience psychiatric morbidity. Potential predictors of psychiatric morbidity include patient disease-related factors and factors relating to the patient’s environment. The aim of this study was to investigate the prevalence of psychiatric morbidity and the relationship between the clinical or personal factors, especially psychiatric morbidity, and awareness of cancer diagnosis among a group of Turkish cancer patients. A total of 117 cancer patients were assessed using the Structured Clinical Interview for DSM-IV (SCID), the Hospital and Anxiety Depression Scale (HADS) and the General Health Questionnaire (GHQ). Of these patients, 30% had a psychiatric diagnosis. Adjustment disorders comprised most of the psychiatric diagnoses. Awareness of the diagnosis of cancer, history of previous psychiatric disorders, pain and stress factors were correlated with psychiatric morbidity. Of the 117 patients, 64 (54.7%) were unaware of the diagnosis of cancer. Most of the patients (67.9%) who were considered to be aware of the cancer diagnosis stated that they had guessed their illness from the treatment process or drug adverse effects. Psychiatric morbidity was significantly higher in the patients who knew that they had a cancer diagnosis (P=0.03). These findings suggest that the awareness of cancer diagnosis is related to the presence of psychiatric morbidity. In particular, the understanding of the diagnosis indirectly may be stressful to the patient because it arouses suspicion about the cancer and treatment, and consequently can lead to psychiatric disturbance. In Turkey honest disclosure of the true diagnosis is still not common for cancer patients and it seems to be essential to improve this situation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Previous studies have demonstrated an increased risk for psychiatric morbidity among cancer patients [1, 24]. Because of the frightening and potentially stigmatizing nature of the disease, those with cancer may experience emotional and psychological distress. Physicians should be aware of the type of patient likely to experience difficulties, to allow them to detect and treat problems earlier or refer the patient to a psychiatrist more appropriately. Untreated psychiatric disorder in the presence of comorbid conditions may result in more frequent clinic visits, increased costs, extended hospitalization and reduced compliance and quality of life [5, 44]. Failure to evaluate comorbid psychiatric disorder may lead to serious consequences, such as suffering, hopelessness, suicidal thoughts and decreased treatment compliance [9, 22, 40].
Potential predictors of psychiatric morbidity include patient-related factors, disease- and treatment-related variables such as pain and other physical symptoms, being aware of the diagnosis of cancer, and factors related to the patient’s environment such as social support [33, 36]. According to a study from India, psychiatric morbidity is significantly lower in patients who are “unaware” of the diagnosis of cancer and who have a more hopeful outlook on the outcome of treatment [2]. On the contrary, in a study by Hosaka et al. in Japan [28], the prevalence rate of psychiatric disorders was 42.9% in the informed group and 48.3% in the uninformed group, suggesting that concealing the true diagnosis is not related to the presence of psychiatric disorder in Japanese cancer patients. On the other hand, some studies have shown that the possible cost of poor communication with cancer patients include increased anxiety, distress, coping difficulties, and noncompliance with treatment [21, 35]. A study performed in Turkey, which is both an Asian and a European country, has shown a low awareness (44%) of the diagnosis of cancer. However, the relationship between awareness and psychiatric morbidity was not investigated in that study [10].
We conducted this study in an attempt to evaluate the psychiatric morbidity in Turkish cancer patients, and the factors that may be related to psychiatric disorder and how the awareness of a cancer diagnosis influences the psychiatric morbidity in these patients.
Patients and methods
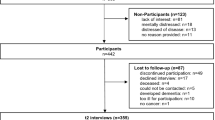
The subjects in the present study were cancer patients who had undergone chemotherapy in different departments (gynaecology and obstetrics, general surgery, internal medicine and oncology) at the Medical School of Pamukkale University Hospital. Admitted to the units between September 2000 and May 2002 were 131 patients. The patients were informed that the aims of study were to determine the prevalence of psychiatric morbidity and to assess their awareness of the illness from which they were suffering. Although an effort was made to recruit a consecutive series of cancer patients admitted to the units, three patients refused to participate, and 11 patients with terminal illness, impaired cognitive function or illiteracy were excluded. Thus, 117 patients participated in the study. Sociodemographic data were obtained from medical records.
The Hospital Anxiety and Depression Scale (HADS) and the 12-item General Health Questionnaire (GHQ-12) were administered by a specially trained nurse. On the same day, each patient’s psychiatric status was evaluated in a detailed psychiatric interview by a psychiatrist who did not know the scores on the two scales. A psychiatric diagnosis was made according to the criteria of DSM-IV with the SCID-I form. Also, the patients’ awareness of the diagnosis of cancer, psychosocial stressors and cancer-related pain were determined during the same interview. Patients’ awareness of the diagnosis of cancer was determined after detailed questioning. Patients were asked tactfully about the nature of their illness and the reasons for hospital admission.
The following questions were asked: “What do you think you are suffering from?” and “Why do you think you are in hospital?”. Based on the responses to these questions a decision regarding awareness or nonawareness of disease diagnosis was made by a psychiatrist. Psychosocial stressors were classified according to life events using the DSM-IV multiaxial diagnostic system. In evaluating the stress factors, a period of 1 year before the interview was taken into consideration. However, psychosocial stressors that had clearly contributed to the development of the psychiatric disorder but happened earlier were also accepted as stress factors [3]. The presence or absence of cancer-related pain was assessed by patient self-reporting.
Instruments
General Health Questionnaire
The GHQ was designed to give a general indication of a possible psychiatric case rather than being indicative of a specific diagnosis. The original 60-item version is rather lengthy; therefore shorter versions are commonly used. The 12-item form of the GHQ was used in our study population. For the GHQ-12, Likert-type scoring (0, 1, 2, 3) is used. Kılıç [29] performed validity and reliability studies of the Turkish version of GHQ-12, and the cut-off score was accepted as 10/11.
The Hospital Anxiety and Depression Scale
The HADS was developed to rate anxiety and depression in patients with physical illness, and consists of two subscales, one assessing anxiety and one depression. Each item is rated on a scale of 0–3, with higher scores indicating greater psychological distress. The summarized minimum score of each of the seven-item subscales is 0 and the maximum 21 [46]. The reliability and validity of the Turkish version of this questionnaire has been established in Turkish patients, and it has been reported that the optimum cut-off point in the anxiety subscale score is 10 and in the depression subscale score is 7 [6]. Furthermore, in our previous study, the Turkish version of the HADS was found to be satisfactory for screening psychiatric disorders in cancer patients [5].
Structured Clinical Interview for DSM-IV—Clinical Version (SCID-I/CV)
This clinical interview inventory was described by First et al. [23] and was constructed partially towards DSM-IV Axis I diagnoses. It not only provides standardization in the process of evaluation but is also convenient to use. Turkish validity and reliability studies were performed by Ozkurkcugil et al. [38].
Statistical analysis
The Chi-squared test or the Fisher exact test for 2×2 tables was used to evaluate associations between psychiatric disorder and sociodemographic, personal and disease-related factors. Median scores for anxiety and depression were compared between groups (e.g. females vs males, patients with pain vs those without pain) using the Mann- Whitney U-test. Group means were compared using an unpaired t-test. The degree of correlation between the scores of the GHQ and HADS and the duration of cancer was determined using Pearson correlation analysis. All analyses were conducted using SPSS for Windows (version 10.0).
Results
The sociodemographic and medical data for the 117 patients are summarized in Table 1. Their mean age was 53.7±14.2 years. Female patients were significantly younger than male patients (t=−2.95, P=0.004). Most of the patients were educated to primary school level (78.5%). The time elapsed since the diagnosis of cancer was between 1 and 12 months for most of the patients (n=93, 79.5%).
Of the 117 patients, 64 (54.7%) were evaluated as being unaware of the cancer diagnosis, and 53 (45.3%) as being aware of their illness. Most patients (67.9%) stated that they had guessed the diagnosis of cancer from the treatment process or drug adverse effects. Only 17 patients (14.5%) stated that they had been fully informed about their diagnosis of cancer by their physicians. The duration of illness of 82% of the patients who were unaware of their diagnosis was less than 1 year. With regard to the relationship between awareness and cancer type, the majority (92.3%) of patients with breast cancer were aware of their diagnosis, but the proportions of patients with gynaecological cancer, gastrointestinal cancer and haematological cancer who were aware of their diagnosis were low (40%, 27% and 25%, respectively).
The standardized interviews revealed that 35 patients (30%) had a psychiatric disorder (Table 2). Adjustment disorders accounted for 48.5% of all diagnoses, and had an associated prevalence rate of 14.5%. The other most diagnostic class was major depressive disorder whose prevalence rate was 13.7% and which accounted for 45.7% of all diagnoses. Eleven patients (9.4%) had a previous psychiatric disorder, five with an anxiety disorder, five with a depressive disorder and one suffered from alcohol abuse. Psychiatric disorders were significantly more frequent among this group of patients (n=7, 63.6%) than among those without a psychiatric history (26.4%; Fisher’s exact test, χ2=6.58, P=0.01).
Pain was reported by 40 patients (34.2%). The depressive disorders (42.5%) were more frequent among cancer patients with pain than among those without pain (18.2%; χ2=7.99, P=0.005).
The prevalence of psychiatric disorder was significantly more frequent in patients who were aware of their diagnosis (39.6%, n=21) than among those who were unaware (21.9%, n=14; χ2=4.5, P=0.03). Psychiatric disorder was also more frequent in patients who guessed the diagnosis from the treatment process (38.9%) than among those who were unaware (21.9%), although the difference did not reach significance (χ2=3.3, P=0.06). The informational status with regard to cancer diagnosis was not significantly related to sociodemographic features such as sex, educational level, age, pain and stress factors.
Psychosocial stress factors were reported by 56% of the patients. Most of the stress factors were related to lack of family support (n=42, 35.9%). Of these patients, 36 (85.7%) complained of unsatisfactory relationships with their spouse and children, and suffered from helplessness and feelings of loneliness. These problems were followed by financial problems (8.5%) and employment-related stress (1.7%). Patients with psychiatric disorder had experienced considerably more psychosocial stress (n=24, 68.6%) than those without psychiatric disorder (n=11, 31.4%; χ2=8.58, P=0.0003).
The means of the total HADS scores, and the HADS depression and anxiety subscale scores, and the GHQ scores for female patients, and patients suffering from pain and lack of family support were significantly higher than those of their counterparts (Table 3). Due to the fact that the majority of breast cancer patients were aware of their diagnosis, it would be expected that these patients would suffer from more psychological distress. Since being female could have been a confounding variable for significantly higher scores on all scales, we considered it necessary to perform an additional statistical analysis excluding the 11 female patients with breast cancer. The result of this analysis showed that the mean of the scores of all scales for females were significantly higher than that for males (GHQ P=0.01, total HADS P=0.01, HADS anxiety subscale P=0.03, HADS depression subscale P=0.02).
The time elapsed from the diagnosis of cancer (in months) was positively correlated with the GHQ and HADS scores (Pearson’s correlation test: r=0.242, P=0.009; r=0.181, P=0.05). The scores of all scales were found to be significantly higher in patients whose duration of illness was more than 1 year. Suffering from a psychiatric disorder was also more common (37%) among these patients than among patients whose duration of illness was shorter than 1 year (28%), although the difference did not reach statistical significance.
Discussion
The frequency of psychiatric morbidity was 30% (according to DSM-IV criteria) in our study group which consisted of 117 cancer patients who received chemotherapy and were not in a terminal state. The prevalence of psychiatric disorder in cancer patients varies greatly among studies, ranging between 9% and 60% [1, 14, 15, 16, 31]. The 30% overall prevalence of psychiatric morbidity among cancer patients is almost the same as the 29% prevalence reported by Hardman et al. [26] and Le Fevre and Devereux [31] who used standardized psychiatric interviews. Higher prevalence rates, between 38% and 60%, were found in the other studies [2, 14, 15, 16]. The presence of organic mental disorder especially may increase the prevalence of psychiatric morbidity in terminally ill cancer patients. In their research of terminally ill cancer patients, Minagawa et al. [34] found that 53.7% of their sample met the DSM-III-R criteria for a psychiatric disorder and 42% had a cognitive impairment. The relatively low prevalence rate (30%) can be explained by exclusion of the patients with cognitive impairment from our study.
Major depression is diagnosed in cancer patients with a prevalence of 25% during the clinical course of the illness [4, 39]. Derogatis et al. [15] reported that 47% of the cancer patients in their study had a psychiatric diagnosis and adjustment disorders accounted for 68% of all diagnoses [4, 30]. Depressive disorder (45.7%) and adjustment disorder with depressive mood (42.8%) were the most common diagnoses in our patients as previously reported [2, 26]. In our study, the high GHQ and HADS scores were associated with prolonged duration of illness and being female. Studies on cancer patients suggest that prolonged duration of illness and female gender are significant risk factors for psychological distress [1, 12, 19, 36].
Our results also confirmed that prior history of psychiatric disorder, the presence of pain and family support are determinants of vulnerability to psychiatric disorder during the course of cancer, as previously reported [8, 11, 30, 33, 36]. The experience of having a life-threatening illness such as cancer would normally be expected to produce significant psychological distress and, consequently, patients with past psychiatric disorder could have difficulties in coping with the new condition. Evidence-based data indicate that pain and depression co-occur [30]. Derogatis et al. [15] reported that, of cancer patients with a psychiatric diagnosis, 39% reported severe pain, compared with only 19% of such patients who did not have a psychiatric diagnosis. Moreover, 15% of the patients with significant pain had symptoms of major depression. Similarly, psychiatric disorder—especially depression—was more common in our patients who were suffering from pain. Pain among cancer patients may have predictive value for depressive disorder. The patients with psychiatric disorders had more psychosocial stress related to family interactions in this study. Bloom and Spiegel [8] found that quality of family support was positively related to the patient’s sense of well-being. Lack of emotional and financial support causes a tendency towards anxiety and depression in cancer patients [36]. Psychosocial stress may contribute to the continuation of such psychological complaints and the development of psychiatric disorder.
Effective and clear communication is essential to the physician–patient relationship in the care of cancer patients. Despite increasing recognition of the need for effective doctor–patient communication, there are still wide variations in communication with cancer patients. In the Western world, honest disclosure to the patient of the truth about a cancer diagnosis has been the common approach. In the Middle East and the Mediterranean region, religious, social and cultural factors are also involved, whereas in the West it is regarded completely as a personal matter [25, 45]. It has been found that 97% of doctors in the USA feel that they should tell the patient about his/her fatal illness and 78% of them have already done so [32, 42]. But in many countries nondisclosure is still common [27, 28]. Over half of our patients (54.7%) being unaware of their cancer diagnosis may be explained in two ways.
First, the low rate of awareness may reflect the attitude of the doctor in avoiding informing patients about a cancer diagnosis, as found in studies from the other oriental countries [13, 20, 45]. Clinical experience and research evidence suggest that many cancer patients in Turkey are not well informed about their diagnosis and prognosis, although relatives are informed [16]. The diagnosis of cancer is interpreted as being equivalent to a death sentence by most people in Turkey, as in many Middle Eastern countries. Therefore, the family of a patient may insist on the patient not hearing the word cancer [16, 41, 43]. They often fear that the outcome of treatment could be negatively affected by the patient being informed of the actual condition by a health professional, and the patient could develop severe psychiatric problems. As a result, it has been reported that 40% of physicians have never informed their patients about a cancer diagnosis and the percentage of patients knowing their diagnosis is low (27–44%) in studies from Turkey [10, 16, 17, 18, 21]. However, two Turkish studies have shown that 82–88% of patients with cancer are aware of their diagnosis. The authors concluded that this high percentage may reflect a concerted effort to increase the level of physician–patient communication about diagnosis and prognosis in their institutions [41, 43].
Second, the low rate of awareness may be related to denial as a defence mechanism. It is well known that patients may often react with denial in the early period of the disease [22]. Most of our patients who were in the early period of their disease were considered to be unaware of the diagnosis of cancer. When confronted initially with a diagnosis of cancer, most patients experience a short period of shock, such that the diagnosis may actually be disbelieved. In this period, denial acts as a defence mechanism permitting the patient to avoid awareness of some painful aspects of the diagnosis. There are some inconclusive reports that denial is more commonly found in oriental cultures [2, 7, 17]. Two Turkish studies imply that 60–70% of cancer patients may use the defence mechanism of denial [21, 37].
A lower rate of psychiatric disorder was observed in the unaware patients in the present study. Similarly, in India, which has an Eastern culture, it has also been demonstrated that psychiatric disorders occur to a lesser extent in patients who are not aware of their cancer diagnosis. The authors concluded that these patients had a more hopeful outlook as to the outcome of treatment [2, 13]. On the other hand, most of the aware patients in our study group were not well informed by their physicians about the cancer diagnosis and they stated that they obtained information indirectly. This may be related to the higher frequency of psychiatric disorders in the aware patients. Communication and providing satisfactory information about diagnosis, treatment and consent have important implications for psychological adjustment of cancer patients [35, 41, 43]. Understanding of the diagnosis indirectly, without having satisfactory information, may cause the individual to be stressed because of arousing suspicions of cancer and of the treatment. The uncertainty may lead to the intrapersonal conflicts and consequently the risk of psychiatric disorders may increase.
In conclusion, this study showed that 30% of cancer patients met the criteria for a psychiatric disorder, and the most common type was an adjustment disorder. Additionally, our results confirm that psychiatric disorders were closely related to factors such as the period of illness, previous psychiatric problems, pain, stress and female gender. Unlike patients reported from Western countries, there was a low awareness of cancer diagnosis in our study group. This can be explained by poor physician–patient communication or by denial. In Turkey, because the diagnosis of cancer is generally regarded as a death sentence, physicians may be reluctant to reveal the exact diagnosis and prognosis to the patient directly. Perhaps this uncertainty may contribute to denial as a way of preventing hope for patients. The high prevalence of psychiatric disorders among the aware patients may be related to having inadequate information. Supporting systems through which patients can get more information and learn coping skills seems to be essential.
The methodological advantage of this study was its detailed evaluation of the psychopathology using structured interviews and standard diagnostic criteria. However, the study sample was not large, and the results cannot be representative of all cancer patients in Turkey. Nevertheless there is a clear need in Turkey to provide more informational support to patients with cancer.
References
Aass N, Fossa SD, Dahl AA, Moe TJ (1997) Prevalence of anxiety and depression in cancer patients seen at the Norwegian Radium Hospital. Eur J Cancer 33:1597–1604
Alexander PJ, Dinesh N, Vidyasagar MS (1993) Psychiatric Morbidity among cancer patients and its relationship with awareness of illness and expectations about treatment outcome. Acta Oncol 32:623–626
American Psychiatric Association (1994) DSM-IV—diagnostic and statistical manual of mental disorders, 4th edn. American Psychiatric Association, Washington DC
Angelino AF, Treisman GJ (2001) Major depression and demoralization in cancer patients: diagnostic and treatment considerations. Support Care Cancer 9:344–349
Atesci FC, Oguzhanoglu NK, Baltalarlı B, Karadağ F, Özdel O, Karagöz N (2003) Psychiatric disorders in cancer patients and associated factor. Turk J Psychiatry 14:145–152
Aydemir O (1997) Validity and reliability of Turkish version of Hospital Anxiety and Depression Scale. Turk J Psychiatry 8:280–287
Baider L, Sarell M (1983) Perceptions and causal attributions of Israeli women with breast cancer concerning their illness: the effects of ethnicity and religiosity. Psychother Psychosom 39:136–143
Bloom JR, Spiegel D (1984) The relationship of two dimensions of social support to the psychological well-being and social functioning of women with breast cancer. Soc Sci Med 19:831–837
Bottomley A (1998) Depression in cancer patients: a literature review. Eur J Cancer 7:181–191
Bozcuk H, Erdoğan V, Eken C, et al (2002) Does awareness of diagnosis make any difference to quality of life? Determinants of emotional functioning in a group of cancer patients in Turkey. Support Care Cancer 10:51–57
Breitbart W (1995) Identifying patients at risk for, and treatment of major psychiatric complications of cancer. Support Care Cancer 3:34–60
Caroll BT, Kathol RG, Noyes R, et al (1993) Screening for depression and anxiety in cancer patients using the Hospital Anxiety and Depression Scale. Gen Hosp Psychiatry 15:69–74
Chandra PS, Chaturvedi SK, Kumar A, et al (1998) Awareness of diagnosis and psychiatric morbidity among cancer patients—a study from South India. Psychosom Res 45:257–261
Costantini M, Musso M, Viterboli P, et al (1999) Detecting psychological distress in cancer patients: validity of the Italian version of the Hospital Anxiety and Depression Scale. Support Care Cancer 7:121–127
Derogatis LR, Morrow GR, Fetting J (1983) The prevalence of psychiatric disorder among cancer patients. JAMA 297:751–757
Devrimci H, Unluglu G (1998) Psychiatric morbidity in cancer patients and their relatives. J Psychiatry Psychol Psychopharmacol 6:196–206
Elbi H (1998) Psycho-oncology. J Psychiatry Psychol Psychopharmacol 6:5–7
Elbi H, Ozaydemir G, Tamar M, Saygılı R, et al (1992) Psychosocial problems and approach in a group cancer patients. XVIIth Congress of the European Society for Medical Oncology. 7–10 November, Lyon
Ell K, Nishimoto R, Morvay T, et al (1989) A longitudinal analysis of psychological adaptation among survivors of cancer. Cancer 63:406–413
Elwyn TS, Fetters MD, Gorenflo W, Tsuda T (1998) Cancer disclosure in Japan: historical comparisons, current practices. Soc Sci Med 46:1151–1163
Ersoy MA (2000) Investigation of relationships between denial, relationships with the treatment team, being informed, knowing the diagnosis, resort to alternative treatment methods and diagnosis. J Psychiatry Psychol Psychopharmacol 8:17–26
Fawzy FI, Greenberg DB (1996) Oncology. In: Rundel JR, Wise MG (eds) Textbook of consultation-liaison psychiatry. American Psychiatric Press, Washington DC, pp 673–694
First MB, Spitzer RL, Gibbon M, Williams JBW (1997) Structured clinical interview for DSM-IV clinical version (SCID-I/CV). American Psychiatric Press, Washington DC
Ford S, Lewis S, Fallowfield L (1995) Psychological morbidity in newly referred patients with cancer. J Psychosom Res 39:193–202
Gordon DR, Paci E (1997) Disclosure practices and cultural narratives: understanding concealment and silence around cancer in Tuscany, Italy. Soc Sci Med 44:1433–1452
Hardman A, Maguire P, Crowther D (1989) The recognition of psychiatric morbidity on a medical oncology ward. J Psychosom Res 33:235–239
Holland JC, Geary N, Marchini A, et al (1987) An international survey of physician attitudes and practice in regard to revealing the diagnosis of cancer. Cancer Invest 5:151–154
Hosaka T, Awazu H, Fukunishi I, Okuyama T, Wogan J (1999) Disclosure of true diagnosis in Japanese cancer patients. Gen Hosp Psychiatry 21:209–213
Kılıc C (1996) General health questionnaire: a validity and reliability study. Turk J Psychiatry 7:3–9
Lancee WJ, Wachon MLS, Ghadirian P, et al (1994) The impact of pain and impaired role performance on distress in persons with cancer. Can J Psychiatry 39:617–622
Le Fevre P, Devereux J (1999) Screening for psychiatric illness in the palliative care inpatient setting: a comparison between the Hospital Anxiety and Depression Scale and the General Health Questionnaire-12. Palliat Med 13:399–409
Levy NB (1988) Fatal illness: what should the patient be told? In: Klagsbrun SC, Goldberg IK, Rawnsley MM (eds) Psychiatric aspects of terminal patients. Charles Press, Philadelphia, pp 42–46
Massie M, Holland J (1990) Depression and the cancer patient. J Clin Psychiatry 51:12–17
Minagawa H, Uchitomi Y, Yamawaki S, Ishitani K (1996) Psychiatric Morbidity in terminally ill cancer patients. Cancer 78:1131–1137
Montgomery C, Lydon A, Lloyd K (1999) Psychological distress among cancer patients and informed consent. J Psychosom Res 46:241–245
Nordin K, Berglung G, Glimelius B, Sjöden PO (2001) Predicting anxiety and depression among cancer patients: a clinical model. Eur J Cancer 37:376–384
Ozkan S, Turgay M (1992) Psychiatric morbidity and psychosocial adjustment in mastectomy and the relationship between cancer-organ loss and psychopathology. Arch Neuropsychiatry 29:207–215
Ozkurkcugil A, Aydemir O, Yildiz M, Esen Danaci A, Koroglu E (1999) Adaptation to Turkish and reliability study of Structured Clinical Interview for Axial I disorders. J Drug Treat 2:233–236
Pirl FW, Roth JA (1999) Diagnosis and treatment of depression in cancer patients. Oncology 13:1293–1306
Roth AJ, Holland JC (1994) Treatment of depression in cancer patients. Primary Care Cancer 14:23–29
Sen M (1997) Communication with cancer patients. The influence of age, gender, education, and health insurance status. Ann N Y Acad Sci 809:514–524
Surbone A (1992) Truth telling to the patients. JAMA 268:1661–1662
Turhal NS, Efe B, Gumus M, et al (2002) Patient satisfaction in the outpatients’ chemotherapy unit of Marmara University, Istanbul, Turkey: a staff survey. BMC Cancer 2:30–35
Valente SM, Saunders F (1997) Diagnosis and treatment of major depression among people with cancer. Cancer Nurs 20:168–177
Younge D, Moreau P, Ezzat A, Gray A (1997) Communicating with cancer patients in Saudi Arabia. Ann N Y Acad Sci 809:309–316
Zigmond AS, Snaith PR (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67:361–337
Author information
Authors and Affiliations
Corresponding author
Additional information
This paper was accepted as a poster presentation at the European Conference of Clinical Oncology (ECCO) Congress held in Copenhagen, 21–25 September 2003.
Rights and permissions
About this article
Cite this article
Atesci, F.C., Baltalarli, B., Oguzhanoglu, N.K. et al. Psychiatric morbidity among cancer patients and awareness of illness. Support Care Cancer 12, 161–167 (2004). https://doi.org/10.1007/s00520-003-0585-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-003-0585-y