Summary
Background
Contrast induced acute kidney injury is one of the most frequent causes of hospital acquired acute kidney injury. The present study aims to investigate the efficacy of vitamin E or N-acetylcysteine as an adjunct to current standard therapy in the prevention of this clinical predicament. We tested the hypothesis that vitamin E or N-acetylcysteine added to standard therapy with 0.45 % saline is superior in preserving renal function in patients with chronic kidney disease stage 1–4 undergoing elective computer-assisted tomography with nonionic radiocontrast agents when compared to 0.45 % saline alone.
Design
Prospective, randomized, single-center, double-masked, double dummy, placebo-controlled, parallel clinical trial.
Methods
The patients were randomized to either vitamin E (total dose 2160 mg i.v.) or N-acetylcysteine (total dose 4800 mg p.o.) in addition to 0.45 % saline (1 mL/kg/h over 24 h) or saline alone. Serum creatinine change between baseline and 24 h after radiocontrast was the primary outcome. Contrast induced acute kidney injury was defined as a rise in serum creatinine > 25 % over the baseline value within 48 h.
Results
Thirty patients (mean age 74.6 years; 17 females; 9 diabetics; all Caucasians; mean serum creatinine 1.35 mg/dL; mean creatinine clearance 56 mL/min) were enrolled. No patient developed contrast induced acute kidney injury. There was no significant difference in serum creatinine change between the three study arms.
Conclusion
Following radiocontrast administration, neither vitamin E nor N-acetylcystein in addition to saline demonstrated an additional beneficial effect on kidney function when compared to saline alone.
Zusammenfassung
Background
Kontrastmittelinduziertes Nierenversagen ist eine der häufigsten Ursachen für akutes Nierenversagen in hospitalisierten Patienten. Die hier präsentierte Studie untersucht die Wirksamkeit von Vitamin E und N-Acetylcysteine als Zusatztherapie in der Prävention dieser Komplikation. Wir testeten die Hypothese, dass bei Patienten mit chronischer Niereninsuffizienz, welche im Rahmen einer Computertomographie nicht-ionisierendes Kontrastmittel erhalten, Vitamin E oder N-Acetylcysteine als Zusatz zur herkömmlichen Standardtherapie mit 0,45 % Kochsalzlösung besser geeignet sind die Nierenfunktion zu erhalten als die alleinige Gabe der Standardtherapie.
Studiendesign
Prospective, randomisierte, doppelblinde, double-dummy, plazebokontrollierte, parallele, klinische Studie.
Methodik
Patienten erhielten entweder Vitamin E (2160 mg i.v.) oder N-Acetylcysteine (4800 mg p.o.) zusätzlich zu 0,45 % Kochsalzlösung (1 mL/kg/h über 24 h) oder 0,45 % Kochsalzlösung alleine. Primärer Endpunkt der Studie war die Änderung des Serumkreatinins zwischen Studienbeginn und 24 h nach Kontrastmittelgabe. Kontrastmittelinduziertes Nierenversagen wurde definiert als ein Anstieg des Serumkreatinins über 25 % des Basiswertes innerhalb von 48 h nach der Kontrastmittelgabe.
Ergebnisse
Dreissig Patienten wurden in die Studie aufgenommen (mittleres Alter: 74,6 Jahre; 17 Frauen; 9 Diabetiker; mittleres Serumkreatinin: 1.35 mg/dL; mittlere Kreatininclearance: 56 mL/min). Keiner der Patienten entwickelte eine Kontrastmittelnephropathie. In keinem der drei Studienarme kam es zu einer signifikanten Veränderung des Serumkreatinins.
Schlussfolgerung
In der Prävention eines Kontrastmittel-induzierten Nierenversagens ist die zusätzliche Gabe von Vitamin E oder N-Acetylcysteine der Standardtherapoie nicht überlegen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Contrast induced acute kidney injury (CIAKI) is one of the most common causes of hospital-acquired acute kidney injury (AKI); it is defined as an impairment in renal function occurring within 3 days following the intravascular administration of contrast medium in the absence of an alternative etiology. CIAKI commonly presents as a reversible, nonoliguric form of AKI with an increase in baseline serum creatinine of 25 %. In otherwise healthy subjects, the prevalence of CIAKI is less than 3 %; however, with rates as high as 20 % in patients with underlying risk factors (e.g. impaired renal function, cardiovascular disease, diabetic nephropathy, reduced effective arterial volume, and high total dose of contrast agent), the estimated annual incidence of CIAKI in the United States amounts up to 150,000 cases [1,2]. CIAKI is associated with a one-year mortality of up to 35 % and for patients with CIAKI requiring dialysis, one-year mortality was found to be as high as 45.2 % [3]. CIAKI can occur with intraarterial contrast studies (e.g. coronary angiograms) as well as after intravenous administration of contrast media (e.g. computer-assisted tomography; CT) [4]. As the number of interventional procedures remains high, so will the number of contrast medium administrations (currently approximately 60 million doses per year in the US) and therefore the associated risk for CIAKI [5]. It is estimated that in the United States, the annual costs of radiocontrast-induced nephropathy are approximately US$180 million [6]. This notion in addition to the ailments inflicted on our patients highlight the need for strategies and international protocols that can prevent CIAKI.
The proposed pathophysiological mechanisms of CIAKI involve intrarenal vasoconstriction with resultant medullary hypoxia, production of reactive oxygen species (ROS), and direct tubular toxicity. During normal conditions, the mammalian renal medulla pO2 levels are as low as 30 mmHg. The limited regional oxygen supply hardly matches the high local oxygen demand necessary for normal tubular reabsorption [7]. Hence, even minor changes in renal blood flow can markedly affect renal parenchymal oxygenation. Radiocontrast injection leads to an abrupt but transient increase in renal plasma flow, glomerular filtration rate, and urinary output [8]. Nevertheless, after a brief increase in renal blood flow following the administration of radiocontrast, a prolonged decline of 10–25 % below baseline is noted [9]. Studies found that ionic high-osmolar as well as nonionic low-osmolar radiologic contrast media markedly reduced inner medullary blood flow [10,11]. The importance of renal vasoconstriction in the pathogenesis of CIAKI was further strengthened when preclinical trials revealed promising effects of fenoldopam, a selective dopamine-1 receptor agonist that produces renal arterial vasodilation, on renal hemodynamics in animal models [12]. However, a recently performed randomized controlled clinical trial could not extend these findings to humans [13]. The complex pathophysiological mechanism responsible for the development of CIAKI may explain why fenoldopam alone was not able to prevent CIAKI in a clinical setting. Contrast agents cause renal medullary ischemia with generation of free oxygen radicals. ROS enhance tubular transport activity and increase oxygen consumption, thereby augmenting the generation of free oxygen radicals [14]. Moreover, ROS induce endothelial dysfunction, and interfere with the generation of the hypoxia response, thus, setting in motion a vicious circle of hypoxia, free radical formation, and further hypoxic injury [15]. Studies have shown increased markers of ROS (e.g. 15-Isoprostane-F2t) in the urine after contrast media administration [16,17]. On a further note, oxidative stress was found to augment oxygen consumption and impair oxygen tension in the kidneys of diabetic rats [18]. This finding goes well in line with the clinical notion that N-acetylcysteine (NAC), a free radical scavenger, yields some protection from developing CIAKI in patients with diabetic nephropathy [16].
Another important component of the antioxidative network and protective mechanism is vitamin E. Vitamin E is highly lipophilic and is incorporated readily into cell membranes. Its efficiency as a free radical scavenger has been intensively studied on animal models of oxidative stress as well as hepatic and cerebral ischemia/reperfusion injury [18–20]. However, there are still several uncertainties about the usefulness of antioxidant therapy in a clinical setting. For instance, it is questionable whether most currently used antioxidants are reaching their target, namely the mitochondria, which are the primary site of free radical generation [21].
Given the current confusion as to whether antioxidant therapy has a clinical application in the prevention of CIAKI, our study set itself to compare two free radical scavengers, namely N-acetylcysteine (NAC) and vitamin E, when given additionally to the current standard saline therapy in a randomized, double-masked, double-dummy, placebo-controlled trial.
Methods
Study population
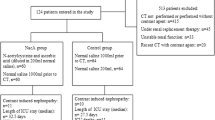
This study was approved by the Ethics Committee, at the Krankenhaus der Barmherzigen Brüder, Graz, Austria, and carried out in accordance with the declaration of Helsinki and Good Clinical Practice regulations. The enrollment period started in August 2002 and ended in July 2003. The patients were enrolled after receiving information regarding details of the clinical study and giving their written and dated consent. The patients 18 years of age or older with a serum creatinine above 1.25 mg/dL for males and 1.09 mg/dL for females (cutoff values were defined by using the hospital’s normal serum creatinine ranges), who did not undergo renal replacement therapy, were considered for enrollment. Exclusion criteria included acute kidney injury, a serum creatinine increase in the enrollment period of more than 0.2 mg/dL, administration of vitamin E, NAC, or other antioxidant therapy within 4 weeks prior to the radiological investigation. Further exclusion criteria were participation in an investigational clinical trial within 1 month prior to the start of the study, known or suspected allergy to the investigational drugs, and current use of a theophylline, dopamine, furosemide, or mannitol.
Study protocol
This single-center, prospective, double-blind, double-dummy, placebo-controlled, randomized, parallel in-center clinical trial tested the hypothesis that Vitamin E or NAC when added to standard therapy with half-normal (0.45 %) saline is superior to standard half-normal saline therapy in preserving renal function in patients with CKD undergoing elective diagnostic nonionic radiocontrast CT. Because this study was conducted in patients with preexisting CKD, 0.45 % saline rather than 0.9 % saline was used in order to avoid potentially harmful salt loading of the patient. Eligible patients were randomly assigned in a double-masked manner in a 1:1:1 ratio to one of the following three treatment arms:
-
NAC group: N-acetylcysteine granules + placebo emulsion + 0.45 % saline infusion (prepared by 1:1 dilution of 0.9 % saline with 5 % glucose solution)
-
Vitamin E: group placebo granules + Vitamin E emulsion + 0.45 % saline infusion
-
Control group: placebo granules + placebo emulsion + 0.45 % saline infusion
All study drugs were provided by Fresenius Kabi Austria GmbH, Graz, Austria. Randomization was performed by a statistician not involved in the data analysis, a block randomization scheme (block size = 6) was used based on the responsible statisticians’ software, and all associated details were documented in the office of the responsible statistician. Treatment allocation was not known to the investigator, the statistician evaluating the study, the clinical study personnel, the patient, and the study sponsor. Patients’ demographics including body weight, height, and smoking status were documented. A detailed medical history was obtained and a full physical examination was performed 2 days prior to the CT. Blood was drawn 24 h before CT, immediately before the CT, 24 and 48 h after CT (Fig. 1). Creatinine clearance was determined based on urine collections in the 24 h immediately before and after CT. During the CT, the patients received the contrast agent 100 ml iopromide (Ultravist 300, Schering, Schering AG. Berlin, Germany) which is a nonionic radiocontrast agent with an iodine content of 300 mg/ml.
Study treatments were administered at prespecified time points. All patients received 0.45 % saline infusion at a rate of 1 ml/kg BW/h for 12 h before and after CT. Over a period of 30 min, an emulsion containing 540 mg of vitamin E (or placebo emulsion in the NAC and the control group) was given intravenously 12 and 6 h before and 6 and 12 h after the CT. NAC 1200 mg (or placebo granules in the vitamin E and control groups) were administrated per oral route, 12 and 6 h before and 6 and 12 h after the CT. All patients received half-normal saline infusion for 12 h prior and for 12 h after CT. Vital signs (blood pressure, heart rate, body temperature) were monitored at the intervention time points and at discharge.
Study end points, laboratory tests, and statistical analyses
The primary efficacy end point was defined as a change in serum creatinine concentration from time of contrast medium administration to 24 h after CT (Fig. 1). Secondary efficacy end points were a change in serum creatinine concentration from time of contrast medium administration to 48 h after CT, the change in creatinine clearance between 24 h before and 24 h after CT, and the development of CIAKI, defined as an increase in serum creatinine of more than 25 % over the baseline value in the following 48 h after CT. Creatinine was determined by the Jaffe method. Estimated glomerular filtration rate (eGFR) was calculated applying the 4-variable Levey-modified version of the Modification of Diet in Renal Disease (MDRD) formula [22,23].
Continuous data are presented using the mean ± standard deviation (SD). Groups were compared using one-way ANOVA and post-hoc test with Bonferroni correction, or by χ2 test when appropriate. The formal null hypothesis of this study stated that the preventive effects of vitamin E or NAC do not differ from the control arm (saline). A two-sidedp < 0.05 was considered significant. Treatment effect differences between groups are reported as mean and 95 % confidence interval (95 % CI).
Sample size estimation based on a study by Tepel et al. [24] indicated that 90 patients (30 per treatment arm) are sufficient to achieve 90 % power to detect a serum creatinine change of 0.6 mg/dl at a significance level α of 0.05 between the three groups. After 30 patients, an interim analysis was conducted with the option to terminate the trial in the absence of a trend toward a benefit of either treatment. All analyses were done on an intention-to-treat basis. All statistical analyses were performed with SPSS version 11.5 (SPSS Inc.).
Results
The baseline characteristics of the study population are summarized in Table 1. Baseline demographics were well matched between the three treatment groups. The trial was terminated based on the results of the interim analysis after the enrollment of 30 patients. One patient was excluded after randomization and prior to treatment administration due to a protocol violation (administration of theophylline prior to the administration of study treatment). All subsequent analyses were done with the 29 remaining patients.
None of the patients developed CIAKI, defined as an increase in serum creatinine of more than 25 % over the baseline value in the 48 h following CT scan. Serum creatinine concentration changes 24 and 48 h after contrast agent administration did not differ between the three treatment arms (Table 2 and Fig. 2a,b, andc).
Change of creatinine clearance and eGFR 24 h after contrast agent administration did not differ between the three groups (Table 2).
Discussion
This study was designed to investigate the prophylactic effect of vitamin E and NAC, when added to the current standard therapy (i.e. saline infusion), in preventing CIAKI in a CKD population undergoing elective contrast CT investigation. None of the 29 studied patients developed CIAKI; however, our results indicate that there is no beneficial effect on kidney function (as measured by serum creatinine levels) with addition of intravenous vitamin E or oral NAC to standard therapy.
Contrast induced acute kidney injury is a major cause of hospitalization and mortality in the CKD population, especially in patients with diabetes. Previous studies have shed light on the multifaceted pathogenesis of CIAKI; although not fully elucidated, two mechanism of injury are currently being thought of as the main drivers of end-organ damage in this clinical conundrum: namely renal hypoperfusion and free radical generation [5,21]. First, the vasoconstrictory effects of the contrast agent itself can cause renal medullary ischemia due to hypoperfusion, which then leads to the generation of free oxygen species causing damage to the tubular epithelial cells and acute tubular necrosis. Free oxygen radicals have also been shown to cause endothelial dysfunction, hampering the hypoxia-adaptive response [15]. This may set off a vicious cycle with hypoxia leading to the generation of ROS, which in turn aggravates the effects of hypoxia, which further increases ROS generation; thereby augmenting cellular injury and ameliorating adaptive measures.
Several trials investigated the role of NAC as a free radical scavenger and its possible vasodilatory effects; however, there is still substantial disagreement regarding its efficacy in prevention of CIAKI. In agreement with our findings, a recently performed study in 90 diabetic CKD patients undergoing elective cardiac angiography could not demonstrate a significant benefit of NAC use as an adjunct to hydration in CIAKI prevention [25]. It has been argued that the levels of NAC administered in these previous studies, which failed to demonstrate a protective effect of NAC administration, are too low to cause a sufficient decrease in ROS [26]. However, we were unable to demonstrate a favorable effect of NAC over standard therapy alone, when given at a dose of 1,200 mg twice daily [26,27].
In recent years, the focus on vitamin E has increased considerably due to its antioxidant properties, with alpha–tocopherol being the main compound of interest, as its intestinal absorption, hepatic transport, and cellular uptake have been well studied and described [28]. In the present study, an intravenous emulsion of alpha-tocopherol has been used, since it has been shown that absorption and bioavailability of orally administered vitamin E strongly rely on physiological factors of fat digestion, such as pancreatic esterase secretion and chylomicron formation [29,30]. In our study, no beneficial effects of intravenous alpha-tocopherol administration on kidney function in CKD patients undergoing elective CT were seen. Interestingly, in a recent randomized controlled trial performed in 103 Thai CKD patients undergoing elective coronary angiography, 525 IU of oral alpha-tocopherol led to a significant 17.2 % reduction of CIAKI (5.9 % in the intervention group; 23.1 % in the placebo group) [31]. This finding is promising and suggests that the efficacy of vitamin E may depend on its route of administration. However, bearing in mind the uncertainties involved with oral administration (e.g. absorption, first-pass effect), one would suspect the parenteral route to be superior. Of note, the frequency of CIAKI in the placebo group was unusually high, considering that none of the patients had CKD stage greater than 2.
A limitation of most studies of preventive strategies, including ours, is that approaches are targeted only against one of the several pathophysiological aspects of CIAKI. Future studies investigating combination therapies, aimed against hypoperfusion and ROS generation (e.g. fenoldopam in conjunction with vitamin E), are of great interest, since they are likely to better account for the complex nature of CIAKI. A recent finding in support of combination strategies comes from the REMEDIAL study results, where the combination of isotonic bicarbonate and NAC has shown to offer better protection from CIAKI development than NAC and saline alone [32].
Our study has limitations: first, the trial was terminated after 30 patients, since the interim analysis revealed no significant trend for a difference between the treatment arms and a continuation was deemed unjustified by the study team. Second, the study population consisted only of Caucasians, thereby limiting the adaptability of our results to other races. Third, 0.45 % saline rather than 0.9 % saline was used. The reason for this approach was to avoid salt loading and potentially harmful acute expansion of the extracellular volume; all enrolled patients had, by design, preexisting CKD and thus an increased likelihood of salt and water retention. Finally, since no patient met the primary endpoint, the final conclusion remains difficult. Nevertheless, since all studied patients received hydration therapy, it is conceivable that standard treatment alone exhibited a preventive effect, which could not be further increased by the addition of NAC or vitamin E.
In conclusion, adding intravenous vitamin E or oral NAC, to 0.45 % saline therapy for prevention of CIAKI, did not translate into improved kidney function in CKD patients undergoing elective CT with radiocontrast administration. Future studies employing combination therapies, which are designed to account for the multifaceted pathophysiologic nature of CIAKI, will hopefully lead to the development of more successful preventive strategies in patients at high risk.
Acknowledgements
This study was supported by Fresenius Kabi Austria GmbH, Graz, Austria.
References
McCullough PA, Sandberg KR. Epidemiology of contrast-induced nephropathy. Rev Cardiovasc Med. 2003;4 (Suppl 5):S3–9.
Mehran R, Nikolsky E. Contrast-induced nephropathy: definition, epidemiology, and patients at risk. Kidney Int Suppl. 2006;100:S11–5.
McCullough PA. Contrast-induced acute kidney injury. J Am Coll Cardiol. 2008;51:1419–28.
From AM, Bartholmai BJ, Williams AW, Cha SS, Pflueger A, McDonald FS. Sodium bicarbonate is associated with an increased incidence of contrast nephropathy: a retrospective cohort study of 7977 patients at mayo clinic. Clin J Am Soc Nephrol. 2008;3:10–18.
Persson PB, Hansell P, Liss P. Pathophysiology of contrast medium-induced nephropathy. Kidney Int. 2005;68:14–22.
McCullough PA, Soman SS. Contrast-induced nephropathy. Crit Care Clin. 2005;21:261–80.
Brezis M, Rosen S. Hypoxia of the renal medulla–its implications for disease. N Engl J Med. 1995;332:647–55.
Arakawa K, Suzuki H, Naitoh M, Matsumoto A, Hayashi K, Matsuda H, et al. Role of adenosine in the renal responses to contrast medium. Kidney Int. 1996;49:1199–1206.
Workman RJ, Shaff MI, Jackson RV, Diggs J, Frazer MG, Briscoe C. Relationship of renal hemodynamic and functional changes following intravascular contrast to the renin-angiotensin system and renal prostacyclin in the dog. Invest Radiol. 1983;18:160–6.
Liss P, Nygren A, Olsson U, Ulfendahl HR, Erikson U. Effects of contrast media and mannitol on renal medullary blood flow and red cell aggregation in the rat kidney. Kidney Int. 1996;49:1268–75.
Nygren A, Ulfendahl HR, Hansell P, Erikson U. Effects of intravenous contrast media on cortical and medullary blood flow in the rat kidney. Invest Radiol. 1988;23:753–61.
Bakris GL, Lass NA, Glock D. Renal hemodynamics in radiocontrast medium-induced renal dysfunction: a role for dopamine-1 receptors. Kidney Int. 1999;56:206–10.
Stone GW, McCullough PA, Tumlin JA, Lepor NE, Madyoon H, Murray P, et al. Fenoldopam mesylate for the prevention of contrast-induced nephropathy: a randomized controlled trial. JAMA. 2003;290:2284–91.
Juncos R, Garvin JL. Superoxide enhances Na-K-2Cl cotransporter activity in the thick ascending limb. Am J Physiol Renal Physiol. 2005;288:F982–7.
Wellman TL, Jenkins J, Penar PL, Tranmer B, Zahr R, Lounsbury KM. Nitric oxide and reactive oxygen species exert opposing effects on the stability of hypoxia-inducible factor-1alpha (HIF-1alpha) in explants of human pial arteries. FASEB J. 2004;18:379–81.
Drager LF, Andrade L, Barros de Toledo JF, Laurindo FR, Machado Cesar LA, Seguro AC. Renal effects of N-acetylcysteine in patients at risk for contrast nephropathy: decrease in oxidant stress-mediated renal tubular injury. Nephrol Dial Transplant. 2004;19:1803–7.
Sandhu C, Newman DJ, Morgan R, Belli AM, Oliveira D. The role of oxygen free radicals in contrast induced nephrotoxicity. Acad Radiol. 2002;9 (Suppl 2):S436–7.
Palm F, Cederberg J, Hansell P, Liss P, Carlsson PO. Reactive oxygen species cause diabetes-induced decrease in renal oxygen tension. Diabetologia. 2003;46:1153–60.
Abd-El-Fattah AA, El-Sawalhi MM, Rashed ER, El-Ghazaly MA. Possible role of vitamin E, coenzyme Q10 and rutin in protection against cerebral ischemia/reperfusion injury in irradiated rats. Int J Radiat Biol. 2010;86:1070–8.
Abu-Amara M, Gurusamy K, Hori S, Glantzounis G, Fuller B, Davidson BR. Systematic review of randomized controlled trials of pharmacological interventions to reduce ischaemia-reperfusion injury in elective liver resection with vascular occlusion. HPB (Oxford). 2010;12:4–14.
Pflueger A, Abramowitz D, Calvin AD. Role of oxidative stress in contrast-induced acute kidney injury in diabetes mellitus. Med Sci Monit. 2009;15:RA125–36.
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130:461–70.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–12.
Tepel M, Van Der Giet M, Schwarzfeld C, Laufer U, Liermann D, Zidek W. Prevention of radiographic-contrast-agent-induced reductions in renal function by acetylcysteine. N Engl J Med. 2000;343:180–4.
Amini M, Salarifar M, Amirbaigloo A, Masoudkabir F, Esfahani F. N-acetylcysteine does not prevent contrast-induced nephropathy after cardiac catheterization in patients with diabetes mellitus and chronic kidney disease: a randomized clinical trial. Trials. 2009;10:45.
Calvin AD, Misra S, Pflueger A. Contrast-induced acute kidney injury and diabetic nephropathy. Nat Rev Nephrol. 2010;6:679–88.
Marenzi G, Assanelli E, Marana I, Lauri G, Campodonico J, Grazi M, et al. N-acetylcysteine and contrast-induced nephropathy in primary angioplasty. N Engl J Med. 2006;354:2773–82.
Rigotti A. Absorption, transport, and tissue delivery of vitamin E. Mol Aspects Med. 2007;28:423–36.
Nakamura T, Aoyama Y, Fujita T, Katsui G. Studies on tocopherol derivatives: V. Intestinal absorption of several d,1–3,4–3H2-alpha-tocopheryl esters in the rat. Lipids. 1975;10:627–33.
Traber MG, Goldberg I, Davidson E, Lagmay N, Kayden HJ. Vitamin E uptake by human intestinal cells during lipolysis in vitro. Gastroenterology. 1990;98:96–103.
Tasanarong A, Piyayotai D, Thitiarchakul S. Protection of radiocontrast induced nephropathy by vitamin E (alpha tocopherol): a randomized controlled pilot study. J Med Assoc Thai. 2009;92:1273–81.
Briguori C, Airoldi F, D’Andrea D, Bonizzoni E, Morici N, Focaccio A, et al. Renal Insufficiency Following Contrast Media Administration Trial (REMEDIAL): a randomized comparison of 3 preventive strategies. Circulation. 2007;115:1211–7.
Conflict of interest
Mag. Dr. Gerald Sendlhofer was employed at Fresenius Kabi Austria GmbH at the time the study was undertaken. His employment at Fresenius Kabi ended in July 2006. All the other authors have no conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kitzler, T., Jaberi, A., Sendlhofer, G. et al. Efficacy of vitamin E and N-acetylcysteine in the prevention of contrast induced kidney injury in patients with chronic kidney disease: a double blind, randomized controlled trial. Wien Klin Wochenschr 124, 312–319 (2012). https://doi.org/10.1007/s00508-012-0169-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-012-0169-2
Keywords
- Computer-assisted tomography
- Contrast induced acute kidney injury
- N-acetylcysteine
- Randomized controlled trial
- Vitamin E
- Chronic kidney disease