Summary
Background
Glaucoma is a chronic and serious disease calling for consistent lifelong therapy. The patient’s compliance requires that he/she be well informed about the disease. The purpose of the present study was to determine the level of knowledge about glaucoma, and compare young patients with older ones as well as glaucoma patients with nonglaucoma ones.
Methods
A total of 1110 questionnaires were distributed to patients and their relatives at the outpatient eye clinic of Hietzing Hospital (Vienna), of which 1041 were returned. The questionnaire comprised 18 questions. Patients were divided into two groups: group 1 consisted of those aged 18–60 years, while group 2 consisted of those older than 61 years.
Results
In total, 941 questionnaires were evaluated; 72.8 % of the respondents were older than 60 years, and one-half of the respondents had glaucoma (51 %). The majority of patients had “moderate knowledge” of the disease (41.87 %), followed by “poor knowledge” (32.52 %). Glaucoma patients had considerably better knowledge of the disease (p < 0.01) than did nonglaucoma patients. Younger patients were significantly better informed than older ones (p < 0.01). Nonglaucoma patients with a positive diagnosis of glaucoma among their circle of friends or family were significantly better informed (p < 0.01) than those without such persons in their circle of friends.
Conclusion
Persons with glaucoma are much better informed about the disease than nonglaucoma patients, but the general level of knowledge is very low. Notably, younger patients were better informed than older ones. The present study, comprising a large number of patients, revealed poor knowledge of glaucoma among patients with the disease and especially among nonglaucoma patients in Vienna.
Zusammenfassung
Grundlagen
Das Glaukom ist eine chronische, schwerwiegende Erkrankung, welche eine lebenslange, konsequente Therapie erfordert. Voraussetzung für eine gute Compliance ist ein ausreichendes Wissen der PatientInnen zu dieser Erkrankung. Aus diesem Grund war das Studienziel die Ermittlung des Glaukom-Wissensstandes, im Vergleich junge PatientInnen/ältere PatientInnen, Selbstbetroffener/nicht Betroffener.
Methodik
Es wurden 1110 Fragebögen in der Augenambulanz Hietzing verteilt und von 1041 PatientInnen bzw. Angehörigen wieder retourniert. Die Umfrage enthielt insgesamt 18 Fragen. Die PatientInnen wurden in Gruppe 1: (18–60 Jahre) und Gruppe 2: (ab 61 Jahre) geteilt.
Ergebnisse
Ausgewertet wurden 941 Fragebögen. 72,8 % der Befragten waren über 60 Jahre alt. Die Hälfte aller Befragten litt an einem Glaukom (51 %). Der Hauptanteil aller PatientInnen hatte ein „durchschnittliches Wissen“ (41,87 %) gefolgt von „geringes Wissen“ (32,52 %). GlaukompatientInnen wussten signifikant mehr (p < 0,01) als Nichtbetroffene. Es zeigte sich ein signifikant besseres Wissen bei jüngeren PatientInnen im Vergleich zu Älteren (p < 0,01). NichtglaukompatientInnen mit positiver Glaukomdiagnose im Bekanntenkreis hatten ein signifikant besseres Wissen (p < 0,01) als solche ohne Glaukomdiagnose im Bekanntenkreis.
Schlussfolgerungen
Selbstbetroffene hatten zwar ein besseres Wissen im Vergleich zu Nichtbetroffenen, jedoch war dieses Wissen immer noch sehr gering. Im Wissensvergleich jüngere PatientInnen zu älteren PatientInnen überraschte in unserer Studie das schlechtere Abschneiden der Älteren. Insgesamt verdeutlicht unsere Studie mit einer sehr hohen Fallzahl die Wissensdefizite von Glaukomerkrankten und besonders von Nichterkrankten zum Thema Glaukom in Wien.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glaucoma is a chronic and severe disease calling for consistent lifelong therapy. Adequate knowledge of the disease is a prerequisite for the patient’s compliance (which may be defined as consistent adherence to the doctor’s advice). This became evident in a study performed by Altangerel et al. [1] in Philadelphia, USA, which revealed that patients who were poorly informed about glaucoma underwent significantly fewer follow-up investigations.
Glaucoma is the most common cause of blindness throughout the world. In a study performed in Switzerland, Mansouri et al. [2] showed that comprehensive knowledge about glaucoma is important for the patient’s compliance and also helps to arrest the progression of the disease.
Nevertheless, the level of knowledge about glaucoma is poor, as many studies have shown. One investigation performed by Lau et al. [3] from Hong Kong revealed knowledge deficits about ophthalmological diseases even in developed countries: 22.9 % of the surveyed persons were able to describe the symptoms of cataract correctly, but only 10.2 % were able to describe the symptoms of glaucoma correctly. The authors concluded that information campaigns should be conducted to provide more information and enhance the efficacy of health promotion, and thus avoid blindness.
According to a study performed by Hoevenaars et al. [4] in The Netherlands, the causes of ignorance about the disease were a low level of education, brief duration of the disease, advanced age, and the absence of access to the Internet. Besides, the study showed that patients preferably obtain information from their ophthalmologists, nurses, or glaucoma patient societies (self-help groups).
Mansouri’s study in Switzerland [5] confirmed that the ophthalmologist is the primary source of information for the patient.
A study performed by Mowatt et al. [6] in Jamaica disclosed the following reasons for poor compliance: financial resources, forgetfulness, and indifference.
In China, Chen et al. [7] showed better drug compliance due to significantly greater knowledge of the disease among members of a self-help group.
In an investigation performed in New Zealand, Danesh-Meyer et al. [8] reported that patients with glaucoma of long duration were just slightly better informed about the disease than patients with newly diagnosed glaucoma: 80 % of the study participants believed that local medication causes no systemic side effects, while 48 % of the long-term glaucoma patients believed that symptoms of the disease are signs of impending disease progression.
One-third of patients with newly diagnosed glaucoma believed that blindness is a part of the usual course of the disease.
As shown in many studies, glaucoma patients are not optimally informed about their disease. Therefore, the aim of the present study was to determine the level of knowledge about glaucoma on comparison of young patients with old ones and glaucoma patients with nonglaucoma ones.
Patients, material, and method
A total of 1110 questionnaires were distributed in the waiting room at the outpatient eye clinic of the Hietzing Hospital. The questionnaires were filled and returned by 1041 patients or their relatives. Figure 1 shows an example of a questionnaire.
The study population consisted of patients as well as family members and accompanying persons aged 18 years and older.
The questionnaire comprised 18 questions: 3 questions concerned the respondent, while 15 concerned glaucoma. Participation in the study was voluntary.
Patients were divided into two age-groups. Group 1 consisted of those aged 18–60 years, while group 2 consisted of those older than 61 years.
We compared the knowledge of patients, glaucoma patients in the respondents’ circle of friends or family, and nonglaucoma patients. The respondents’ knowledge was divided as shown in Table 1.
SPSS was used for data analysis. Depending on the distribution of data, a t-test or a Mann–Whitney U-test was used to determine significance. The level of significance was set to p < 0.05.
Results
Questionnaires were returned by 1041 persons. Of them, 100 questionnaires in which the question “Do you have glaucoma (glaucoma, raised intraocular pressure)” was left blank were excluded from analysis. Thus, 941 questionnaires were evaluated. Unanswered questions were deemed false.
The majority of the respondents were older than 60 years (72.8 %). A very small percentage of patients (3.4 %) were between 18 and 30 years of age. Figure 2 shows the age distribution of the study population.
Of the 941 surveyed patients, 480 (51 %) had glaucoma. The results revealed a nearly identical ratio with regard to a positive diagnosis of glaucoma in the respondents’ circle of friends: of the 941 respondents, 488 patients (51.9 %) had friends with a confirmed diagnosis of glaucoma.
Overall knowledge in relation to age
Compared with older patients, younger patients had significantly (p < 0.01) better knowledge of the disease. The details are shown in Table 2.
Of 941 patients, 3 failed to mention their age and were therefore excluded from the analysis. Thus, the baseline population comprised 938 patients. Only 1 of the 938 patients was very well informed about the disease. The large majority had “moderate knowledge,” followed by “poor knowledge” of the disease. Table 2 shows the overall knowledge of the subjects in relation to their age.
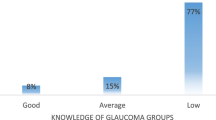
Knowledge of glaucoma patients and nonglaucoma patients
Glaucoma patients were significantly better informed (p < 0.01) than nonglaucoma patients. Table 3 shows the distribution.
Nonglaucoma patients with a confirmed diagnosis of glaucoma in their circle of friends or family compared with nonglaucoma patients with no confirmed diagnosis of glaucoma in their circle of friends
The large majority (329 subjects; 71.37 %) of nonglaucoma patients had no glaucoma among their circle of friends or family, while a mere 132 (28.63 %) reported friends with glaucoma.
Nonglaucoma patients with confirmed glaucoma among their circle of friends or family were significantly better informed (p < 0.01) about the disease than those with no glaucoma among their circle of friends or family (Table 4).
Evaluation of individual questions
Question 1:
The correct “definition of glaucoma” was provided by 75.7 % of patients with the disease, but by only 24.3 % of nonglaucoma patients; the difference was statistically significant (p < 0.01).
Table 5 shows the distribution of glaucoma patients and nonglaucoma patients who answered the question correctly.
Question 7:
A total of 65.6 % of glaucoma patients were able to estimate the risk of blindness correctly, but only 20.3 % of nonglaucoma patients were able to do so (p < 0.01).
Table 6 shows the distribution of glaucoma patients and nonglaucoma patients who answered the question correctly.
Question 12:
A total of 69.2 % of glaucoma patients knew that the measurement of their intraocular pressure was a part of their standard investigation at the ophthalmologist’s office, whereas only 18.2 % of nonglaucoma patients were aware of the fact (p < 0.01).
Table 7 shows the distribution of glaucoma patients and nonglaucoma patients who answered the question correctly.
Question 13:
A total of 60.2 % of glaucoma patients, but only 23.6 % of nonglaucoma patients, were aware of the association between glaucoma and age (p < 0.01).
Table 8 shows the distribution of glaucoma patients and nonglaucoma patients who answered the question correctly.
Discussion
Knowledge of glaucoma
In the present study, only 1 of 943 study participants was very well informed about glaucoma, 416 (44.1 %) of the respondents had moderate knowledge of the disease, and the large majority of 473 (50.2 %) were poorly or very poorly informed about the disease (in our study, 50 % of patients had glaucoma).
Mansouri et al.’s investigation in Switzerland [5], which consisted of 502 telephone interviews with a questionnaire comprising 40 questions, also revealed poor knowledge of glaucoma. A respondent’s definition of glaucoma was deemed positive when the respondent had either “heard about it” or provided a correct association when asked about the definition of the term. Only 24.7 % were able to classify glaucoma as an eye disease. Women were able to do so more frequently (26 %) than men (14 %).
In the aforementioned report [5], a few other studies concerning knowledge of glaucoma were compared. The percentage of respondents with knowledge of glaucoma varied markedly in developed countries: from 51 % in Germany, 72 % in the United States to 93 % in Australia [9–11]. In fact, Singapore fared much worse (23 %), while the same was true for India (2.3 %) [12, 13]. Similar results were shown in further studies: England (80 %), Greece (49 %), Nepal (2.4 %) [14–16].
Chen et al. [7] compared knowledge in the “general population” to the knowledge of patients who were members of a glaucoma club in Shanghai. Club members were aware of the course of glaucoma and the characteristics of the disease to a significantly greater extent than the normal population, and also led more healthy lives. Questions about types of glaucoma were answered correctly by 93 % of the glaucoma club members, but by a mere 63 % of the normal population. The correct answer about visual field investigations, which confirms the progression of disease, was provided by 61 % of club members and just 38 % of the normal population.
Knowledge about glaucoma has been defined diversely in various studies, which makes it difficult to compare these with the present study.
Lau et al.’s study [3] in Hong Kong, which also comprised a large number of patients (2538), revealed poor knowledge of glaucoma in Hong Kong: only 10.2 % were able to describe the symptoms of glaucoma correctly. This is in contrast to our study, in which at least 75.7 % of glaucoma patients and 24.3 % of nonglaucoma patients were able to define the disease correctly.
The poorer knowledge of glaucoma registered in the Hong Kong study may have been due to the nature of interrogation: the respondents were questioned verbally by the interviewers. Besides, the respondents were derived from “a random sample of addresses.” In our study, we employed written questionnaires with answers that could be crossed “right” or “wrong.” The questionnaires were distributed at the registration counter of the outpatient eye department. Besides, the aforementioned study showed that younger patients with better education and higher incomes were more likely to be informed about the definition of glaucoma.
The fact that education plays a role was also noted by Hoevenaars JG et al. [17] and Altangerel et al. [1] in Philadelphia, USA. An interesting detail of this study was that the poor results (only 29 % could define glaucoma correctly) were not related to the absence of insurance, lack of access to doctors, or transportation problems. The cited reasons were lack of interest, lack of confidence in the results of the study, and forgetfulness.
Mowatt et al.’s study conducted in Jamaica [6] is interesting in this regard. The authors noted the following reasons for poor compliance: 44 % of the respondents mentioned financial reasons, 20 % reported forgetfulness, and 12 % mentioned lack of confidence in the effect of eye drops.
In our study glaucoma patients were better informed about the disease than nonglaucoma patients, but their knowledge was still very poor. Among glaucoma patients, only 45 of 482 patients (9.3 %) had good or extensive knowledge. This was true for just 10 (2.3 %) of 444 nonglaucoma patients.
Comparison of nonglaucoma patients to those with glaucoma in their circle of friends or family revealed that the latter group was better informed about the disease, but their knowledge was still very poor. Among those with confirmed glaucoma among their circle of friends or family (454), 39 (8.6 %) had good or excellent knowledge of the disease, whereas this was true for just 16 (3.5 %) members of the reference group.
In agreement with our investigation, Danesh-Meyer et al.’s study in New Zealand [8] and Landers JA et al.'s study in Australia [18] showed that patients with glaucoma among friends or family members were better informed about the disease.
Surprisingly, in our study, younger patients (18–60 years of age) were better informed about glaucoma than older ones (older than 60 years). In fact, younger patients had significantly better knowledge of the disease (p < 0.01). In all, 43 % of younger patients had very poor or poor knowledge of glaucoma (128 of 298), whereas this was true for 53.5 % of older patients (345 of 645). Also, 7.4 % of younger patients had good or excellent knowledge about glaucoma, but this was true for just 5 % of the older ones.
Danesh-Meyer et al.’s investigation [8], which was also a questionnaire study (right/wrong; the patient population consisted of 408 persons), showed that long-term glaucoma patients (mean age, 72 years) were significantly better informed about the disease than newly diagnosed glaucoma patients (mean age, 61 years). Both groups were significantly better informed than controls (nonglaucoma patients; mean age, 61 years).
In Mowatt et al.’s study in Jamaica [6], compliance rates were much higher in older patients (61–80 years; compliance rate, 47.3 %) than among younger ones (age-group 21–40 years; compliance rate, 33.3 %). Besides, the authors of the study investigated compliance in relation to knowledge levels (100 patients were interviewed at home): 47 % had attended a glaucoma clinic for more than 10 years (in fact, 14 % for more than 20 years). Also, 85 % were aware of their diagnosis, but only 22 % understood it fully (33 % understood it partly, while 45 % had no idea what it meant).
A total of 50 % reported full compliance (they followed all therapy instructions), 43 % reported partial compliance (they forgot to take their medication once a week or more often), while 7 % reported noncompliance (no glaucoma therapy was used as prescribed). Patients who were not well informed about glaucoma tended to be noncompliant. Women were more compliant (69.4 %) than men (30.6 %). Compliance between the 5th and 10th year of treatment was better than it was in the first 5 years and after the 10th year.
However, despite a few reports postulating that better knowledge of the disease may be equated with better compliance, this fact cannot be stated with certainty.
Hoevenaars et al.’s study in The Netherlands reported interesting data about compliance [19]. In contrast to other studies, the authors found no significant correlation between knowledge levels and compliance. The investigation was a questionnaire study (166 patients) comprising 22 questions to be crossed (yes/no/don’t know); 27.3 % (42 of 154) of patients were noncompliant (noncompliant was defined as forgetting to use one or more eye drops in the preceding 3 weeks). The authors of the study and the Author's reply [19, 20] concluded that further improvement of knowledge levels was unlikely to improve the patients’ compliance with glaucoma treatment to a marked extent.
Awareness of the severity of disease may be an important factor. Contact with other experienced glaucoma patients may lead to higher compliance rates.
Some articles have reported a correlation between knowledge of glaucoma and better compliance [21–28]. A highly motivated and concerned patient need not necessarily be a well-informed one. However, imparting discipline and a favorable basic attitude could improve therapy compliance.
In a meta-analysis from The Netherlands [19], 50 % of the reviewed publications reported a noncompliance rate of more than 29 % [21, 22, 29–32].
One limitation of our study is the absence of questions concerning the duration of glaucoma, compliance data, and accompanying diseases. However, it may be assumed that the results were markedly different from those of other European studies mentioned earlier in the text.
Basic rudimentary knowledge of the disease is absolutely essential to understand the importance of regular controls and the treatment of the disease. This was confirmed by Mansouri et al. [2] in a study conducted in Switzerland; the authors state that a high level of knowledge enhances compliance.
In general, our study—comprising a large number of cases—disclosed a knowledge deficit about glaucoma among patients with the disease and especially nonglaucoma patients in Vienna.
Information provided directly by the treating ophthalmologist, information campaigns (shown in the study of Mohamed EA et al. [33]), and also joining self-help groups should help patients to be better informed about the disease and conscientiously undergo regular controls as well as therapy.
Possibly, patient booklets providing simple and comprehensible answers to the most important questions would be very suitable for informing patients. However, data concerning this aspect are not available yet.
Further limitations of the present study include the absence of questions concerning the respondents’ educational level, social status, gender, family history, general medical history, mother tongue, and ethnic origin. Information about these aspects may provide valuable additional data and further important starting points for the prevention of avertable blindness.
It would also be interesting to include, in a future study, a control group derived from the average population outside the hospital.
Vote of the ethics committee
The ethics committee issued a written statement to the effect that no appraisal of the ethics committee is required for the study.
Conflict of interest
The authors declare no conflict of interests.
References
Altangerel U, Nallamshetty HS, Uhler TK, et al. Knowledge about glaucoma and barriers to follow-up care in a community glaucoma screening program. Can J Ophthalmol. 2009;44(1):66–9.
Mansouri K, Iliev ME, Rohrer K, Shaarawy T. Compliance and knowledge about glaucoma in patients at tertiary glaucoma units. Int Ophthalmol. 2011;31(5):369–76.
Lau JT, Lee V, Fan D, Lau M, Michon J. Knowledge about cataract, glaucoma, and age related macular degeneration in the Hong Kong Chinese population. Br J Ophthalmol. 2002;86(10):1080–4.
Hoevenaars JG, Schouten JS, van den Borne B, Beckers HJ, Webers CA. Knowledge base and preferred methods of obtaining knowledge of glaucoma patients. Eur J Ophthalmol. 2005;15(1):32–40.
Mansouri K, Orgül S, Meier-Gibbons F, Mermoud A. Awareness about glaucoma and related eye health attitudes in Switzerland: a survey of the general public. Ophthalmologica. 2006;220(2):101–8.
Mowatt L, Nelson-Imoru J, Gordon-Strachan G. Glaucoma medication compliance issues in a Jamaican hospital eye clinic. West Indian Med J. 2011;60(5):541–7.
Chen X, Chen Y, Sun X. Notable role of glaucoma club on patients’ knowledge of glaucoma. Clin Experiment Ophthalmol. 2009;37(6):590–4.
Danesh-Meyer HV, Deva NC, Slight C, et al. What do people with glaucoma know about their condition? A comparative cross-sectional incidence and prevalence survey. Clin Experiment Ophthalmol. 2008;36(1):13–8.
Pfeiffer N, Krieglstein GK, Wellek S. Knowledge about glaucoma in the unselected populations: a German survey. J Glaucoma. 2002;11(5):458–63.
Gasch AT, Wang P, Pasquale LR. Determinants of glaucoma awareness in a general eye clinic. Ophthalmology. 2000;107(2):303–8.
Mitchell P, Smith W, Attebo K, et al. Prevalence of open angle glaucoma in Australia: the blue mountains eye study. Ophthalmology. 1996;103:1661–9.
Saw S-M, Gazzard G, Friedman D, et al. Awareness of glaucoma, and health beliefs of patients suffering primary acute angle closure. Br J Ophthalmol. 2003;87(4):446–9.
Dandona R, Dandona L, John RK, et al. Awareness of eye diseases in an urban population in southern India. Bull World Health Organ. 2001;79(2):96–102.
Baker H, Cousens SN, Murdoch IE. Poor public health knowledge about glaucoma: fact or fiction? Eye (Lond). 2010;24(4):653–7.
Konstas AG, Maskaleris G, Gratsonidis S, Sardelli C. Compliance and viewpoint of glaucoma patients in Greece. Eye (Lond). 2000;14(Pt. 5):752–6.
Thapa SS, Berg RV, Khanal S, et al. Prevalence of visual impairment, cataract surgery and awareness of cataract and glaucoma in Bhaktapur district of Nepal: the Bhaktapur Glaucoma Study. BMC Ophthalmol. 2011;11:2.
Hoevenaars JG, Schouten JS, van den Borne B, Beckers HJ, Webers CA. Socioeconomic differences in glaucoma patients’ knowledge, need for information and expectations of treatments. Acta Ophthalmol Scand. 2006;84(1):84–91.
Landers JA, Goldberg I, Graham SL. Factors affecting awareness and knowledge of glaucoma among patients presenting to an urban emergency department. Clin Experiment Ohthalmol. 2002;30(2):104–9.
Hoevenaars, JG, Schouten JS, van den Borne B, Beckers HJ, Webers CA. Will improvement of knowledge lead to improvement of compliance with glaucoma medication? Acta Ophthalmol. 2008;86(8):849–55.
Hoevenaars JG, Schouten JS, van den Borne B, Beckers HJ, Webers CA. Will Improvement of knowledge lead to improvement of compliance with glaucoma medication? Authors’ reply. Acta Ophthalmol. 2009;87(4):468–9. Author reply 469–71.
Spaeth GL. Visual loss in a glaucoma clinic. Invest Ophthalmol. 1970;9(1):73–82
Vincent PA. Patients’ viewpoint of glaucoma therapy. Sight Sav Rev. 1972;42(4):213–21.
Bloch S, Rosenthal AR, Friedman DS, Caldarolla P. Patient compliance in glaucoma. Br J Ophthalmol. 1977;61(8):531–4.
MacKean JM, Elkington AR. Compliance with treatment of patients with chronic open-angle glaucoma. Br J Ophthalmol. 1983;67(1):46–9.
Amon M, Menapace R, Wedrich A, Radax U. Aspekte der Betreuung von Glaukompatienten und deren Auswirkung auf die Compliance (Aspects of glaucoma patient care and its impact on compliance). Spektrum Augenheilkunde. 1990;4:5–8.
Olthoff CMG, Schouten JSAG, Van de Borne BW, Webers CAB. Noncompliance with ocular hypotensive treatment in patients with glaucoma or ocular hypertension. Ophthalmology. 2005;112:953–61.
Chawla A, McGalliard J, Batterbury M. Use of eyedrops in glaucoma: how can we help to reduce non-compliance? Acta Ophthalmol Scand. 2007;85(4):464.
Mansouri K, Shaarawy T. Will improvement of knowledge lead to improvement of compliance with glaucoma medication? Acta Ophthalmol. 2009;87:468–9.
Rotchford AP, Murphy KM. Compliance with timolol treatment in glaucoma. Eye (Lond). 1998;12(Pt. 2):234–6.
Pecori Giraldi J, Liguori A, Mollicone A, Paone E. Compliance and psychological conditions: a long-term investigation in 245 glaucomatous patients. Acta Ophthalmol Scand. 1999;77(Suppl. 229):66–7.
Tsai JC, McClure CA, Ramos SE, Schlundt DG, Pichert JW. Compliance barriers in glaucoma: a systematic classification. J Glaucoma. 2003;12(5):393–8.
Deokule S, Sadiq S, Shah S. Chronic open angle glaucoma: patient awareness of the nature of the disease, topical medication, compliance and the prevalence of systemic symptoms. Ophthalmic Physiol Opt. 2004;24(1):9–15.
Mohamed EA, Bayoumi OR, Draz SF. Impact of an educational programme on knowledge, beliefs, practices and expectations about care among adolescent glaucoma patients in Cairo. East Mediterr Health J. 2011;17(12):960–8.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fabjani, S., Richter-Müksch, S., Cakmak, N. et al. Level of knowledge about glaucoma in Vienna. Wien Klin Wochenschr 127, 612–618 (2015). https://doi.org/10.1007/s00508-014-0687-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-014-0687-1