Abstract
The aim of our study was to compare and assess the effectiveness of antioxidant mixtures on the erythrocytes (RBC) of adult male albino rats (Wister) subjected to simulated intermittent high altitudes—5,100 m (AL1) and 6,700 m (AL2)—to induce oxidative stress (OS). To achieve our objective, we pre-supplemented four sets of animals with different antioxidant mixtures [vitamin E (vit.E; 50 IU/kg BW), vitamin C (vit.C; 400 mg/kg) and l-carnitine (400 mg/kg)] in different combinations [M1 (vit.E+vit.C), M2 (vit.C+carnitine), M3 (vit.E+carnitine) and M4 (vit.C+vit.E+carnitine)] for 30 days prior to as well during exposure to intermittent hypobaric hypoxia (IHH). Membrane instability, in terms of osmotic fragility and hemolysis, decreased in RBCs of supplemented animals. There was a significant increase in the activity of glutathione peroxidase in the RBCs of supplemented animals. We confirmed OS imposed by IHH with assays relating to lipid [thiobarbituric acid reactive substances (TBARS) and lipofuscin (LF)] and protein (carbonyl, PrC) oxidation, and found a positive correlation between PrC and hemolysis, with a decrease in both upon supplementation with M3 and M4 mixtures. Fluorescence microscopic observation showed a maximum decrease in the LF content in rats administered M4 and M1 compared to those on M2 and M3 mixtures at both altitudes. We suggest that multiple antioxidant fortifications are effective in overcoming increased OS experienced by RBCs at high altitudes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The mammalian erythrocyte [red blood cell (RBC)] is an ideal cell model in which to study free radical-mediated injury, since it is enucleated and has a short life span. Changes in membrane lipids can affect the RBC shape by disrupting the balance in area between the two lipid leaflets.
Autoxidation of hemoglobin (Hb) produces superoxide as well as methemoglobin. It is known that Hb reacts with hydrogen peroxide to produce ferrylhemoglobin, which is a strong oxidant (Everse and Hsia 1997). Hb binds to membrane proteins of the RBC, particularly under hypoxic conditions. The reactive oxygen species (ROS) generated by bound Hb may not be accessible to cellular antioxidants, facilitating the production of heme degradation products in close proximity to the membrane (Bakonyi and Radak 2004; Nagababu and Rifkind 2000; Nagababu et al. 2003).
Erythrocyte membrane proteins are susceptible to covalent damage, including cross-linking and aggregation by free radical-induced peroxidation products. Extensive peroxidation of lipids causes changes in fluidity, e.g., a fall in the membrane potential, and an increase in the permeability to different ions that finally lead to hemolysis. Therefore erythrocytes are very sensitive to oxidative injury (Bernabucci et al. 2002). To defend themselves against oxidative stress (OS), erythrocytes are equipped with an effective and complex antioxidant system, including protective enzymes and biological antioxidants such as superoxide dismutase (SOD), catalase (CAT), glutathione peroxidase (GPx), glutathione (GSH), vitamin C, and vitamin E. Despite the efficacy of this antioxidant system, the capacity to repair oxidative damage to RBCs is limited.
At intermittent hypobaric hypoxic (IHH) situations during high altitude exposure, cells become more susceptible to oxidative injury. It is well known that OS results in damage to cells, which may lead to the loss of cell function. The biochemical changes taking place during acute hypoxia at altitude may make cells particularly susceptible to oxidative injury. Thus there could be a role for antioxidant supplements in protecting the cells from oxidative injury. Among the potential antioxidants in foods, vitamin C and vitamin E are the principal dietary antioxidants that protect erythrocytes from damage caused by ROS. Non-enzymic antioxidants such as vitamin E (vit.E), vitamin C (vit.C) and l-carnitine (LC) act towards reducing the OS caused by IHH as demonstrated in an earlier study (Asha et al. 2007). Although studies have been conducted to investigate the effect of altered physiological state during exposure to high altitude, much still needs to be evaluated regarding the extent of the influence of these antioxidants when supplemented as mixtures.
In this study, we report three different findings on the in vitro effects of different mixtures of vitamin E, vitamin C and carnitine on (1) hematological parameters (Hb, osmotic fragility and hemolysis); (2) cellular glutathione peroxidase; and (3) lipid peroxidation (LPO) [thiobarbituric acid reactive substances (TBARS) and lipofuscin (LF)] and protein oxidation (PrC) in erythrocytes of rats subjected to IHH.
Materials and methods
The present study and protocols were approved by the Institutional Animal Ethics Committee (IAEC), Bangalore University, Bangalore, India.
Chemicals
The Hb reagent was obtained from Coral Clinical Systems (Goa, India). Thiobarbituric acid (TBA); glutathione reductase; glutathione; nicotinamide dinucleotide phosphate (NADPH); t-butyl hydroperoxide; acrylamide; bis-acrylamide; sodium dodecylsulphate (SDS); 1, 1, 3, 3-tetramethoxy propane (TMP); α-tocopherol; and bovine serum albumin (BSA) stock were purchased from Sigma-Aldrich Chemicals (St. Louis, MO); LC was procured from Lonza (Basel, Switzerland). Ascorbic acid was from S.D.Fine Chemicals (Mumbai, India). All other chemicals used were of reagent grade and organic solvents were of spectral grade.
Supplementation of antioxidants
Adult male rats (3 months old; Wistar strain) were obtained from the Central Animal Facility at the Indian Institute of Science, Bangalore, and were maintained in our animal house. At 4 months of age, animals were grouped into four sets: control normal (CON-N), control supplemented, altitude normal (AL-N) and altitude supplemented. Animals were supplemented with mixtures of antioxidants: M1 (vit.E+vit.C), M2 (vit.C+LC), M3 (vit.E+LC) or M4 (vit.C+vit.E+LC) before and during exposure to altitudes at concentrations of 50 IU/ kg body weight ( BW) (vit.E, tocopherol) and 400 mg/ kg BW (vit.C, ascorbic acid and LC as indicated in Table 1.
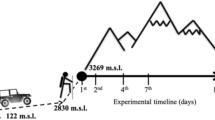
Altichamber for stimulation of hypobaric hypoxia
The procedure for exposure of animals to IHH was essentially that reported in an earlier work (Asha et al. 2005). In brief, the altichamber consisted of a thick-walled high pressure resistant glass animal chamber fitted with brass lid and with three brass outlets connected to the other components of the unit via vacuum tubes. The first outlet was connected to a manometer, which indicates the barometric pressure, while the third outlet was fitted to an adjustable knob to regulate the entry of air and hence the developed pressure in the chamber. During the simulation, pressure was gradually decreased until a particular pressure was reached. This was possible by exposing the animal to a step-wise reduction in pressure by 30 mm Hg/day until the required pressure, i.e., 370 mm Hg (representing an altitude of 5,700 m) and 340 mm Hg (6,300 m) was reached. After exposing the animals for 30 min or 90 min, the pressure was gradually decreased to reach normal levels. The schedule was followed every day for 9 or 15 days (Table 1).
Blood sampling
Animals were lightly anaesthetized with ether and 4 ml blood was carefully aspirated from the heart into 5 ml collecting tubes that had been rinsed with 10% ethylene diamine tetracetic acid (EDTA).
Erythrocyte separation
Erythrocytes were isolated in Eppendorf tubes by centrifuging in a fixed angle rotor (No.1, RV/FM, Superspin, Plastocraft), for 20 min at 1,000 g. The plasma and buffy coat were removed using a micropipette. The cell pellet was washed three times with 310 mOsm isotonic phosphate buffer, pH 7.4, centrifuged at 1000 g for 10 min and finally suspended in an equal volume of isotonic phosphate buffer. This constituted the erythrocyte suspension, which was stored at 4°C in Eppendorf tubes for 24 h until further analysis (Dodge et al. 1963).
Erythrocyte membrane preparation
The above procedure was followed by hemolysis for membrane preparation. Hemolysis was performed by pipetting 1 ml aliquots of washed erythrocyte suspension into a plastic centrifuge tube containing 14 ml hypotonic phosphate buffer (20 mOsm, pH 7.4). The resulting suspension was the hemolysate. The contents were mixed by gentle swirling and then centrifuged in a fixed angle rotor (No.6) at 20,000 g for 40 min. The supernatant was decanted carefully and the ghost (membrane) was resuspended by adding same strength buffer to reconstitute the original volume. The ghosts were washed thrice with the same hypotonic buffer (1:14), centrifuged for 10 min at 20,000 g. This was followed by a resuspension of the cell pellet in the isotonic phosphate buffer at 4°C (Dodge et al. 1963).
Hemoglobin
Hb was measured using a Hemocor-D Kit (Coral Clinical Systems), which utilizes the cyanomethaemoglobin method. Whole blood was incubated with Hb reagent for 3 min at room temperature and absorbance was measured at 540 nm. Hb concentration was represented in terms of g/dl.
Osmotic fragility
The procedure was slightly modified from that of O’Dell et al. (1987). A 100 µl aliquot of washed erythrocyte suspension was added to tubes with 2 ml of 0.3%, 0.4%, and 0.9% buffered salt solutions (BSS; pH 7.4). These tubes were allowed to stand at room temperature for 30 min, centrifuged at 1,270 g for 10 min to pellet the cells and the absorbance of the supernatant measured at 540 nm. Hemolysis in each tube was expressed as a percentage, taking as 100% the maximum value of absorbance of distilled water (0.9% buffered salt solution was considered as control).
Hemolysis
A 5% suspension of washed, packed erythrocytes in buffer (310 mOsm) was mixed with the same volume of 8 mM H2O2. The mixture was incubated at 37°C for 2 h in a BOD incubator. One of the samples was pre-treated with 10 μl 1 mM sodium azide, an inhibitor of CAT, at 37°C for 10 min before inducing OS as above. Hemolysis was determined by measuring released Hb into the supernatant of the induced samples at 540 nm and was expressed on the basis of the maximum absorbance (100%) in aliquots of erythrocytes completely hemolysed in distilled water (Senturk et al. 2001).
Antioxidant enzyme—glutathione peroxidase
Glutathione peroxidase (GSH-Px, EC 1.11.1.9) was analyzed by the method of Flohe and Gunzler (1984): 50 µl 0.1 M phosphate buffer (pH 7.0), 100 µl enzyme sample, 100 µl glutathione reductase (0.24 units) and 100 µl 10 mM GSH were mixed. The mixture was pre-incubated for 10 min at 37°C followed by the addition of 100 µl 1.5 mM NADPH in 0.1% NaHCO3. The overall reaction was started by adding 100 µl pre-warmed hydrogen peroxide, and the decrease in absorption at 340 nm was monitored for 3 min. Enzyme activity was expressed as units/g Hb; 1 unit corresponds to 1 mM NADPH oxidized/min.
Lipid peroxidation
Lipofuscin
LF, a byproduct of reactions between carbonyls and aldehydes resulting from LPO reactions, was measured in erythrocytes (Monji et al. 1994). The samples were examined under a fluorescence microscope (Olympus IX 70). A 10 µl aliquot of the erythrocyte suspension (diluted 20 times in isotonic phosphate buffer) consisting of 200–300 cells was placed on a slide with a cover slip. An individual experiment (n) was observed in a field of 50–60 cells on a cover slip and for five cover slips originating from five animals. In the micrographs, LF pigments appeared bluish in color under a UV broad band filter (see Electronic Supplementary Material). Cells were imaged using a cool-snap PC-controlled camera coupled with micro image software for the quantification of changes in fluorescence, which were expressed in arbitrary units.
Thiobarbituric acid reactive substances
TBARS, a product of LPO, were determined according to the method of Ohkawa et al. (1979). In brief, the sample was added to 8.1% SDS, vortexed and incubated for 10 min at room temperature. This was followed by the addition of 375 µl 20% acetic acid and an equal volume of 0.6% TBA, and placing in a boiling water bath for 60 min. The samples were allowed to cool and 1.25 ml butanol-pyridine (15:1) was added and centrifuged at 640 g for 5 min. Absorbance was measured at 532 nm with 1,1,3,3-tetramethoxy propane as standard. TBARS concentration was expressed as nmol/mg protein.
Protein oxidation
Protein carbonyl content
Carbonyl was measured as an index of protein oxidation as described by Uchida and Stadtman (1993). In brief, the experimental tube included 0.8 ml membrane sample in isotonic buffer with an equal volume of 0.1% (w/v) 2, 4-DNPH in 2 N HCl, whereas the control tube contained equal volumes of sample and 2N HCl. Both sets were incubated at room temperature for 60 min. After the incubation period, 20% TCA was added and the contents centrifuged at 1,900 g. After washing with ethanol:ethylacetate mixture, the residue was dissolved in 8 M guanidine hydrochloride in 133 mM Tris solution (pH 7.2) containing 13 mM EDTA and centrifuged at 1,900 g. The absorbency of each sample was read at 365 nm in an UV/VIS spectrophotometer (ELICO, Model SL 159) against the control. The results were expressed as µmoles of 2,4-DNPH incorporated/mg protein based on a molar extinction coefficient of 2.1 × 104 M−1 cm−1 for aliphatic hydrazones.
Protein determination
Protein was determined by the method of Lowry et al (1951) using BSA as the standard.
Statistics
Results are represented as means ± SE. Values between the groups were analyzed by one-way ANOVA and was considered significant at P < 0.05. Tukey-Kramer’s multiple comparison test was performed for hemoglobin and lipofuscin using GraphPad Instat 3 software. Protein carbonyl was also analyzed by one-way ANOVA followed by Tukey-Kramer’s multiple comparison test. Two-way ANOVA was performed between the groups and sub-groups to analyze hemolysis and osmotic fragility followed by Bonferroni Post test, using GraphPad Prism software. Correlation analysis was performed between hemolysis and protein carbonyls and the values were considered significant at P < 0.05 using GraphPad Instat 3 software.
Results
Hemoglobin
Animals supplemented with antioxidant mixtures showed significant changes in Hb within sub groups, but not within different antioxidant groups. Increases in Hb were also noted in the AL1(M1) group (by 7%) and AL1(M4; by 5%) while Hb was reduced in AL2(M1) by 4% as represented in Fig. 1.
Changes in hemoglobin (Hb) level in erythrocytes of animals exposed to high altitude. Data are means ± SEM from five animals. CON-N Control, AL1 Altitude 1 (5,700 m), AL2 Altitude 2 (6,300 m), M1 Vitamin E (vit.E) + Vitamin C (vit.C), M2 vit.C + l-carnitine (LC), M3 vit.E + vit.C, M4 vit.E + vit.C + LC. Changes between groups were analyzed by ANOVA and further tested by Bonferroni Post test using Graphpad Prism software; P < 0.05 was considered significant. Values within a group are represented in lower case (a, b). Those not sharing the same letters are significant
Osmotic fragility
Osmotic fragility of erythrocytes in animals supplemented with antioxidant mixtures M1–M4 are represented in Table 2. Membrane fragility was reduced by 60% in sedentary rats supplemented with antioxidant mixtures in 0.3% BSS. Osmotic fragility decreased by 34%, 48%, 60% and 43% compared to CON-N in 0.4% BSS in groups CON (M1), CON (M2), CON (M3), and CON (M4) respectively. Fragility also decreased in 0.9% in supplemented controls with M1 (58%), M2 (51%), M3 (58%) and M4 (57%) with respect to unsupplemented controls.
Cells from AL1 (M3) showed a 25% decrease in fragility. When exposed to altitude 2, supplemented animals showed a reduction in erythrocyte fragility by 38% and 47% in AL2 (M1), 40% and 46% in AL2 (M2), 48% and 53% in AL2 (M3), and 47% and 54% in AL2 (M4) in 0.3% and 0.4% BSS respectively, with respect to altitude normals. Fragility also decreased in 0.9% in AL2 animals supplemented with M1, 33%; M2, 54%; M3, 58% and M4, 58% with respect to controls. M3 and M4 were more effective than M1 and M2 at protecting cells from stress and loss in membrane stability at 0.3% BSS in contrast to those stressed at 0.4%, which exhibited no marked effects for any of the antioxidant combinations.
Hemolysis
Experiments were conducted to test the potential for antioxidant mixtures to reduce LPO-induced hemolysis in animals exposed to high altitude (Table 3). Reduced hemolysis of LP-I (−i) was seen in all the groups on supplementation and exposure to altitude 2 (6,300 m) over their respective controls, with 23% in AL2 (M1), 17% in AL2 (M2), 23% in AL2 (M3) 21% in AL2 (M4) with respect to altitude normals. In the supplemented control, a decrease was seen in CON(M2) compared to control in LP-I(+i).
Lipid peroxidation
Another set of experiments was conducted to relate the observed hematological changes in LPO in terms of TBARS in the membrane and LF on whole cells. TBARS decreased in relation to their respective altitude normal in animals that were supplemented and exposed to altitude 1 (M1, 58%; M2, 69%; M3, 58%; M4, 53%) and altitude 2 (M1, 47%; M2, 63%; M3, 44%; M2, 35%; Fig. 2a–d). LF also showed a reduction in AL1 (M1), 67%; AL2 (M1), 74%; AL1 (M2), 48%; AL2 (M2), 63%; AL1 (M3), 61%; AL2 (M3), 69%; AL1 (M4), 65% and AL2 (M4), 74% with respect to the corresponding AL-N (Fig. 3a–d).
a–d Changes in malondialdehyde (MDA) concentration in erythrocytes of animals exposed to high altitude. Data are means ± SEM from five animals. CON-N Control, AL1-N Altitude 1 (5,700 m), AL2-N Altitude 2 (6,300 m). Supplements: aM1 Vitamin E (vit.E) + Vitamin C (vit.C), bM2 vit.C + l-carnitine (LC), cM3 vit.E + vit.C, dM4 vit.E + vit.C + LC. Changes between groups were analyzed by ANOVA and further tested by Bonferroni Post test using Graphpad Prism software; P < 0.05 was considered significant. Values within a group are represented in upper case (A, B, C). Those not sharing the same letters are significant
a–d Changes in lipofuscin (LF) concentration in erythrocytes of animals exposed to high altitude. Data are means ± SEM from five animals. CON-N Control, AL1-N Altitude 1 (5,700 m), AL2-N Altitude 2 (6,300 m). Supplements: aM1 Vitamin E (vit.E) + Vitamin C (vit.C), bM2 vit.C + l-carnitine (LC), cM3 vit.E + vit.C, dM4 vit.E + vit.C + LC. Changes between groups were analyzed by ANOVA and further tested by Bonferroni Post test using Graphpad Prism software; P < 0.05 was considered significant. Values within a group are represented in upper case (A, B, C). Those not sharing the same letters are significant
Glutathione peroxidase
Glutathione peroxidase (GSH-Px) activity in animals supplemented with M1 and M2 showed a significant increase (by 89% and 73%, respectively) over CON-N values. Increases in enzyme activity by one-fold in AL2 (M1) and Al1(M2) over their respective altitude normals were noted (Fig. 4a–d).
a–d Changes in glutathione peroxidase (GSH-Px) activity in erythrocytes of animals exposed to high altitude. Data are means ± SEM from five animals. CON-N Control, AL1-N Altitude 1 (5,700 m), AL2-N Altitude 2 (6,300 m). Supplements: aM1 Vitamin E (vit.E) + Vitamin C (vit.C), bM2 vit.C + l-carnitine (LC), cM3 vit.E + vit.C, dM4 vit.E + vit.C + LC. Changes between groups were analyzed by ANOVA and further tested by Bonferroni Post test using Graphpad Prism software; P < 0.05 was considered significant. Values within a group are represented in upper case (A, B, C). Those not sharing the same letters are significant
Protein oxidation
Further experiments were carried out to establish a possible link between the effects of antioxidants and stress-induced changes in the oxidation of proteins and the observed changes in membrane LPO. Membrane PrC decreased in animals exposed to altitude1 (M1, 60%; M2, 66%; M3, 52%; M4, 46%) as well to altitude2 (M1, 61%; M2, 65%; M3, 56%; M4, 48%) in relation to their respective AL-N values (Fig. 5a–d).
Changes in protein carbonyl level in erythrocytes of animals exposed to high altitude. Data are means ± SEM from five animals. CON-N Control, AL1-N Altitude 1 (5,700 m), AL2-N Altitude 2 (6,300 m). Supplements: a M1 Vitamin E (vit.E) + Vitamin C (vit.C), b M2 vit.C + l-carnitine (LC), c M3 vit.E + vit.C, d M4 vit.E + vit.C + LC. Changes between groups were analyzed by ANOVA and further tested by Bonferroni Post test using Graphpad Prism software; P < 0.05 was considered significant. Values within a group are represented in upper case (A, B, C). Those not sharing the same letters are significant
A positive correlation between PrC and hemolysis was noticed in the control (r = 0.95) and supplemented, M1 (r = 0.95), M2 (r = 0.98), M3 (r = 0.86) and M4 (r= 0.99). MDA and hemolysis also showed a positive correlation in M1 (r = 0.95), M2 (r = 0.79), M3 (r= 0.70) and M4 (r = 0.98).
Discussion
Inactivation and removal of ROS depends on reactions involving the antioxidant system, the capacity of which is determined by a dynamic interaction between individual components comprising vitamin E, vitamin C and reduced glutathione (GSH) as well as SOD, GSH-Px and CAT. The latter two form a substantial defense network against oxidative stress imposed by several other factors such as physical exercise (Asha et al. 2005; Cooper et al. 2002).
Physiological responses to high altitude hypoxia are complex and involve a range of mechanisms, some of which occur within minutes of oxygen deprivation while others result in a cascade of biosynthetic and physiological pathways within the cellular milieu. Repeated episodes of hypoxia interspersed with episodes of normoxia results in periods of intermittent hypoxia characterized by free radical production. Our present study has demonstrated that vit.E and LC as a mixture (M3) and a mixture of vit.E, vit.C and LC (M4) are more effective than vit.E and vit.C (M1) and vit.C and LC (M2).
A significant increase in the GSH-Px activity was noted in erythrocytes obtained from animals that were supplemented and exposed to IHH. These results clearly support the function of the enzyme interacting with membrane peroxides for scavenging lipid hydroperoxides. Our results showed that hemolysis is directly proportional to protein oxidation and LPO. In the present study, all the antioxidant mixtures were effective in reducing hemolysis in supplemented animals exposed to IHH.
The erythrocyte membrane encounters OS from both the interior and exterior of the cell and, regardless of the site of origin of the OS, the primary protection against peroxidative damage is through α-tocopherol, which is recycled by ascorbate. Vitamin E, a constituent of the plasma membrane, is an effective antioxidant since it is present at the site of free radical generation and can therefore neutralize the toxic effects of ROS (John et al. 2001). Vitamin E scavenges peroxide free radicals and converts them to less toxic lipid hydroperoxides, thereby protecting the cell membrane and decreasing hemolysis (Niki and Noguchi 2004).
The present findings indicating a significant decrease in fragility upon supplementation suggest that the combined effects of different antioxidants provide greater protection than single antioxidants. α-tocopherol is probably the most efficient compound in the lipid phase due to (1) its shielding methyl groups in the vicinity of the phenolic hydroxyl group of the chromane moiety, and (2) its optimal position in the membrane due to its phytyl side-chain. The maintenance of a steady-state rate of peroxyl-radical reduction by tocopherol in the membrane is dependent on the reduction of the tocopheroxyl radical, once formed, by external reductants. These include ascorbate and thiols. A typical example of synergism between antioxidants is that between glutathione regenerating ascorbate and ascorbate regenerating a-tocopherol (Ghiselli et al. 2000; Kraus et al. 1997).
Oxygen radicals formed above the detoxifying capacity of erythrocytes can cause peroxidative breakdown of phospholipid fatty acids in the erythrocyte membrane, resulting in an accumulation of TBARS (Ramazan et al. 2000). Lipofuscin accumulation leads to an accumulation of oxidatively modified proteins and lipids awaiting degradation. This pigment formation appears to be directly proportional to the occurrence of LPO, which causes an increase in osmotic fragility. Antioxidant mixtures reduced TBARS in the lysates, possibly in two ways: (1) since ascorbic acid is one of the cofactors of carnitine biosynthesis, supplementation of LC spares ascorbic acid and thereby elevates its level, (2) LC also acts as a chelator and hence decreases the amount of iron available for LPO, signifying the fact that these antioxidants act synergistically to protect the cells against OS. Since ascorbic acid, vitamin E and GSH are linked tightly to each other, the oxidizability of vitamin E is controlled by the level of endogenous antioxidants (Rani and Paneerselvam 2001). Oxidation of proteins by free radicals plays a major role in many oxidative processes within the cells, the magnitude of which is often measured by the carbonyl content (Hawkins and Davies 2001). Oxidative modification of proteins, considering their multiple functions, unlike LPO, can be selective and specific (Adams et al. 2001). It is worth noting that membrane proteins are the major targets of post-biosynthetic alterations during erythrocyte intravascular aging, a situation similar to OS, wherein increased generation of free radicals occur (Gallagher et al. 1998). Oxidative damage to a specific protein, especially at the active site, can induce a progressive loss of a particular biochemical function (Dubinina et al. 2002). Thermodynamically, vit.E and vit.C are reported to function catalytically to quench free radicals as long as cellular reducing power is available. Thus, they can act synergistically when the initiating radicals are generated within the lipid core of the membrane (Kondo et al. 1997) as shown by our results on reduced protein oxidation.
Thus, supplements of antioxidant mixtures [M4 ≈ M2 > M3 > M1] can compensate for the decline in membrane stability following IHH and this may be attributed to decreased LPO and protein oxidation. This study focused on intermittent exposure to different altitudes and subsequently validated the hematological and oxidative stress level as reliable indicators of antioxidant fortifications to offset the detrimental effects of OS. Further, the results suggest that there could be benefits from combined antioxidant fortifications in situations such as increased hemolysis and intermittent high altitude stress by protecting RBC from free radical injury.
References
Adams S, Green P, Claxton R, Simeox S, Williams MV, Walsh K et al (2001) Reactive carbonyl formation of oxidative and non-oxidative pathways. Front Biosci 6:17–24. doi:dxdoi.org/102741/Leeuwen
Asha DS, Subramanyam MVV, Vani R, Jeevaratnam K (2005) Adaptations of the antioxidant system in erythrocytes of trained adult rats: impact of intermittent hypobaric-hypoxia at two altitudes. Comp Biochem Physiol (Part C) Environment Science 140:59–67. doi:10.1016/j.cca.2005.01.003
Asha DS, Vani R, Subramanyam MVV, Reddy SS, Jeevaratnam K (2007) Intermittent hypobaric hypoxia-induced oxidative stress in rat erythrocytes: protective effects of vitamin E, vitamin C and carnitine. Cell Biochem Funct 25:221–231. doi:10.1002/cbf.1344
Bakonyi T, Radak Z (2004) High altitude and free radicals. J Sports Sci Med 3:64–69
Bernabucci U, Ronchi B, Lacetera N, Nardone A (2002) Markers of oxidative status in plasma and erythrocytes of transition dairy cows during hot season. J Dairy Sci 85:2173–2179
Cooper CE, Vollard NBJ, Choueiri T, Wilson MT (2002) Exercise, free radicals and oxidative stress. Biochem Soc Trans 30:280–285
Dodge JT, Mitchell C, Hanahan DJ (1963) The preparation and chemical characteristics of hemoglobin-free ghosts of human erythrocytes. Arch Biochem Biophys 100:119–130. doi:10:10166/0003-98963.90042-0
Dubinina EE, Gavrovskaya SV, Kuzmich EV, Leonova NV, Morozova MG, Kovrugina SV et al (2002) Oxidative modification of proteins: oxidation of tryptophan and production of dityrosine in purified proteins using fenton’s system. Biochemistry 67:343–350
Everse J, Hsia N (1997) The toxicities of native and modified hemoglobins. Free Radic Biol Med 22:1075–1099. doi:10.1016/s0891-5849(96)00499-6
Flohe L, Gunzler W (1984) Assays of glutathione peroxidase. In: Packer L (ed) Methods enzymol. Academic, Orlando, pp 114–121
Gallagher PG, Forget BG, Lux SE (1998) In: Nathan DG, Oski FA (eds) Hematology of infancy and childhood. Saunders, Philadelphia, pp 544–564
Ghiselli A, Serafini M, Natella F, Scaccini C (2000) Antioxidant capacity as a tool to assess redox status: critical view and experimental data. Free Radic Biol Med 29:1106–1114. doi:10.1015/s0891-5849(00)00394-4
Hawkins CL, Davies MJ (2001) Generation and propagation of radical reactions on proteins. Biochim Biophys Acta 1504:196–119. doi:10.1016/s0005-2728(00)00252-8
John S, Kale M, Rathore N, Bhatnagar D (2001) Protective effect of vitamin E in dimethoate and malathion induced oxidative stress in rat erythrocytes. J Nutr Biochem 12:500–504. doi:1016/s0955-2863(01)00160-7
Kraus A, Roth HP, Kirchgessner M (1997) Supplementation with vitamin C, vitamin E or β-carotene influences osmotic fragility and oxidative damage of erythrocytes of zinc-deficient rats. J Nutr 127:1290–1296
Kondo H, Takahashi M, Niki E (1997) Peroxynitrite-induced hemolysis of human erythrocytes and its inhibition by antioxidants. FEBS Lett 413:236–238. doi:10.1016/s0014-5793(97)00922-8
Lowry OH, Rosenberg NJ, Farr AL, Randall RJ (1951) Protein measurements with the Folin-phenol reagent. J Biol Chem 193:265–275. doi:10.1074/jbc.R000005200
Monji A, Morimoto N, Okuyama I, Yamashita N, Toshiro N (1994) Effect of dietary vitamin E on lipofuscin accumulation with age in the rat brain. Brain Res 634:62–68
Nagababu E, Rifkind JM (2000) Heme degradation during autoxidation of oxyhemoglobin. Biochem Biophys Res Commun 273:839–845. doi:10.1006/bbrc.2000.3025
Nagababu E, Chrest FJ, Rifkind JM (2003) Hydrogen-peroxide-induced heme degradation in red blood cells: the protective roles of catalase and glutathione peroxidase. Biochim Biophys Acta 1620:211–217. doi:10.1016/s0304-4165(02)00537-8
Niki E, Noguchi N (2004) Dynamics of antioxidant action of vitamin E. Acc Chem Res 37:45–51. doi:10.10021chin.200416265
O’Dell BL, Browning JD, Reeves PG (1987) Zinc deficiency increases the osmotic fragility of rat erythrocytes. J Nutr 117:1883–1889
Ohkawa H, Ohishi N, Yagi K (1979) Assay for lipid peroxidation in animal tissues by thiobarbituric acid reaction. Anal Biochem 95:351–358. doi:1016/0003-2697(79)90738-3
Ramazan MS, Ekeroglu SH, Dulger H, Algun E (2000) The effect of dietary treatment on erythrocyte lipid peroxidation, superoxide dismutase, glutathione peroxidase, and serum lipid peroxidation in patients with Type 2 Diabetes Mellitus. Clin Biochem 33:669–674. doi:10.1016/s0009-9120(00)00190
Rani PJA, Paneerselvam C (2001) Carnitine as a free radical scavenger in aging. Exp Gerontol 36:1713–1726. doi:10.1016/s0531-5565(01)00116-4
Senturk UK, Gunduz F, Kuru O, Aktekin MR, Kipmen D, Yalcin O et al (2001) Exercise-induced oxidative stress affects erythrocyte in sedentary rats but not exercise-trained rats. J Appl Physiol 91:1999–2004
Uchida K, Stadtman ER (1993) Covalent attachment of 4-hydroxynonenal to glyceraldehyde-3-phosphate dehydrogenase. J Biol Chem 268:6388–6393
Acknowledgments
The authors wish to acknowledge Prof. M.A. Yadugiri for editing the initial draft of this manuscript. This work was supported by grants received from the Department of Science and Technology [DST SP/SO/AS-58/2004].
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 228 kb)
Rights and permissions
About this article
Cite this article
Vani, R., Shiva Shankar Reddy, C.S. & Asha Devi, S. Oxidative stress in erythrocytes: a study on the effect of antioxidant mixtures during intermittent exposures to high altitude. Int J Biometeorol 54, 553–562 (2010). https://doi.org/10.1007/s00484-010-0304-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00484-010-0304-6