Summary
Background
Histamine intolerance (HIT) is characterized by an imbalance between histamine intake and the capacity for histamine degradation. The main enzyme for metabolizing ingested histamine is diamine oxidase (DAO). Determining DAO activity in serum may be useful in diagnosing HIT.
Methods
Over a period of 3.5 years we recruited 316 subjects with clinically suspected HIT and 55 healthy controls. Serum DAO activity was measured with a quantitative enzyme immunoassay. Twenty patients with highly reduced DAO activity went on a histamine-free diet for 6–12 months. Afterwards, their DAO activity was determined again.
Results
We found that DAO activity was significantly lower in patients than in healthy control subjects (P < 0.0001). Furthermore, 54 patients had highly reduced serum DAO activity (< 40 HDU/ml). Their main symptoms involved the skin, gastrointestinal tract, respiratory system, and eyes. In all the 20 patients with highly reduced DAO activity, the main clinical symptoms typical of histamine intolerance disappeared after they adopted a histamine-free diet. Furthermore, the serum DAO activity values measured increased significantly (P < 0.0001).
Conclusions
Our results suggest that determining DAO activity in serum is a useful tool in diagnosing HIT. Furthermore, our results showed the benefit of a histamine-free diet because after the diet the majority of symptoms disappeared and the serum DAO activity significantly increased.
Zusammenfassung
Einleitung
Die Histaminintoleranz (HIT) ist ein Ungleichgewicht zwischen aufgenommenen Histamin und Histaminabbau. Das wichtigste Enzym für den Abbau von aufgenommenen Histamin ist Diaminooxidase (DAO). Die Bestimmung der Aktivität von DAO vermag sich als hilfreich erweisen bei der HIT-Diagnose.
Methoden
Über einen Zeitraum von 3,5 Jahre haben wir 316 Probanden mit klinischem HIT-Verdacht und 55 gesunde Versuchspersonen angeworben. Die Aktivität von DAO im Serum wurde per Enzymimmunoassay quantitiv bestimmt. Zwanzig Patienten mit einer stark reduzierten DAO-Aktivität wurden auf eine histaminfreie Diät gesetzt über einen Zeitraum von 6 bis 12 Monaten. Danach wurde deren DAO-Aktivität erneut gemessen.
Ergebnisse
Wir haben festgestellt, dass die DAO-Aktivität in diesen Patienten signifikant niedriger war als in den gesunden Versuchspersonen (P < 0,0001). Desweiteren hatten 54 Patienten eine stark reduzierte DAO-Aktivität im Serum (< 40 HDU/ml). Deren Hauptsymtome betrafen die Haut, den Magen-Darm-Trakt, die Atemwege und Augen. In allen 20 Patienten mit stark reduzierter DAO-Aktivität verschwanden die typischen klinischen Symptome bei Histaminintoleranz nach Durchführung der histaminfreien Diät. Zudem stieg DAO-Aktivität im Serum signifikant an (P < 0,0001).
Ergebnisse
Unsere Ergebnisse lassen darauf schließen, dass die Bestimmung der Aktivität von Diaminooxidase in Serum dienlich ist als Diagnostiktest auf HIT Desweiteren zeigen unsere Ergebnisse die Vorteile einer histaminfreien Diät, da die Mehrheit der Symptome verschwunden sind während die DAO-Aktivität im Serum signifikant anstieg.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
- HIT:
-
Histamine intolerance
- DAO:
-
Diamine oxidase
- HIT:
-
Histaminintoleranz
- DAO:
-
Diaminooxidase
Introduction
Histamine intolerance (HIT) is mainly caused by ingestion of food containing high amounts of histamine by people with low intestinal histamine inactivation and degradation or inhibition of this activity by other food constituents or drugs. This leads to resorption of histamine, a biogenic amine, in amounts sufficient to cause adverse reactions [1–5]. The main enzyme for inactivating and metabolizing ingested histamine is diamine oxidase (DAO). DAO is a secretory enzyme that acts extracellularly to oxidatively deaminate the primary amino group of histamine yielding imidazole acetaldehyde [2, 5]. Impaired histamine degradation based on reduced DAO activity and the resulting excess in histamine may cause a variety of symptoms, including gastrointestinal discomfort associated with vomiting or diarrhea, abdominal pain, headache, urticaria, rhinitis, pruritus, flushing, asthma-like symptoms, cardiovascular complaints such as hypotension and tachycardia, and other conditions, often mimicking an allergic reaction [1–6].
HIT symptoms are mainly provoked by foods with high amounts of histamine, such as alcoholic beverages (especially red wine and champagne), cheese (especially aged), meat (especially cured), and fish. In addition, many foods, such as citrus fruits and nuts, have the ability to release histamine from tissue mast cells. Besides, because of high histamine intake, DAO-blocking drugs or drugs that release histamine such as contrast media, muscle relaxants, narcotics, analgesics, local anesthetics, diuretics, antibiotics, and so on can be causative agents for HIT [1–4].
Due to the multifaceted symptoms and multiple organs involved, the existence of HIT is frequently underestimated, or its symptoms are misinterpreted [3, 4]. Approximately 1–3 % of the population has HIT, and the majority (80 %) of these people are middle-aged [3].
HIT is commonly diagnosed based solely on subjective reporting of symptoms instead of following systematic diagnostic procedures based on objective laboratory and physical parameters [4, 5]. A diagnosis of HIT is made based on the presentation of at least two typical symptoms of HIT and improvement from using a histamine-free diet and antihistamines [1–5]. Although the gold standard in diagnosis is a double-blind, placebo-controlled histamine provocation after eating a histamine-free diet for 4 weeks, in a patient clinically suspected of having HIT, determination of DAO activity in serum might be useful for diagnosing HIT. There is some controversy regarding the usefulness of determining DAO activity [1, 3, 7–11].
Our study sets out to measure the serum DAO activity in patients with clinically suspected HIT and compare the results with healthy controls that have no histamine-related problems. Furthermore, in patients with highly reduced serum DAO activity, a prospective study was conducted. In this study, we addressed the effects of a histamine-free diet on clinical symptoms and serum DAO activity in histamine-intolerant patients, both before and after the diet.
Materials and methods
Study subjects
The study group consisted of 316 adult patients (median age 45 years; range 14–83 years; 207 female and 109 male) with suspected HIT and 55 healthy controls (median age 41 years; range 17–74 years; 37 female and 18 male) without any HIT symptoms (Table 1). This group was recruited at the Golnik University Clinic of Respiratory and Allergic Diseases over a period of 3.5 years, from January 2006 to May 2009. All patients recruited had been subject to the usual tests for food allergy (skin prick tests, specific IgE, and/or oral provocation tests) in order to exclude food allergy. Furthermore, all patients were regularly observed and information regarding clinical signs and symptoms of histamine effects were also recorded.
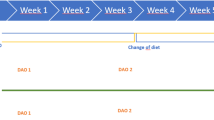
Of these patients, 20 with highly reduced initial serum DAO activity (< 40 HDU/ml) were selected. Those patients went on a histamine-free diet. After 6–12 months of this diet, all clinical parameters and serum for determination of DAO activity were taken again.
Determination of histamine-degradation activity by diamine oxidase (DAO)
Serum DAO activity was measured with enzyme immunoassay for the quantitative determination of histamine-degradation activity by DiAmineOxidase (DAO) in serum and EDTA-plasma (D-HIT, Sciotec, Austria) in accordance with the manufacturer’s instructions. We used the manufacturer’s recommended reference values: normal activity of DAO > 80 HDU/ml, reduced activity of DAO 40–80 HDU/ml, and highly reduced activity of DAO < 40 HDU/ml, for evaluation. One HDU (histamine degrading unit) corresponds to the DAO activity that degrades 1 pmol/ml (0.11 ng/ml) of histamine.
Statistical analyses
Data distribution was recalculated using the Shapiro-Wilk test. As the data were not normally distributed, we performed a Mann-Whitney test and/or Wilcoxon test. Probability values of P < 0.05 were accepted as significant. Analyses were performed with GraphPad Prism 5.
Results
We found that DAO activity was significantly lower in patients than in healthy control subjects (P < 0.0001, Mann-Whitney test) as seen in Fig. 1. Moreover, 199 of 316 (63 %) patients had reduced DAO activity according to the manufacturer’s reference values (< 80 HDU/ml) in comparison to only 12 of 55 (22 %) control subjects. Furthermore, 54 (17 %) patients, but no healthy control subject, had highly reduced DAO activity ( < 40 HDU/ml) (Fig. 2). The main symptoms in patients with highly reduced serum DAO activity involved the skin in 83 % (urticaria, angioedema, pruritus, and erythema), the gastrointestinal tract in 52 % (tenesmus, diarrhea, oral itching, abdominal pain, vomiting, constipation, and burping), the respiratory system in 26 % (cough, bronchospasm, rhinitis, hoarseness, and sinusitis), and the eyes in 9 %. Other symptoms (in 6 % of cases) were headache, conjunctivitis, hot flashes, aphthae, swollen joints, and paresthesia in the hands. The main causes of symptoms were fruits such as citrus fruits and strawberries, animal foods such as meat and fish, alcoholic beverages such as wine and beer, cheese, chocolate, and additives and spices.
We selected 20 patients with highly reduced initial serum DAO activity (< 40 HDU/ml). These patients went on a histamine-free diet (avoidance of histamine-containing food, histamine-releasing substances, and substances that inhibit DAO) and after 6–12 months of the diet all clinical parameters and the serum for determination of DAO activity were taken again. In all the 20 patients the main clinical symptoms typical of HIT had disappeared or at least were highly diminished. Furthermore, in all patients the measured values for serum DAO activity increased significantly following the histamine-free diet (P < 0.0001) above the levels for highly reduced activity based on the reference values (< 40 HDU/ml) (Fig. 3). In patients who reported diet errors, symptoms reappeared after the intake of food and beverages with high histamine content, such as wine, beer, aged cheese, salami, and chocolate.
Discussion
The major problems in diagnosing HIT is the lack of in vitro diagnostic tests and highly variable and heterogeneous symptoms after the intake of histamine-rich food, alcoholic beverages, or histamine-releasing or DAO-blocking drugs [2, 3, 5, 6]. Definitive diagnosis necessitates double-blind, placebo-controlled oral histamine provocation with determination of plasma histamine concentrations and objective physical parameters [3, 5, 6]. However, the interpretation of provocation results is often difficult because of lack of symptom reproducibility [6, 12]. Furthermore, even otherwise healthy subjects may respond to a standard histamine provocation using 75 mg liquid histamine [13]. Therefore, the need for an objective diagnostic test is more than evident. In cases of confirmed HIT, a histamine-free diet represents an effective treatment and should be advised [3, 5]. The role of DAO activity in serum as well as its use as a diagnostic tool has been addressed several times, frequently with contradictory results and conclusions [3, 7–11]. Some authors still deny the role of DAO in HIT despite clinical symptoms, excluded allergy, and lower DAO activity [10, 11].
In our study, we analyzed the results from 316 cases with clinical signs of HIT recruited at our hospital over a period of 3.5 years. Our results show that the determination of serum DAO activity is a useful tool in HIT diagnosis, especially in patients with highly reduced DAO activity. Detailed case histories, negative allergy tests (exclusion of food allergy), and reduced serum DAO activity made it possible to diagnose HIT. Moreover, DAO activity in patients was much lower than in healthy controls, and the patients with highly reduced DAO activity had several typical symptoms of HIT after the intake of histamine-rich food. The main clinical symptoms involved the skin, gastrointestinal system, respiratory system, and eyes.
Therapy for HIT is mainly based on a histamine-free diet [2–4, 9, 14]. The patients with highly reduced DAO activity were put on a histamine-free diet and after the diet the majority of symptoms disappeared and the included patients’ quality of life significantly improved, confirming the usefulness of diet therapy in addition to supporting the diagnosis of HIT along with the involvement of DAO in it. Furthermore, DAO activity increased in all patients on the diet. These findings are consistent with those of another study in which an increase of DAO activity along with a reduction in symptoms was observed in migraine patients following a histamine-free diet [9]. The role of a histamine-free diet in DAO activity conforms with the idea that jejunal DAO is relieved with lower histamine intake, which indirectly activates the enzyme and results in more histamine being effectively eliminated [9, 15].
Based on our observations, we can conclude that determination of serum DAO activity is a useful diagnostic tool, along with a detailed history, for diagnosing HIT. It should be performed in patients suspected of having HIT with symptoms such as headache, tachycardia, urticaria, pruritus, diarrhea, and hypotension. Furthermore, our results showed the benefit of a histamine-free diet because after following the diet the majority of histamine-related symptoms disappeared and the serum DAO activity increased.
References
Jarisch R. Histamin-Intoleranz [Histamine intolerance]. Aerztemagazin. 2004;8:1–4.
Maintz L, Bieber T, Novak N. Histamine intolerance in clinical practice. Dtsch Arttebl. 2006;103(102–103):3477–83.
Maintz L, Novak N. Histamine and histamine intolerance. Am J Clin Nutr. 2007;85:1185–96.
Schwelberger HG. Histamine intolerance: overestimated or underestimated? Inflamm Res. 2009;58(S1):51–2.
Schwelberger HG. Histamine intolerance: a metabolic disease? Inflamm Res. 2010;59(S2):219–21.
Komericki P, Klein G, Reider N, Hawranek T, Strimitzer T, Lang R, Kranzelbinder B, Aberer W. Histamine intolerance: lack of reproducibility of single symptoms by oral provocation with histamine: a randomized, double-blind, placebo-controlled cross-over study. Wien Klin Wochenschr. 2011;123(1–2):15–20.
Tufvesson G, Tryding N. Determination of diamine oxidase activity in normal human blood serum. Scand J Clin Lab Invest. 1969;24:163–8.
Mayer I, Missbichler A, Wantke F, Focke M, Reichl H, Winter M, Jarisch R. Optimierter Radioextraktionsassay zur quantitativen Bestimmung der Aktivität von Diaminooxidase (DAO) in humanem Serum und Plasma [Optimized radioextraction assay for the quantitative measurement of the activity of diamine oxidase (DAO) in human serum and plasma]. Allergologie. 2005;28:1–8.
Steinbrecher I, Jarisch R. Histamin und Kopfschmerz [Histamine and headache]. Allergologie. 2005;28:84–91.
Töndury B, Wüthrich B, Schmid-Grendelmeier P, Seifert B, Ballmer-Weber BK. Histaminintoleranz: Wie sinnvoll ist die Bestimmung der Diaminoxidase-Aktivität im Serum in der alltäglichen klinischen Praxis? [Histamine intolerance: is the determination of diamine oxidase activity in the serum useful in routine clinical practice?]. Allergologie. 2008;31:350–6.
Kofler H, Aberer W, Deibi M, Hawranek T, Kleih G, Reider N, Fellner N. Diamine oxidase (DAO) serum activity: not a useful marker for diagnosis of histamine intolerance. Allergologie. 2009;32:105–9.
Kanny G, Gerbaux V, Olszewski A, Fremont S, Empereur F, Nabet F, Cabanis JC, Moneret-Vautrin DA. No correlation between wine intolerance and histamine content of wine. J Allergy Clin Immunol. 2001;107:375–8.
Wöhrl S, Hemmer W, Focke M, Rappersberger K, Jarisch R. Histamine intolerance-like symptoms in healthy volunteers after oral provocation with liquid histamine. Allergy Asthma Proc. 2004;25:305–11.
Stolze I, Peters KP, Herbst RA. Histaminintoleranz imitiert Anorexia nervosa [Histamine intolerance mimics anorexia nervosa]. Hautarzt. 2010;6:776–8.
Wantke F, Götz M, Jarisch R. Die histaminfreie Diät [The histamine-free diet]. Hautarzt. 1993;44:512–6.
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mušič, E., Korošec, P., Šilar, M. et al. Serum diamine oxidase activity as a diagnostic test for histamine intolerance. Wien Klin Wochenschr 125, 239–243 (2013). https://doi.org/10.1007/s00508-013-0354-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-013-0354-y