Abstract
Goals of work
Caregivers have become part of a triad of care and frequently attend patient consultations in the ambulatory cancer setting. Effective caregiving and decision making require that they understand the course of the disease and the changing treatment goals. This study sought to evaluate caregiver perception of treatment intent.
Patients and methods
A cohort of 317 subjects (181 patients and 136 caregivers) from The Canberra Hospital's Cancer Services were followed for 6 months. Caregiver understanding of patient treatment intent was measured over time together with sources of information.
Main results
Most caregivers understood that the illness was life-threatening (92% at week 12) and that treatment goals were to control illness and improve quality of life. Only half understood that treatment was noncurative (48% at week 12); 27% were unsure and 25% believed that treatment would cure. A high proportion of caregivers identified the specialist as the source of information (77%) and almost half also included the general practitioner (47%). These figures remained fairly constant over time. There were significant gender and age differences in understanding. At baseline, more women than men had an accurate perception of treatment intent and these numbers increased over time. Men's perception did not change.
Conclusions
Caregivers' ability to fully engage in the task of caring for those with a terminal illness may be hampered by their lack of understanding of the treatment patients receive.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Family caregiving is an indispensable part of the care and management of patients with cancer. The responsibility and burden upon family members have increased as more cancer including advanced cancer is treated in an ambulatory setting. Research on the role of family caregivers is still sparse, focusing mainly on the impact of caring on caregivers' psychological and physical health.
An early review of the literature concerning communication about cancer concluded that caregivers feel the need to conceal their feelings, have difficulty acquiring information and identify their chief emotional problem as coping with helplessness [1]. In these descriptive studies families said that they have difficulties contacting physicians [2, 3]. Reviewing the information needs of families of cancer patients, Houts et al. confirmed that their key problem is a lack of medical information in regard to the course of the disease [4]. All studies have found that family caregivers have marked difficulties in both obtaining information and understanding what is happening [5, 6, 7, 8, 9, 10].
Recent research is shedding new light on the process of cancer family caregiving [11, 12]. Caregivers need knowledge to define, act on and organize around the patient's illness [13]. Olesen outlined food preparation, emotional management and monitoring health practices as productive work in caring for people who are ill. With appropriate information, patient/family decision making can ensure that the family tasks of assistance with self-care and the conduct of medical care are blended with those of the health team. Equally important, family matters such as emotional care, financial management and the provision of social support can be structured to respond to individual patient and family need [14].
Research on perceptions of a good death undertaken in the 1990s has drawn attention to differences in the utilization of health systems internationally. In the UK a retrospective study found that most people are now aware when they are dying, in contrast to an earlier study in which most people were unaware of their impending death. This increased awareness is associated with family caregivers knowing for some time that the patient is dying [15]. British hospice best practice recommends that attention be paid to the individual nature of each family's information needs relating to illness and prognosis [16]. It has been found that caregiver knowledge of impending death helps ensure access to hospice care and enables a greater opportunity for the patient to die at home. Family ties are strengthened with the opportunity for close relatives to be present at the time of death [17].
The introduction of managed care in the US and increased ambulatory cancer care have now highlighted the need for decision making to be a negotiated process between physicians, patients and their families in which information and decision making are increasingly shared [18, 19]. The necessity to expand the research focus to understand different cultural perceptions surrounding death and dying is also acknowledged as a priority [20]. In Australia, health-promotion strategies have been incorporated into palliative care with an emphasis on community education and information [21].
The theoretical model of Weitzner et al. develops the stress process model as a way for clinicians to view the emerging large-scale social challenge of caregiving [22]. Because caring for a dying relative is stressful, family caregivers—like other people experiencing stress—require realistic appraisal of their situation in order to be able to cope. Individual appraisal relies upon effective information sharing between patient, family, and health-care team.
The work reported here, part of a larger longitudinal study, sought to measure caregivers' knowledge of patient illness and their sources of knowledge measured over time. The aims were:
-
To measure caregiver knowledge of treatment intent
-
To identify caregiver sources of information about the illness
-
To investigate associations over time between caregiver knowledge of treatment intent and selected variables, including sources of information
Patients and methods
Study population
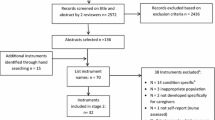
The Canberra Cancer Quality of Life Project (CCQLP) was designed to observe the experience of patients with advanced cancer and their caregivers. The study randomly selected 237 patients over 18 years of age. All patients had a diagnosis of incurable malignant disease with symptoms attributable to their disease or anticipated as likely to occur within a 6-month observation period. Of the 237, 183 (77%) agreed to participate, 1 withdrew and 1 died, leaving 181 patients at enrolment. Caregivers were described as "a carer or support person, e.g. a spouse/partner, other relative or friend who gives you physical and/or emotional support". Caregivers were nominated by 167 (92%), of whom 136 agreed to participate. Patients were observed until March 2003 to record deaths, at which time nine only remained alive. All participants gave written informed consent. Approval was given by the Australian Capital Territory (ACT) Health and Community Care Ethics Committee.
The survey instrument for this report was completed by 136 caregivers at week 1, and 92 caregivers at week 12. Loss to follow-up was due to the death of 18 patients. The remaining caregivers included 5 where the patient was seriously ill, and the remainder tended to be Australian, living in the non-metropolitan area, were the child of the patient and were more likely to be aged under 50 years.
Data collection
Patients screened from March to August 1996 were enrolled together with their caregivers. Trained nurse interviewers collected data for this study during weeks 1 and 12.
Measures
Questionnaires were administered at enrolment to obtain relevant sociodemographic and clinical characteristics of patients and caregivers. A survey instrument to obtain details of information-giving was presented at week 1. We sought to determine caregiver knowledge of patient treatment intent, whether they understood that the illness was life threatening and to identify their sources of information. Three aspects of treatment goals were specified: to monitor the illness, to improve quality of life, and to control the illness. A fourth aspect was included to evaluate overall perception of treatment intent and asked whether they considered treatment was to cure. All four dimensions offered a three-point response scale—yes, no, don't know. A wide-ranging index of sources of information was offered with more than one response permitted. Categories were based on interpersonal communication (formal and informal) and written and other media (commercial and educational).
Data analysis
Sociodemographic and clinical variables were designed to ensure a comprehensive picture. We sought to capture the illness course of the patient population who were in reality approaching death using three types of analytic measures: the Eastern Cooperative Oncology Group (ECOG) measure, a time to death measurement, and a psychosocial classification. The ECOG indicator is now accepted throughout cancer medicine worldwide. It uses an ordinal approach for clinical evaluation of physical functioning amongst a cancer patient population:
- 0:
-
Able to carry out normal activities without restriction
- 1:
-
Ambulatory—capable of light work, restricted with strenuous activity
- 2:
-
Ambulatory—capable of self-care, but unable to work
- 3:
-
Resting in bed/chair more than half waking hours, only capable of limited self-care
- 4:
-
Totally confined to bed/chair, not capable of any self-care
- 9:
-
Not recorded
Time to death was accurately determined for all respondents by accessing the Australian National Death Index in conjunction with the clinical records within the Canberra Hospital and the ACT Health System. A four-stage classification captured the distribution of mortality amongst the sample. In addition, we calculated a psychosocial stage of disease classification that records time phases in the natural history of disease [23]. The variable was constructed by defining the crisis phase as 90 days from diagnosis and calculating the terminal phase as 60 days from date of death. The chronic phase was calculated as the period between these time-points. For patients who died within 90 days of diagnosis, the period before death was classified as crisis phase.
The characteristics of caregiving captured aspects of primary and secondary caregiving, key details related to household composition, and the impact of caring on employment patterns and social activity. Specific information was sought in regard to whether caregivers accompanied the patient to the clinical consultation, their perception of the amount of average weekly assistance they provided and some global indices of difficulty in caregiving were sought.
Statistical analysis
Simple kappa statistics were used to assess the magnitude of association. The statistical significance of these associations was assessed using McNemar's test. All statistical analyses were done using both the SPSS and the SAS statistical software packages.
Results
Patient and caregiver characteristics
Sociodemographic, clinical and care characteristics of patients and caregivers are presented in Tables 1 and 2. Most patients nominated a caregiver. Only 14 patients (7.7%) did not nominate a caregiver. The characteristics of patients not nominating a caregiver were similar to those who did nominate, with the exception of marital status: only 3 of the 14 patients not nominating a caregiver were married compared with 124 of 167 patients with caregivers (P<0.001, Fisher's exact test).
While most caregivers were married to the patient (71.5%), adult daughters (17%) also provided care, and a small cluster comprised either relatives or friends (8%), or were parents (3%). Most caregivers were married (88%) and 12% had dependent children. A comparatively high number of caregivers were male (35%). One-fifth of caregivers did not live in the same household as the patient. One-quarter had taken leave or stopped work as a result of their caring role. They were supplying substantial amounts of care: more than 80% had given an average of over 10 h weekly in the past month, the majority invested more than 30 h weekly and one-quarter undertook over 100 h weekly. Caregivers identified a web of secondary supports for themselves, nominating their daughters (48.5%), and sons (39.7%) as well as siblings (around 18%). There were, however, 16% of caregivers who had no-one to support them in their role. Most caregivers attended patient consultations (87%), and 62% did so regularly.
Knowledge of illness
All caregivers were aware that the patient had a cancer diagnosis. Most understood that the illness was life threatening (89.5% at week 1 rising to 92% at week 12). The majority of caregivers understood that treatment intent was both to improve patient quality of life and to control the illness. However, fewer than half clearly understood the fundamental aspect that treatment was noncurative. One-quarter believed that treatment was to cure (Table 3).
Over time, there was little change in caregivers' knowledge of treatment intent but a trend towards improved understanding was discernible (Table 3). While at week 1, 40% said they understood that treatment would not cure, by week 12 this figure had increased to 48.2%. A large proportion (77%) nominated the specialist and just under half mentioned the general practitioner (47%) as sources of illness information (Table 4). For more than one-third of the caregivers the patient was an important source of knowledge of the illness, but other family members and friends had little input. Few caregivers identified written information about the illness from either commercial or educational sources.
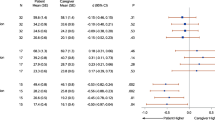
In the quest to understand whether subpopulation differences in our sample were evident, or whether patients' clinical or caring factors determined response patterns amongst their caregivers, a bivariate analysis was undertaken. Both sociodemographic and clinical characteristics were identified as important and a number were significant (P<0.05; Table 5). Predictors for believing that treatment intent was "to cure" included caregiver gender, age and whether they were employed or not (see Table 5). More males (35%) than females (19%) thought treatment was curative (P=0.01). Most of those aged under 40 years (73%) understood that treatment was not expected to cure, with 10.5% saying they didn't know. By contrast, amongst those over 70 years of age, 21.7% said that treatment was noncurative and almost half (47.8%) said they did not know. Amongst caregivers who had stopped work to care, almost twice as many as those still working or retired/unemployed had a correct grasp of treatment goals.
A range of patient clinical characteristics and the course of the illness were significant. Caregivers of lung cancer patients showed comparatively high levels (66.7%) of accurate understanding of treatment, in contrast to caregivers of patients with breast cancer and cancer of the ovary of whom around half believed that treatment was curative. Many caregivers (43.4%) of patients recruited through radiation oncology indicated uncertainty as to whether treatment was curative in intent.
The stage of patient illness highlighted the evolution of caregiver understanding. Caregivers were frequently optimistic when the patient was more than 1 year from death (Table 5). But a realistic trend was clearly demonstrated in the last year of life, with very few caregivers still believing treatment to be curative when there was less than 1 year of life remaining. In the last 6 months of life, almost no caregivers believed treatment would cure and two-thirds were clear that treatment was noncurative.
Cross-tabulation of caregiver response to aim of treatment at weeks 1 and 12 provided insight into the pattern of response: 30 of 85 respondents understood at both times that treatment was noncurative (Table 6). There were four respondents who shifted from an accurate perception at week 1 to a view that treatment would cure (one) or that they no longer knew the aims of treatment (three). The overall improvement in awareness (41 respondents) flowed in almost equal proportions from the other two categories of response.
Discussion
This cancer caregiving population contained more male caregivers than previously estimated for caregivers of Australian cancer and non-cancer patients [24]. This may reflect our patient population, of whom nearly a quarter had breast cancer. Along with spousal caregivers, our study identified adult daughters caring for aged parents and other smaller groups including other family/friends caring for those without a partner and parents caring for children. Adult sons did not undertake a primary caring role in the main, but did provide secondary support within the extended family network.
Our findings confirm that family caregivers in the advanced cancer care setting are part of the health-care triad. Most attend some medical consultations and 62% do so often. The majority of caregivers appreciated the serious nature of the illness in that they acknowledged it was life threatening and that treatment was aimed only at controlling the illness and its symptoms. Most agreed that the treatment aim was also to improve quality of life with the notable exception of elderly caregivers.
However, fewer than half understood that treatment was noncurative. One-quarter believed treatment intent to be curative. Caregivers indicated that they relied overwhelmingly on the medical team for information about the patient's illness: four-fifths identified the specialist, with around half also including the general practitioner as their source. While we found most caregivers attended consultations most of the time, qualitative research in the US exploring physicians' patterns of cancer consultation have noted an individualistic approach to the doctor-patient relationship. In fact, Miyaji found that physicians who saw themselves as the principal information-giver at times expressed a distrust of family members [25]. By contrast the family member is accorded the right of involvement in cultures such as the southern European countries of Italy, Greece and Spain, as well as India and the Arab states [26]. Disclosure of prognosis goes to the heart of the patient's (and implicitly the caregiver's) understanding of the goals of treatment and of its critical nature in the advanced cancer setting. Interviews with physicians in both the US and the UK confirm doctors' information-giving as a process that showed marked difference in discussions of treatment compared with prognosis. Miyaji reports that while full details are frequently given in regard to treatment, many physicians are deliberately vague when discussing prognosis, giving optimistic estimates and using euphemisms [25, 27, 28, 29]. Recent research has shown that doctors are only prepared to provide a frank estimate in 37% of cases [30]. Medical practitioners explained they shape their evaluation of what a patient wishes to know to fit an estimate of the patient's intellectual capacity and emotional state, and researchers have concluded that information sharing with patients and caregivers may often be inhibited [25, 27].
Our findings emphasize the relevance of gender to caregiving through its association with treatment knowledge. Women in this study demonstrated better knowledge of what was happening both initially and over time. By contrast, twice the proportion of men as women did not correctly understand treatment intent, and showed no improvement in their understanding over time. Recent research into the stress response has introduced gender as an important factor in differing responses. The concept used for 70 years of the "fight/flight" syndrome has been complemented by the new concept of "tend/befriend" in which women are said to engage when under stress [31]. These differing responses may in cancer care lead to a range of behavioural repertoires underpinning caregivers' perception of their role and enable women to draw upon a range of resources to help clarify the nature of the problem and how best to respond. Age was a significant predictor of knowledge amongst these caregivers, with 74% of caregivers under 40 years of age (compared with only 22% of those over 70 years) having accurate knowledge. This may be because the management of the information-giving process appears still to be dominated by physicians who may communicate differentially across age strata, affecting dissemination of accurate knowledge [25].
While many caregivers had optimistic misconceptions when patients were 2 years and more from death, by the time of the terminal phase (the last 6 months) many more caregivers (60%) had obtained accurate knowledge, and major distortions in their understanding had disappeared. Family caregivers in the advanced cancer setting have been identified as using three specific strategies to manage their emotional struggle: hoping, pretending and preparing for death [32]. Timmermans' qualitative research found that the process of developing an awareness of dying is a gradual one for family caregivers [33]. It is characterized by uncertainty and anguish. It was found that the uncertainty is heightened at times by interactions with health-care providers. Our findings would seem to confirm the analysis of Timmermans in the trends uncovered in our time-from-death analysis. We found that those caregivers who had ceased full-time employment had a relatively accurate understanding of the treatment aims. We could not determine causality—whether knowledge led to withdrawal from the workforce, or whether withdrawal facilitates acquisition of knowledge. This pattern may be due to gradual clarification with changing disease stage, or greater opportunity to discuss illness with the patient and health-care providers, or the opportunity to create with the patient and for themselves a more emotionally supportive environment. While patients, observed over time in St Christopher's Hospice in the UK, were found to only slightly increase their awareness of dying over time, their caregivers in contrast progressed markedly in their understanding [34].
It was beyond the scope of this study to assess the communication ability of individual clinicians, or to control for treatment and other professional patient interactions. Since most caregivers attended consultations in this cohort, it is possible that the predominantly male physicians in the consultation room with the female patients and male caregivers focused on life-extending treatment options. An Australian cross-sectional study specifically exploring information needs in regard to prognosis of women with early-stage breast cancer has confirmed that the patients rarely understand the statistical language used by cancer specialists [35]. Do doctors respond to their female patients in a different way to male patients in discussing prognosis? While research is still limited on how doctors discuss treatment options, we do know that it is closely related to the realities of clinical practice including their own emotional coping [25]. It also may be that doctors' own emotional responses are influenced by caregiver gender and be part of the explanation for why nearly half the male caregivers believed that treatment was curative for patients with breast or ovarian cancer, while most caregivers of patients with lung cancer understood that treatment was noncurative. It may also be due to the overall differences in baseline prognosis for breast cancer compared to lung cancer (and other cancers) that affects either slower uptake of updated prognoses, or attenuated communication of the changed status by the physician.
We had insufficient statistical power to conduct a multivariate analysis of explanatory variables for respondent knowledge of treatment intent. A study with a larger sample and an extension of the study follow-up with additional measures would be needed to elucidate influences on caregivers' knowledge over time. This study sought to measure knowledge content. As there is as yet no suitable validated instrument to measure this domain, there may be considerable misclassification and measurement error for this variable in our study. Despite these shortcomings, this study provides valuable baseline prevalence measures of caregiver knowledge and changes in their knowledge over time.
Conclusions
Our study provides prevalence estimates for caregiver understanding of treatment intent for patients seriously ill with cancer. Only around half understood that treatment was noncurative. While age differences in understanding of medical information have been established for some time in the literature, only recently have studies begun to examine gender differences. We found women caregivers to be more successful than men in understanding treatment goals.
Our findings indicate that there is unacceptably low understanding of treatment intent amongst caregivers for patients with advanced cancer. More understanding of the dynamics is needed, including an examination of the determinants of awareness. Without additional information it is not possible to recommend feasible, practical suggestions for changes that may improve this caregiver awareness. Questions that further explore gender, cultural, age and educational differences, the potential differential of information-giving by health workers, and the role of self-preservation amongst the caregivers first need to be addressed through more research. Answers to these questions will enhance understanding of how people cope and lead to suggested strategies.
Research and service providers must develop a better understanding of how to support family caregivers if "the care triad" is to supply optimum care to cancer patients, and to avoid imposing an undue burden on family members who care for them.
References
Northouse PG, Northouse LL (1987) Communication and cancer: issues confronting patients, health professionals, and family members. J Psychosoc Oncol 5:17–45
Bond S (1982) Relatively speaking—communicating with families of cancer patients. The relatives and doctors. part 1. Nurs Times 78:962–965
Krant MJ, Johnston L (1977) Family members' perceptions of communications in late stage cancer. Int J Psychiatry Med 8:203–216
Houts PS, Rusenas I, Simmonds MA, Hufford DL (1991) Information needs of families of cancer patients: a literature review and recommendations. J Cancer Educ 6:255–261
Tringali CA (1986) The needs of family members of cancer patients. Oncol Nurs Forum 13:65–70
Cooper ET (1984) A pilot study on the effects of the diagnosis of lung cancer on family relationships. Cancer Nurs 7:301–308
Maguire P, Faulkner A (1988) Communicate with cancer patients: 2. Handling uncertainty, collusion, and denial. BMJ 297:972–974
Hinds C, Streater A, Mood D (1995) Functions and preferred methods of receiving information related to radiotherapy. Perceptions of patients with cancer. Cancer Nurs 18:374–384
Dyck S, Wright K (1985) Family perceptions: the role of the nurse throughout an adult's cancer experience. Oncol Nurs Forum 12:53–56
Hockley JM, Dunlop R, Davies RJ (1988) Survey of distressing symptoms in dying patients and their families in hospital and the response to a symptom control team. Br Med J (Clin Res Ed) 296:1715–1717
Thomas C, Morris SM (2002) Informal carers in cancer contexts. Eur J Cancer Care (Engl) 11:178–182
Nijboer C, Tempelaar R, Triemstra M, van den Bos GA, Sanderman R (2001) The role of social and psychologic resources in caregiving of cancer patients. Cancer 91:1029–1039
Olesen VL (1989) Caregiving, ethical and informal: emerging challenges in the sociology of health and illness (review). J Health Soc Behav 30:1–10
Nijboer C, Tempelaar R, Sanderman R, Triemstra M, van den Spruijt RJ, et al (1998) Cancer and caregiving: the impact on the caregiver's health (review). Psychooncology 7:3–13
Seale C, Addington-Hall J, McCarthy M (1997) Awareness of dying: prevalence, causes and consequences. Soc Sci Med 45:477–484
Rose KE (1999) A qualitative analysis of the information needs of informal carers of terminally ill cancer patients. J Clin Nurs 8:81–88
Seale C (1995) Dying alone. Sociol Health Illness 17:376–392
Haug MR (1994) Elderly patients, caregivers, and physicians: theory and research on health care triads (review). J Health Soc Behav 35:1–12
Steinhauser KE, Christakis NA, Clipp EC, McNeilly M, McIntyre L, Tulsky JA (2000) Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA 284:2476–2482
Steinhauser KE, Clipp EC, McNeilly M, Christakis NA, McIntyre LM, Tulsky JA (2000) In search of a good death: observations of patients, families, and providers. Ann Intern Med 132:825–832
Kellehear A (1999) Health promoting palliative care. Oxford University Press, Oxford
Weitzner MA, Haley WE, Chen H (2000) The family caregiver of the older cancer patient. Hematol Oncol Clin North Am 14:269–281
Rolland JS (1994) Families, illness, and disability: an integrative treatment model. Basicbooks, New York
Schofield HL, Herrman HE, Bloch S, Howe A, Singh B (1997) A profile of Australian family caregivers: diversity of roles and circumstances. Aust N Z J Public Health 21:59–66
Miyaji NT (1993) The power of compassion: truth-telling among American doctors in the care of dying patients. Soc Sci Med 36:249–264
Surbone A, Zwitter M (eds) (1997) Communication with the cancer patient: information and truth. Ann N Y Acad Sci 809:1–540
Delvecchio Good MJ, Good BJ, Schaffer C, Lind SE (1990) American oncology and the discourse on hope. Cult Med Psychiatry 14:59–79
Burton MV, Parker RW (1997) Psychological aspects of cancer surgery: surgeons' attitudes and opinions. Psychooncology 6:47–64
The AM, Hak T, Koeter G, van Der Wal G (2000) Collusion in doctor-patient communication about imminent death: an ethnographic study. BMJ 321:1376–1381
Lamont EB, Christakis NA (2001) Prognostic disclosure to patients with cancer near the end of life. Ann Intern Med 134:1096–1105
Taylor SE, Klein LC, Lewis BP, Gruenewald TL, Gurung RA, Updegraff JA (2000) Biobehavioral responses to stress in females: tend-and-befriend, not fight-or-flight. Psychol Rev 107:411–429
Yates P, Stetz KM (1999) Families' awareness of and response to dying. Oncol Nurs Forum 26:113–120
Timmermans S (1994) Dying of awareness: the theory of awareness contexts revisited. Sociol Health Illness 16:322–336
Hinton J (1999) The progress of awareness and acceptance of dying assessed in cancer patients and their caring relatives. Palliat Med 13:19–35
Lobb EA, Kenny DT, Butow PN, Tattersall MH (2001) Women's preferences for discussion of prognosis in early breast cancer. Health Expect 4:48–57
Acknowledgements
This study was undertaken as part of the Canberra Cancer Quality of Life Project funded by the Australian Commonwealth Department of Health and Community Services. The authors wish to thank patients and their caregivers for their participation and medical, nursing and social work colleagues for their support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Burns, C.M., Dixon, T., Broom, D. et al. Family caregiver knowledge of treatment intent in a longitudinal study of patients with advanced cancer. Support Care Cancer 11, 629–637 (2003). https://doi.org/10.1007/s00520-003-0501-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-003-0501-5