Summary
Objective
The purpose of this study was to investigate recent epidemiological trends of myasthenia gravis (MG) in Austria.
Methods
We used the national hospital discharge register, which records the discharge diagnoses of all inpatient stays in Austria to calculate the yearly inpatient prevalence of MG from 1992 to 2009 (main or secondary diagnosis of MG). The population prevalence was indirectly estimated. The temporal and geographical variability of the inpatient prevalence was correlated with the number of practicing neurologists.
Results
The inpatient prevalence of 2009 was calculated as 8.0 and the population prevalence as 15.69 (95 % CI 13.16–19.42) per 100,000. We observed a 2.2 fold increase in the inpatient prevalence between 1992 and 2009, which was mainly due to a rise in the number of older patients (³ 50 years). Partly this could be accounted for by an ageing of the population as a whole and a rise in the age of hospitalised patients. However, after adjusting for demographic factors an unexplained average yearly rise of 3.7–3.9 % remained. We found a significant spatial and temporal correlation of MG inpatient prevalence rates with the number of practicing neurologists, which increased over the same period.
Conclusions
The results from this study support the notion that the prevalence rate of MG in Austria is rising and near the higher end of the wide range discussed in the literature. Our data argue for the importance of specialist neurological care for the diagnosis of this disease.
Zusammenfassung
Hintergrund
Das Ziel der vorliegenden Studie war es, rezente epidemiologische Entwicklungen der Myasthenia gravis (MG) in Österreich zu untersuchen.
Methodik
Im Rahmen des Systems der leistungsorientierten Krankenanstaltenfinanzierung (LKF) werden die Entlassungsdiagnosen aller in Österreich hospitalisierten Patienten in einem zentralen, nationalen Register gesammelt. Mithilfe dieses Registers wurde die jährliche Prävalenz aller stationär aufgenommenen Patienten mit der ICD-Haupt- oder -Nebendiagnose „Myasthenia gravis“ zwischen 1992 und 2009 berechnet (Hospitalisationsprävalenz). Die Gesamtprävalenz der MG in der Bevölkerung wurde aus diesen Zahlen indirekt geschätzt. Weiters wurde die Hospitalisationsprävalenz, zeitlich und nach Regionen gegliedert, mit der jeweiligen Zahl der praktizierenden Neurologen korreliert.
Ergebnisse
Die Hospitalisationsprävalenz im Jahr 2009 betrug 8,0 pro 100.000 Wohnbevölkerung und die Prävalenz in der Gesamtbevölkerung 15,69 (95 % CI 13,16–19,42) pro 100.000 Wohnbevölkerung. Wir beobachteten einen 2,2-fachen Anstieg der Hospitalisationsprävalenz zwischen 1992 und 2009. Zum Teil war dieser Trend durch eine Zunahme bei den älteren Patienten (³ 50 Jahre) zu erklären, hauptsächlich bedingt durch den steigenden Altersdurchschnitt in der Gesamtbevölkerung und in der Gruppe aller stationären Patienten. Eine Komponente dieses Trends war jedoch nicht durch allgemeine demographische Faktoren zu erklären, da nach deren Korrektur immer noch ein jährlicher Anstieg der Prävalenz von 3,7 bis 3,9 % festzustellen war. Wir beobachteten eine signifikante, zeitliche und geographische Korrelation der MG-Prävalenz mit der Dichte der neurologischen Versorgung.
Schlussfolgerungen
Die MG-Prävalenz in Österreich ist ansteigend und im oberen Bereich der in der Literatur diskutierten Spannbreite gelegen. Unsere Ergebnisse legen die Wichtigkeit einer fachärztlich neurologischen Versorgung für die korrekte Diagnosestellung dieser Erkrankung nahe.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myasthenia gravis (MG) is a worldwide occurring autoimmune disease marked by a fluctuating muscle weakness due to an impaired neuromuscular transmission. It is further characterised by a pronounced clinical variability both between different patients and within individual patients during the course of the disease [1–3].
Numerous studies have investigated the epidemiology of MG over the years, but the resultant incidence and prevalence rates turned out to be highly heterogeneous [4, 5]. In recent epidemiological surveys the prevalence rates varied from 1.5 per 100,000 to 17.9 per 100,000 [5]. It remains unclear whether this primarily reflects methodological differences or true differences in disease frequencies based on ethnical or other demographic factors [6].
Another open epidemiological question concerns the causes for the rising frequency of MG over the last decades, which has been observed in several studies [7, 8]. Most authors have attributed this trend to the better medical diagnosis and enhanced survival [9], though this relationship has not been formally investigated.
To our knowledge no epidemiological studies have been performed on MG in Austria. To fill this gap we took advantage of the large national Austrian hospital discharge register (HDR), which reliably records the diagnoses of all inpatients in this country of over 8 million people. Using this database we evaluated several epidemiological parameters of MG, in particular we analysed the time trend of hospitalisations for this disease over a period of 18 years from 1992 to 2009 and correlated the results with demographic developments in this country.
Methods
Data source
The main data source of this study was the Austrian hospital discharge register (HDR) recording the discharge diagnoses of all inpatient stays in acute care hospitals, which are funded by the obligatory health insurance system. As the insurance coverage in Austria is over 99 %, nearly all hospital admissions are captured. Previous studies could show the accuracy and reliability of the Austrian HDR by comparing discharge data with other databases (e.g. Hepatitis C notification database) [10, 11].
The HDR does not include the names of the patients but their dates of birth, sex and residential districts (zip codes). After identification and exclusion of re-admissions and of non-residents the number of individual hospitalised patients within a given year and with a certain diagnosis can thus be extracted and assigned to residential districts. Between 1992 and 2000 the database was searched for ICD 9 code 358 (Myoneural disorders) and thereafter for ICD 10 code G70 (Myasthenia gravis and other myoneural disorders) to identify all myasthenia gravis patients (principal or secondary diagnosis). We note that in contrast to the ICD 10 code G70 the ICD 9 code 358 also includes the Lambert–Eaton myasthenic syndrome (LEMS). The usage of the ICD 9 code might have led to a marginal overestimation of the prevalence rates from 1992 to 2000 and therefore to a small underestimation of the increase in the prevalence rates in the single year from 2000 to 2001. However, as the prevalence of LEMS (approximately 3 per million) is only a fraction of that of MG the resulting errors can be considered negligible [12].
Population counts of Austria were downloaded from Statistics Austria (http://www.statistik.at/web_en/). The number of practicing neurologists for each year from 1990 was obtained from the Austrian Health Institute, which captures all doctors practising in Austria.
Calculation of the prevalence rates
From the HDR, we could extract the MG inpatient prevalence, i.e. all hospitalised MG patients in a certain year. We further retrospectively reviewed 100 myasthenia gravis outpatients of our department, who were suffering from the disease in 2009 to evaluate their hospitalisation rate, and thus evaluated the proportion of our patients being hospitalised (for whatever reason) in that year. Thus, extrapolating this hospitalisation rate to the overall population we could calculate the prevalence of MG in Austria by dividing the inpatient prevalence in 2009 by the hospitalisation rate. We note that this is likely to be an overestimation of the true hospitalisation rate in the total myasthenia gravis population as our sample may be biased towards a more severe disease course. However, on that assumption the overall prevalence of MG would be even higher. Furthermore, to account for general trends affecting Austrian society as a whole, we adjusted the inpatient prevalence rates for the ageing of the overall population and for possible changes in hospitalisation trends over time. Therefore, we expressed the inpatient prevalence in relation to 100,000 of the age adjusted reference population and in relation to 10,000 of the age adjusted hospital admissions.
Statistics
Pearson’s correlation coefficients (regional MG inpatient prevalence rates and density of neurologists) and p-values (two sided tests) were calculated using the statistical package SPSS v.18. Prevalence rates refer to 100,000 residential population per year unless otherwise stated.
Results
Inpatient prevalence of myasthenia gravis in Austria
From the Austrian hospital discharge register (HDR) we were able to extract all inpatient cases with a discharge diagnosis of myasthenia gravis (MG) from 1992 to 2009. For 2009 the register returned 669 unique inpatients with myasthenia gravis as their principal or secondary diagnosis. Given a residential population of 8,363,040 in Austria in 2009 the inpatient prevalence of myasthenia gravis can be calculated as 8.0 per 100,000.
This inpatient prevalence can be used to infer on the likely bounds of the population prevalence of MG. Clearly, not every patient with MG was hospitalised in 2009, thus the population prevalence must be higher than 8.0 per 100,000. To derive an estimation of the hospitalisation rate of MG patients, we surveyed 100 consecutive MG patients of our outpatients clinic on whether they were hospitalised (for any reason) in 2009 or not, which returned a hospitalised proportion of 0.51 (95 % CI 0.41–0.61). Applying that our sample may be biased towards a more severe disease course we estimate that the population prevalence of MG was at least 15.69 (95 % CI 13.16–19.42) per 100,000 in Austria in 2009.
Sex and age characteristics
The histogram (Fig. 1) shows the age and sex distribution of MG inpatients averaged for the years 2005 till 2009. These data are based on 3,284 cases. In women a bimodal distribution was clearly discernable with a broad peak between 30 and 55 years and a second peak above 60 years of age. In men the curve remained flat in the younger age range with a steep rise only after the age of 50 to parallel the female curve.
Age and sex distribution of hospitalised MG patients. The histogram shows the age distribution of hospitalised myasthenia gravis patients for women and men averaged for the years 2005–2009 (data points are mean values and error bars represent standard deviations). The data are based on 3,284 patients. In contrast to men women display a clear bimodal distribution
In this MG inpatient population (averaged over 5 years) the majority of patients (74.4 %) were older than 50 years, 22.4 % were aged between 15 and 49 years and only 3.2 % were younger than 15 years. There was a clear female preponderance in the younger adult age range (15–49 years, female-to-male ratio: 2.2–1.0) but a balanced distribution in the older age group and in children (female-to-male ratio for < 15 years: 1.0–1.0; for ³ 50 years: 0.9–1.0).
Increase of myasthenia gravis inpatient prevalence between 1992 and 2009
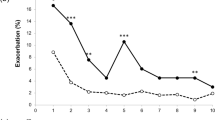
Over the 18 years between 1992 and 2009 there was a 2.2 fold increase in the prevalence of hospitalised MG patients from 3.63 per 100,000 in 1992–8.00 per 100,000 in 2009 (with an averaged 5.1 % rise per year). A closer look at the underlying age composition revealed that in absolute terms this increase was mainly due to the group of older patients (≥ 50 years) with an averaged yearly rise of 6.2 % in contrast to a lower 3.8 % rise in the middle-aged group (15–49 years) (Fig. 2 and Table 1). Stated differently, during that period the proportion of older MG patients in the overall MG inpatient population increased from 63 % in 1992–73 % in 2009.
Time trend of MG inpatient prevalence from 1992 to 2009. The graph displays the MG inpatient prevalence rates from 1992 till 2009 in relation to 100,000 of the residential population (not age adjusted). Circles: MG patients of all ages combined. Triangles: Patients aged ³ 50 years. Squares: Patients aged 15–49 years. Diamonds: Patients aged £ 14 years. The overall rise of MG inpatient prevalence rates over the years was mainly due to a rise in the fraction of older patients
This development could have been influenced by two known underlying trends affecting the Austrian society as a whole: (i) the ageing of the overall population and (ii) a shift of medical care towards inpatient treatment with rising rates of hospitalisations, particularly for older patients. We, therefore, corrected for both of these factors by expressing the inpatient prevalence in relation to 100,000 population of the relevant age range group (i.e. 15–49 or ³ 50 years) and by adjusting for the average hospitalisation rate in each age group (Table 1). After these corrections the average yearly increases in MG inpatient prevalence rates were lower and similar in both age groups (3.7 % for the middle-aged group and 3.9 % for the older group). However, a substantial yearly rise remained that could not be accounted for by demographic changes or general hospitalisation practices.
Regional differences in the inpatient prevalence of MG
We speculated that any changes in MG inpatient prevalence figures might be the result of improved diagnostic rates and better medical care, both of which are likely to depend on the degree of specialist neurological care available. Between 1990 and 2009 the number of practicing neurologists in Austria increased from 4.3 to 10.0 per 100,000 population resulting in a strong correlation with inpatient prevalence rates (Pearson’s correlation coefficient: 0.97, p = 0.002), which would be compatible with this notion. Another strong argument in support of this hypothesis comes from the regional analysis of MG inpatient prevalence rates amongst the 32 Austrian health districts of 2009 (MG patients were assigned to their residential area irrespective of the location of the hospital). The inpatient prevalence rates in 2009 ranged from 2.48 in rural Liezen/Styria to 13.49 in urban regions near Vienna and Linz (mean and standard deviation across Austria: 7.41 ± 2.54). The numbers of specialist neurologists practicing in each of the 32 health districts also varied substantially and ranged from 1.86 to 23.28 per 100,000 population (mean and standard deviation: 8.90 ± 5.68). There was a clear and significant spatial correlation between these variables (Pearson’s correlation coefficient: 0.43, p = 0.015) (Fig. 3).
MG inpatient prevalence rates in Austria. Map of Austria displaying the inpatient prevalence rates for myasthenia gravis in each of the 32 health districts. MG hospitalisations were assigned to the residential area of the patients irrespective of the location of the hospital. Inpatient prevalences varied substantially between districts but correlated with the density of practicing neurologists
Discussion
In this first epidemiological study of myasthenia gravis (MG) in Austria we utilised the national Austrian hospital discharge register (HDR) to determine epidemiological data relating to this disease. The HDR is a national database with more than 99 % complete coverage of all Austrian hospital admissions. As the correct ICD coding of inpatient stays is tied to the remuneration of hospitals by the obligatory health insurance system these discharge diagnoses are highly accurate as has been shown previously [10, 11]. This is particularly true for unequivocal diagnostic entities such as myasthenia gravis. Given the advantages of this registry, i.e. its large size and the accuracy of the data, we are confident that the epidemiological figures derived here are reliable estimates.
The inpatient prevalence for myasthenia gravis determined in this study (8 per 100,000 residential population) has not been ascertained before and is in itself a variable of interest for planners of health resources. Based on this figure and the hospitalisation rate of our MG outpatients we can deduce that the population prevalence of myasthenia gravis in Austria must be at least 15.69 (95 % CI 13.16–19.42) per 100,000. Our results are thus more in line with the upper estimates in the literature [5]. The discrepancies in prevalence rates in the literature may be due to methodological differences, particularly regarding the ascertainment of MG cases, as cases with minor symptoms might have been missed in some studies. Other authors postulate ethnic or geographic reasons for these differences [13].
We could also confirm—based on a large number of patients—that women display a bimodal age distribution. Further, we showed that the prevalence of MG in males remains uniformly low until the age of 50 with a steep rise thereafter. This is in agreement with some recent studies [14, 15], but in contrast to some older studies, which suggest a bimodal age-distribution also in men [16–18]. An explanation for these discrepancies might be the recent rise in old-age MG with its tail-end overlying and therefore masking a younger age peak.
The availability of nationwide discharge diagnoses over a period of 18 years allowed us to detect unequivocally an increase in the MG inpatient prevalence rate with an average rise of 5.1 % per year. This result is consistent with data from other studies suggesting a rising rate of MG, particularly amongst older patients, over the years [19, 20]. We could further demonstrate that in absolute numbers the increase was indeed largely due to the fraction of older patients and that this rising trend could be partly explained by purely demographic factors—i.e. the ageing of our society—and by the growing tendency of inpatient care in this country. However, a yearly rise of 3.7 % for patients aged between 15 and 49 years and 3.9 % for patients aged ³ 50 years could not be accounted for by obvious reasons. We suggest that one contributing factor could be the growing number of specialist neurologists in this country. This notion is supported not only by the temporal correlation of these two variables but also by a close spatial correlation of the MG inpatient prevalences with the densities of neurologists in Austrian health districts.
Our data, therefore, argue that a sufficient supply with specialists in neurology is a prerequisite for the correct diagnosis of this disease and thus for satisfactory treatment results.
Funding
No external funding was obtained for this study.
References
Meriggioli MN, Sanders DB. Autoimmune myasthenia gravis: emerging clinical and biological heterogeneity. Lancet Neurol. 2009;8:475–90.
Conti-Fine BM, Milani M, Kaminski HJ. Myasthenia gravis: past, present, and future. J Clin Invest. 2006;116:2843–54.
Zimprich F, Assem-Hilger E. Myasthenia gravis. J Neurol Neurochir Psychiatr. 2010;11(2):52–63.
McGrogan A, Sneddon S, de Vries CS. The incidence of myasthenia gravis: a systematic literature review. Neuroepidemiology. 2010;34:171–83.
Carr AS, Cardwell CR, McCarron PO, McConville J. A systematic review of population based epidemiological studies in Myasthenia Gravis. BMC Neurol. 2010;10:46.
Phillips LH, 2nd. The epidemiology of myasthenia gravis. Ann N Y Acad Sci. 2003;998:407–12.
Phillips LH. The epidemiology of myasthenia gravis. Semin Neurol. 2004;24:17–20.
Casetta I, Groppo E, De Gennaro R, Cesnik E, Piccolo L, Volpato S, et al. Myasthenia gravis: a changing pattern of incidence. J Neurol. 2010;257:2015–19.
Phillips LH, 2nd, Torner JC. Epidemiologic evidence for a changing natural history of myasthenia gravis. Neurology. 1996;47(5):1233–8.
Weichbold V, Bertel A, Pelzer A, Pfeiffer KP, Ferenci P. Hepatitis B and C: incidence and regional distribution of hospitalizations in Austria. Wien Klin Wochenschr. 2000;112:995–1001.
Strauss R, Fulop G, Pfeifer C. Hepatitis C in Austria 1993–2000: reporting bias distort HCV epidemiology in Austria. Euro Surveill. 2003;8:113–8.
Wirtz PW, van Dijk JG, van Doorn PA, et al. The epidemiology of the Lambert-Eaton myasthenic syndrome in the Netherlands. Neurology. 2004;63(2):397–8.
Oh SJ, Morgan MB, Lu L, Hatanaka Y, Hemmi S, Young A, et al. Racial differences in myasthenia gravis in Alabama. Muscle Nerve. 2009;39:328–32.
Alshekhlee A, Miles JD, Katirji B, Preston DC, Kaminski HJ. Incidence and mortality rates of myasthenia gravis and myasthenic crisis in US hospitals. Neurology. 2009;72:1548–54.
Bateman KJ, Schinkel M, Little F, Liebenberg L, Vincent A, Heckmann JM. Incidence of seropositive myasthenia gravis in Cape Town and South Africa. S Afr Med J. 2007;97:959–62.
Somnier FE, Keiding N, Paulson OB. Epidemiology of myasthenia gravis in Denmark. A longitudinal and comprehensive population survey. Arch Neurol. 1991;48:733–9.
Ferrari G, Lovaste MG. Epidemiology of myasthenia gravis in the province of Trento (northern Italy). Neuroepidemiology. 1992;11:135–42.
Mantegazza R, Baggi F, Antozzi C, et al. Myasthenia gravis (MG): epidemiological data and prognostic factors. Ann N Y Acad Sci. 2003;998:413–23.
Somnier FE. Increasing incidence of late-onset anti-AChR antibody-seropositive myasthenia gravis. Neurology. 2005;65:928–30.
Aarli JA. Myasthenia gravis in the elderly: Is it different? Ann N Y Acad Sci. 2008;1132:238–43.
Conflict of interest
All authors state that there are no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cetin, H., Fülöp, G., Zach, H. et al. Epidemiology of myasthenia gravis in Austria: rising prevalence in an ageing society. Wien Klin Wochenschr 124, 763–768 (2012). https://doi.org/10.1007/s00508-012-0258-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-012-0258-2