Abstract
Glomerular hyperfiltration (GHF) is an increase in single-nephron glomerular filtration rate (GFR) that occurs in both physiological states and pathological states. Whole-kidney GHF is often used as a surrogate for single-nephron hyperfiltration since determining single-nephron GFR is impossible in routine clinical care. A clear definition (read threshold) of GHF is lacking. The aim of the first part of this review was to find evidence for defining the threshold for GHF, based on literature review, including systematic reviews and meta-analysis data, with both measured and estimated GFR. The consensus pediatric threshold for GHF as obtained from reviews, measured and estimated GFR studies, can reliably be set to 135 mL/min/1.73 m2 for children aged > 2 years. Diagnosing GHF from SCr-based estimated GFR is not reliable in subjects with reduced muscle mass. In these cases, it could be of interest to confirm the state of GHF using cystatin C-based eGFR, or preferably, by measured GFR, using methods that are accurate in the high GFR-range.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glomerular hyperfiltration (GHF) is an increase in single-nephron glomerular filtration rate (GFR) that occurs in both physiological states and pathological states. Whole-kidney GHF is often used as a surrogate for single-nephron hyperfiltration since determining single-nephron GFR is impossible in routine clinical care [1]. GHF is thought to play an important role in the initiation of chronic kidney function loss, especially in the diabetic patient. GHF has not only been described in patients with diabetes mellitus [2, 3] but also in patients with sickle cell disease [4, 5], polycystic kidney disease [6], in hypertensive patients [7], and obese subjects [8] or patients experiencing the metabolic syndrome [9]. A physiological state of hyperfiltration may occur after consumption of high-protein meals [10] or during pregnancy [11]. GHF has been hypothesized to predispose to irreversible nephron damage, thereby contributing to initiation and progression of kidney disease. However, many patients reach kidney failure without going through a hyper-filtering stage [12]. GHF can start during childhood, but there is controversy about this since a clear definition of GHF is still absent. Studies have shown that higher baseline GFR is associated with faster decline in GFR over time, but whether this relationship is causal is still questionable [12, 13].
There are many factors that contribute to the difficulty in setting a clear definition (read threshold) of GHF. First, there is a lack of harmonization to measure GFR, that is, a large variety of methods are currently used to measure GFR, depending on different exogenous markers, different protocols (kidney versus plasma clearance), different timing of sampling and correction methods when only late samples are used in the concentration–time curve, and different fitting methods for the plasma-concentration versus time decay. Second, when measured GFR is not available, or cannot be measured, there exist a wide variety of estimating GFR formulas, depending on age, gender and/or height, and biomarkers like serum creatinine (SCr), cystatin C (ScysC), or the combination of both. Variations in test methods for SCr and ScysC increase the error in estimating equations. GHF status is often missed using estimated GFR (eGFR)-equations and the accuracy within 30% statistic is much too broad to ensure accurate diagnosis of GHF based on eGFR. This might suggest that the true GHF status can only be determined with directly measured GFR. Third, the natural decline in GFR with aging may obscure GHF [14]. Fourth, there are possible differences in eGFR between ethnic populations due to differences in creatinine generation [15], although current pediatric eGFR-equations do not require race [16]. Finally, the indexation by body surface area (BSA) may falsely decrease GFR in obese patients and can obscure hyperfiltration [17].
Evidence for the GHF threshold
From systematic reviews
In a first systematic review [18], the threshold for GHF was reported as ranging from 125 to 175 mL/min/1.73 m2. It was mentioned that this definition did not take into account the age-related decline of GFR after the age of 40 years. This review mentions also that GHF could either be defined as an abnormally high whole-kidney GFR, increased filtration fraction, or as increased filtration per nephron. Increased GFR can occur as an early manifestation of disease, but it remains to be proven whether GHF is a precursor of chronic kidney disease (CKD). It should be emphasized that creatinine clearance, often used as replacement for GFR, overestimates GFR by about 25% owing to tubular secretion of creatinine, and high creatinine clearance can misleadingly be confused with GHF. Also, estimating GFR-equations may be very high when serum creatinine is (very) low, and this can also misleadingly be attributed to GHF, while this may be an artifact of the estimating GFR formulae.
In a second systematic review [19], focusing on defining the GHF threshold, it was mentioned that the GHF threshold (when reported) varied between studies, ranging from 90.7 to 175 mL/min/1.73 m2, although half of GHF thresholds lie between 130 and 140 mL/min/1.73 m2. The review presented a distribution of threshold values with expression of GFR in mL/min/1.73 m2 reported in 151 studies with a single threshold. Median (minimum, maximum) was 135 mL/min/1.73 m2 (90.7, 175); first and third quartiles, 130 and 140 mL/min/1.73 m2; mean ± SD = 134.6 ± 11.7 mL/min/1.73 m2. Also, a pediatric threshold of 137.7 ± 16.1 mL/min/1.73 m2 was reported as the mean of 27 studies (see Table 1). The review mentioned that GHF thresholds reported in pediatric studies were not significantly different from studies that included mixed-age or adult populations. This may look surprising because GFR declines after the age of 40 years, at approximately 0.90 mL/min/1.73 m2/year. This implicates that the threshold for GHF is the same for everyone prior to age 40, but declines thereafter. Also, GHF thresholds according to the GFR evaluation method did not really reveal clinically relevant differences (see Table 2).
From estimating GFR formulas
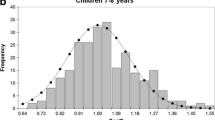
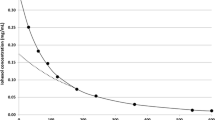
A different approach to define a GHF threshold for GFR can be based on SCr-based eGFR-formulas for children. Reference intervals for SCr vary with age and gender in children, but the so-called normalized or rescaled SCr, denoted as SCr/Q (with Q the median or mean SCr for 1-year age-/sex-specific intervals), is an interesting alternative, as it is independent of age/sex with a mean of “1” and fixed reference interval of [0.67–1.33]. This establishment forms the basis for the (pediatric form of the) full age spectrum (FAS)-equation [20]. This eGFR-equation was defined as FAS = 107.3/(SCr/Q), where the value of Q has been published in tables and formulas before [21, 22]. The lower limit or 2.5th percentile would correspond to 107.3/1.33 = 80.7, and, symmetrical to 107.3, this would be 107.3 + (107.3 – 80.7) = 107.3 + 26.6 = 133.9 mL/min/1.73 m2. The European Kidney Function Consortium (EKFC) equation is an evolution of the FAS equation, with better performance in low SCr-levels. The lower limit calculated from the EKFC-equation [23] would be 107.3 / 1.331.132 = 77.7 mL/min/1.73 m2, and symmetrically to 107.3, this would give an upper limit of 107.3 + (107.3 – 77.7) = 136.9 mL/min/1.73 m2. Note, however, that the lower limit of SCr/Q = 0.67 would result in a much higher FAS-estimation (107.3/0.67) of 160.1 mL/min/1.73 m2. The inverse relationship between GFR and SCr/Q does not allow that both variables are normally distributed (Gaussian bell shaped). Therefore, a lower limit of SCr/Q = 0.80 would correspond to a FAS-prediction close to 135 mL/min/1.73 m2, suggesting that hyperfiltration (when defined as eGFR > 135 mL/min/1.73 m2) would correspond to SCr/Q < 0.80.
However, the accuracy of creatinine for eGFR may be affected by hyperfiltration as suggested by Huang et al. [24]. These authors state that hyperfiltration should be defined as the result of an increase in the glomerular capillary pressure. Hyperfiltration should only be considered if the filtration fraction (defined as the ratio of GFR and effective renal plasma flow) is above the reference interval. The main finding of their study was that SCr-based eGFR was influenced by the filtration fraction, while this was not the case when using cystatin C or beta trace protein as kidney biomarker. They concluded that the error between eGFR as estimated from the bedside Schwartz formula and measured GFR was altered by hyperfiltration. They further concluded that SCr was a less accurate marker for eGFR in the presence of hyperfiltration. It should, however, be noted that the Schwartz formula was designed for children with CKD and is less accurate in children with normal or high GFR [25]. It can therefore be questioned whether the conclusion of their study was not an artifact of the bedside Schwartz-equation. The recently updated Schwartz equation corrects for some of the artifacts in the original bedside Schwartz equation [26]. In a study by Braat et al. [27], in 20 children with Duchenne muscular dystrophy (DMD) undergoing direct measurement of GFR (51Cr-EDTA plasma clearance), hyperfiltration (as defined by mGFR > 150 mL/min/1.73 m2) was found in 5/20 patients (note: the median mGFR was 130.4 mL/min/1.73 m2, and 9/20 patients had mGFR > 135 mL/min/1.73 m2; 19/20 patients had mGFR > 107.3 mL/min/1.73 m2, which could be considered the median reference GFR for children). In these 20 DMD children, estimating GFR from creatinine-based equations (both the bedside Schwartz equation and the pediatric FAS-equation) largely overestimated mGFR (up to 300%) due to the very low serum creatinine values in patients with reduced muscle mass, resulting in all 20 patients having eGFR > 135 mL/min/1.73 m2, that is, all being diagnosed with GHF. A similar observation was made in young women with severe anorexia nervosa [28]. Cystatin C-based eGFR-equations (like FAS = 107.3/(ScysC / 0.82)) performed much better than SCr-based eGFR-equations in these children, being closer to measured GFR, and with only 3 patients having eGFR > 135 mL/min/1.73 m2. It should also be emphasized that all 20 DMD patients had very low SCr, reflected in SCr/Q < 0.67, while all 20 DMD patients had ScysC/0.82 between 0.67 and 1.33, thus normal cystatin C values. Clearly, the very low SCr-values are mainly due to the reduced muscle mass in these patients, but the question is: when is muscle mass too low to avoid the use of SCr-based eGFR? This study, therefore, demonstrates that SCr and SCr-based eGFR-equations alone are not suited to define GHF. It must be kept in mind that SCr and GFR are inversely related (hyperbolic relationship). This means that at high GFR levels, and thus by definition in a possible state of GHF, a slight change in creatinine (for example due to analytical error) will result in a large change in GFR [29]. In other words, even if the bias of the creatinine-based equation is close to zero in a state of GHF, the imprecision remains quite large. In this context, it must be underlined that a P30 (a metric frequently used for the performance of eGFR equations and corresponding to the % of eGFR within 30% of mGFR) of 85% at the threshold for GHF (30% of 135 mL/min/1.73 m2 is 41 mL/min/1.73 m2) means that the true GFR-result has a chance of 85% to be between 94 and 176 ml/min/1.73 m2, a very broad range. It demonstrates that, at the individual level, the diagnosis of GHF in patients with reduced muscle mass based on estimated GFR can be very inaccurate.
Based on the FAS-equation, and using the upper limit 1.33 of the normalized biomarker (whether it is SCr or ScysC), a lower limit for FAS-eGFR can be defined as 107.3/1.33 (× 0.988(Age−40) if age > 40 years) = 80.7 (× 0.988(Age−40) if age > 40 years), and symmetrical to this lower limit, the upper limit is defined as 133.9 (× 0.988(Age−40) if age > 40 years). The pediatric thresholds are therefore < 80.7 for CKD and > 133.9 for GHF. The regions defined by these thresholds are illustrated in Fig. 1.
From the upper limit of measured GFR
Conventionally, GHF can be defined as a GFR of more than two standard deviations above the mean of healthy individuals. This also corresponds to the 97.5th percentile.
In a meta-analysis [30] to define mean GFR in healthy living potential kidney donors, the 2.5th and 97.5th percentiles for mGFR were obtained as mean ± 1.96 × SD for 12 studies [31] and 6 different age-groups. The means of the lower limits and upper limits with their SDs are listed in Table 3. The upper limit for young adults (20–30 years) is 136.0 ± 7.6 (mean ± SD) and can be considered a good estimate for the GHF-threshold, also for children.
In a study by Chakkera et al. [14] in 3317 potential donors, including 2125 actual donors, the overall 95th percentile for BSA-indexed measured GFR was reported as 134 mL/min/1.73 m2. They calculated an age-based threshold for mGFR expressed in mL/min/1.73 m2 as 164 – 0.730 × age, and for mGFR expressed in mL/min, it was 198 – 0.943 × age. However, they claimed that high age-based mGFR expressed in mL/min (thus not corrected for BSA) had the strongest association with higher single-nephron GFR.
To our knowledge, the study by Piepsz et al. [32] is probably the only study with measured GFR in 623 children, aged 0.1 year to 15 years, with apparently normal kidney function. They published a mean GFR of 104.4 ± 19.9 mL/min/1.73 m2 with 10th and 90th percentiles of 81 and 135 mL/min/1.73 m2, respectively, for children aged > 2 years. For infants (children younger than 2 years), the mean ± SD for measured GFR is presented in Table 4. GHF thresholds for children < 2 years of age were calculated as mean + 1.96 × SD (corresponding to the 97.5th percentile). The FAS-equation has been presented for infants by multiplying the pediatric form 107.3/(SCr/Q) with a “correction factor” of 1 – exp(–age/0.5) [20]. Upper limits calculated from this “corrected” equation are also presented in Table 4, for children aged > 1 year.
Finally, in a smaller study by Blake et al. [33] in 24 children, aged 2–17 years, with a normal scan result (99mTc-dimercaptosuccinic acid (99mTc-DMSA) scintigraphy), the reported mean GFR (± SD) was 109.5 ± 16.8 mL/min/1.73 m2, which would result in a GHF threshold of 109.5 + 1.96 × 16.8 = 142.4 mL/min/1.73 m2, very close to the reported 97.5th percentile obtained from Piepsz et al.
Conclusion
The consensus pediatric threshold for GHF as obtained from reviews, measured and estimated GFR studies, can reliably be set to 135 mL/min/1.73 m2 for children aged > 2 years. Diagnosing GHF from SCr-based estimated GFR is not reliable in subjects with reduced muscle mass. In these cases, it could be of interest to confirm the state of GHF using cystatin C-based eGFR, or preferably, by measured GFR, using methods that are accurate in the high GFR-range.
References
Denic A, Glassock RJ, Rule AD (2017) Single-nephron glomerular filtration rate in healthy adults. N Engl J Med 377:1203–1204
Tonneijck L, Muskiet MH, Smits MM, van Bommel EJ, Heerspink HJ, van Raalte DH, Joles JA (2017) Glomerular hyperfiltration in diabetes: mechanisms, clinical significance, and treatment. J Am Soc Nephrol 28:1023–1039
Molitch ME, Gao X, Bebu I, de Boer IH, Lachin J, Paterson A, Perkins B, Saenger AK, Steffes M, Zinman B; Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Research Group (2019) Early glomerular hyperfiltration and long-term kidney outcomes in type 1 diabetes: the DCCT/EDIC experience. Clin J Am Soc Nephrol 14:854–861
Haymann JP, Stankovic K, Levy P, Avellino V, Tharaux PL, Letavernier E, Grateau G, Baud L, Girot R, Lionnet F (2010) Glomerular hyperfiltration in adult sickle cell anemia: a frequent hemolysis associated feature. Clin J Am Soc Nephrol 5:756–761
Hirschberg R (2010) Glomerular hyperfiltration in sickle cell disease. Clin J Am Soc Nephrol 5:748–749
Helal I, Reed B, McFann K, Yan XD, Fick-Brosnahan GM, Cadnapaphornchai M, Schrier RW (2011) Glomerular hyperfiltration and renal progression in children with autosomal dominant polycystic kidney disease. Clin J Am Soc Nephrol 6:2439–2443
Schmieder RE, Messerli FH, Garavaglia G, Nunez B (1990) Glomerular hyperfiltration indicates early target organ damage in essential hypertension. JAMA 264:2775–2780
Chagnac A, Herman M, Zingerman B, Erman A, Rozen-Zvi B, Hirsh J, Gafter U (2008) Obesity-induced glomerular hyperfiltration: its involvement in the pathogenesis of tubular sodium reabsorption. Nephrol Dial Transplant 23:3946–3952
Tomaszewski M, Charchar FJ, Maric C, McClure J, Crawford L, Grzeszczak W, Sattar N, Zukowska-Szczechowska E, Dominiczak AF (2007) Glomerular hyperfiltration: a new marker of metabolic risk. Kidney Int 71:816–821
Bergstrom J, Ahlberg M, Alvestrand A (1985) Influence of protein intake on renal hemodynamics and plasma hormone concentrations in normal subjects. Acta Med Scand 217:189–196
Conrad KP (2004) Mechanisms of renal vasodilation and hyperfiltration during pregnancy. J Soc Gynecol Investig 11:438–448
Luyckx VA, Rule AD, Tuttle KR, Delanaye P, Liapis H, Gandjour A, Romagnani P, Anders HJ (2022) Nephron overload as a therapeutic target to maximize kidney lifespan. Nat Rev Nephrol 18:171–183
Melsom T, Nair V, Schei J, Mariani L, Stefansson VTN, Harder JL, Jenssen TG, Solbu MD, Norvik JV, Looker H, Knowler WC, Kretzler M, Nelson RG, Eriksen BO (2019) Correlation between baseline GFR and subsequent change in GFR in Norwegian adults without diabetes and in Pima Indians. Am J Kidney Dis 73:777–785
Chakkera HA, Denic A, Kremers WK, Stegall MD, Larson JJ, Ravipati H, Taler SJ, Lieske JC, Lerman LO, Augustine JJ, Rule AD (2020) Comparison of high glomerular filtration rate thresholds for identifying hyperfiltration. Nephrol Dial Transplant 35:1017–1026
Peralta CA, Katz R, DeBoer I, Ix J, Sarnak M, Kramer H, Siscovick D, Shea S, Szklo M, Shlipak M (2011) Racial and ethnic differences in kidney function decline among persons without chronic kidney disease. J Am Soc Nephrol 22:1327–1334
Levey AS, Titan SM, Powe NR, Corsh J, Inker LA (2020) Kidney disease, race and GFR estimation. Clin J Am Soc Nephrol 15:1203–1212
Delanaye P, Krzesinski JM (2011) Indexing of renal function parameters by body surface area: intelligence or folly? Nephron Clin Pract 119:c289-292
Helal I, Fick-Brosnahan GM, Reed-Gitomer B, Schrier RW (2012) Glomerular hyperfiltration: definitions, mechanisms and clinical implications. Nat Rev Nephrol 8:293–300
Cachat F, Combescure C, Cauderay M, Girardin E, Chehade H (2015) A systematic review of glomerular hyperfiltration assessment and definition in the medical literature. Clin J Am Soc Nephrol 10:382–389
Pottel H, Hoste L, Martens F (2012) A simple height-independent equation for estimating glomerular filtration rate in children. Pediatr Nephrol 27:973–979
Pottel H, Hoste L, Delanaye P (2015) Abnormal glomerular filtration rate in children, adolescents and young adults starts below 75 mL/min/1.73m2. Pediatr Nephrol 30:821–828
Pottel H (2017) Measuring and estimating glomerular filtration rate in children. Pediatr Nephrol 32:249–263
Pottel H, Bjork J, Courbebaisse M, Couzi L, Ebert N, Eriksen BO, Dalton RN, Dubourg L, Gaillard F, Garrouste C, Grubb A, Jacquemont L, Hansson M, Kamar N, Lamb EJ, Legendre C, Littmann K, Mariat C, Melsom T, Rostaing L, Rule AD, Schaeffner E, Sundin PO, Turner S, Bokenkamp A, Berg U, Asling-Monemi K, Selistre L, Akesson A, Larsson A, Nyman U, Delanaye P (2021) Development and validation of a modified full age spectrum creatinine-based equation to estimate glomerular filtration rate : a cross-sectional analysis of pooled data. Ann Intern Med 174:183–191
Huang SH, Sharma AP, Yasin A, Lindsay RM, Clark WF, Filler G (2011) Hyperfiltration affects accuracy of creatinine eGFR measurement. Clin J Am Soc Nephrol 6:274–280
Pottel H, Björk J, Delanaye P, Nyman U (2022) Evaluation of the creatinine-based chronic kidney disease in children (under 25 years) equation in healthy children and adolescents. Pediatr Nephrol. https://doi.org/10.1007/s00467-022-05429-0
Pierce CB, Munoz A, Ng DK, Warady BA, Furth SL, Schwartz GJ (2021) Age- and sex-dependent clinical equations to estimate glomerular filtration rates in children and young adults with chronic kidney disease. Kidney Int 99:948–956
Braat E, Hoste L, De Waele L, Gheysens O, Vermeersch P, Goffin K, Pottel H, Goemans N, Levtchenko E (2015) Renal function in children and adolescents with Duchenne muscular dystrophy. Neuromuscul Disord 25:381–387
Delanaye P, Cavalier E, Radermecker RP, Paquot N, Depas G, Chapelle JP, Scheen AJ, Krzesinski JM (2009) Estimation of GFR by different creatinine- and cystatin-C-based equations in anorexia nervosa. Clin Nephrol 71:482–491
Delanaye P, Cavalier E, Pottel H (2017) Serum creatinine: not so simple! Nephron 136:302–308
Pottel H, Hoste L, Yayo E, Delanaye P (2017) Glomerular filtration rate in healthy living potential kidney donors: a meta-analysis supporting the construction of the full age spectrum equation. Nephron 135:105–119
Pottel H, Delanaye P, Weekers L, Selistre L, Goffin K, Gheysens O, Dubourg L (2017) Age-dependent reference intervals for estimated and measured glomerular filtration rate. Clin Kidney J 10:545–551
Piepsz A, Tondeur M, Ham H (2006) Revisiting normal 51Cr-ethylenediaminetetraacetic acid clearance values in children. Eur J Nucl Med Mol Imaging 33:1477–1482
Blake GM, Gardiner N, Gnanasegaran G, Sabina D (2005) Reference ranges for 51Cr-EDTA measurements of glomerular filtration rate in children. Nucl Med Commun 26:983–987
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pottel, H., Adebayo, O.C., Nkoy, A.B. et al. Glomerular hyperfiltration: part 1 — defining the threshold — is the sky the limit?. Pediatr Nephrol 38, 2523–2527 (2023). https://doi.org/10.1007/s00467-022-05827-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05827-4