Abstract
Background
Lung ultrasound is a well-established technique to assess extravascular lung water, a proxy for volume status, in the adult population. Despite its utility, the data are limited supporting the use of ultrasound to evaluate fluid volume status among pediatric patients. Our study uses a simplified ultrasound protocol to evaluate changes in extravascular lung water, represented by b-lines, among pediatric patients undergoing hemodialysis.
Methods
This prospective single-center study included children from birth to 18 years of age. The number of b-lines per ml/kg of fluid removed was compared prior to, at the midpoint, and following termination of dialysis. An 8-zone protocol was utilized, and b-lines were correlated to hemoconcentration measured by the CRIT-LINE® hematocrit.
Results
Six patients with a total of 26 hemodialysis sessions were included in this study. The b-line measurements post-dialysis were 2.27 (p < 0.001; 94%CI -3.31, -1.22) lower relative to pre-dialysis. The number of b-lines was reduced by 1.69 (p < 0.001; -2.58, -0.80) between pre-dialysis and at the midpoint of dialysis and by 0.58 (p = 0.001; -0.90, -0.24) between the midpoint of dialysis and post-dialysis. A 1 mL/kg fluid loss correlated to a decrease in the original b-lines by 0.079. An inverse relationship (r = -0.54; 95% CI: -0.72, -0.34; p < 0.001) was noted between the b-lines and the patients’ hematocrit levels.
Conclusions
A simplified 8-zone ultrasound protocol can assess fluid volume change in real time and correlates with hematocrit levels obtained throughout dialysis. This provides a valuable method for monitoring fluid status in volume overloaded patient populations.
Graphical abstract

A higher resolution version of the Graphical abstract is available as Supplementary information
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The ability to accurately determine a patient’s intravascular volume status is of critical importance in the care of those with volume-sensitive disease processes such as kidney disease or heart failure. Currently, physicians primarily rely upon the clinical examination, including weight gain, skin turgor, crackles on auscultation, peripheral edema, or jugular venous distension, as well as chest X-ray, or laboratory testing. Recently, however, lung ultrasound has been utilized to evaluate for extravascular lung water and has been shown to reflect changes in water volume among adult patients undergoing routine hemodialysis in real time [1].
Lung ultrasound involves the assessment of the lungs in multiple zones for detection of several types and patterns of sonographic artifacts. Typically, 28 zones are used; however, a simplified approach has been validated in both adult and pediatric populations and may be more efficient in clinical practice [2, 3]. B-lines are vertical hyperechoic reverberation artifacts that extend from the pleural line to the bottom of the screen. Greater than three b-lines between a rib interspace suggests alveolar interstitial syndrome, and the number of b-lines allows semi-quantification of the degree of volume overload in adult populations [4, 5].
While lung ultrasound has been demonstrated to provide reliable quantification of fluid overload in adult dialysis patients, there are limited data in the pediatric population [1, 6, 7].
The primary objective of this study was to evaluate whether fluid overload can be quantified in infants and children receiving dialysis by assessing whether the number of b-lines correlates with the volume of fluid removed per kilogram of body weight using a simplified 8-zone lung ultrasound protocol. Additionally, our study aimed to evaluate the correlation between number of b-lines and blood-volume changes during treatment.
Materials and methods
This prospective observational study included pediatric patients aged birth to 18 years of age receiving hemodialysis at Arkansas Children’s Hospital. Informed consent was obtained from the subjects and/or guardians as specified in the ICMJE recommendations. Patients with lung fibrosis, interstitial lung disease, acute respiratory distress syndrome (ARDS), or multifocal pneumonia were excluded as b-lines may represent their underlying pathology rather than fluid overload. All patients had normal biventricular systolic function on echocardiogram performed concurrently with this study.
Clinical parameters, including weight, height, and vital signs, were recorded before and after each dialysis session per the routine practice at our institution. Changes in blood volume are routinely monitored during dialysis sessions as a real-time noninvasive method to guide fluid removal [8].
Hematocrit values from the CRIT-LINE® monitor (Fresenius Medical Care North America, Waltham, MA, USA) were recorded at the start, midpoint, and end of each dialysis session. Calculations of mL/kg of fluid removed were made using pre-dialysis weights.
Ultrasound details
Lung ultrasound evaluations were performed using a Mindray TE7 (Mindray North America, Mahwah, NJ). Imaging was performed by an emergency physician fellowship trained in emergency ultrasound with extensive clinical experience with lung ultrasound. The linear probe was preferentially used; however, in cases where subject body habitus prevented adequate visualization of the lung the phased array or curvilinear probe was utilized.
Participants underwent ultrasound evaluation within 30 min of starting dialysis, at the approximate midpoint of dialysis, and within 30 min of stopping dialysis. Multiple measurements were taken on each enrolled subject. The studies were performed on either Monday, Wednesday, or Friday based on scanning physician’s availability. The 8-zone protocol whereby an ultrasound probe is placed longitudinally on two anterior and two lateral fields per hemithorax was used. The anterior field was defined as anterior to the anterior axillary line, with preference given to the mid-clavicular line due to its reflection of well-aerated lung. The lateral field was defined as posterior to the anterior axillary line and anterior to the posterior axillary line with the diaphragm representing the inferior margin. B-lines were defined as hyper-echoic lines perpendicular to the probe surface and originating at the pleural line that extended to the lower limit of the field. B-lines were counted based on the moment the maximal number of b-lines was visible in each field over an entire respiratory cycle. The total number of b-lines per field and total number of b-lines in all fields were recorded.
Statistical analysis
Descriptive analyses were used to assess changes in the number of b-lines pre- to post-dialysis, stratified by the number of b-lines at baseline. To test for changes in the number of b-lines from prior to dialysis to after dialysis, we used generalized estimating equations (GEEs) with an exchangeable working correlation matrix structure to account for multiple measurements for each patient. GEE models were conducted from pre- to post-dialysis, from pre- to midpoint dialysis, and from midpoint to post-dialysis. To assess for a relationship between the number of b-lines and hematocrit levels, a repeated-measures correlation was conducted to measure the within-patient association of paired b-line and lung fluid volume measurements. Graphics were created to visualize relationships between changes in b-lines and changes in lung fluid as well as changes in b-lines and changes in hematocrit levels.
Data management and the GEE models were conducted in SAS v 9.4, the repeated-measures correlation was conducted in R, and visualizations were created in R and in Tableau Software, version 2019.2. All tests were 2-sided assuming a p value of 0.05.
Results
Demographics included patients 7–17 years of age of whom half were male. Underlying diagnoses included hemolytic uremic syndrome, congenital hypoplasia of the kidneys, obstructive uropathy and steroid-resistant nephrotic syndrome.
Of the 26 encounters, nine had 0 b-lines prior to dialysis, all of whom maintained 0 b-lines after dialysis. Only 1 encounter had an increase in b-lines, from 1 to 2. We did not find significant reductions when considering encounters with only 1 or 2 b-lines prior to dialysis. However, among encounters with 3 to 5 b-lines, the number of b-lines reduced by 3.0 for all encounters, equivalent to a 92.7% reduction from pre- to post-dialysis. Among encounters with at least 6 b-lines prior to dialysis, we found that the number of b-lines reduced by an average of 6.1 b-lines, equivalent to a 78.8% reduction (Table 1). Figure 1 displays the number of b-lines pre- and post-dialysis for the 17 encounters with > 0 b-lines prior to dialysis.
Similarly, we found that a greater number of b-lines were associated with increased average fluid removal. Specifically, we found incremental increases in fluid removed among encounters with no b-lines (32.0 ml/kg), 1 or 2 b-lines (38.1 ml/kg), 3 to 5 b-lines (44.7 ml/kg), and 6 or more b-lines (45.0 ml/kg).
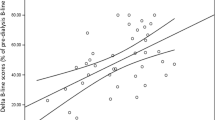
When assessing whether there were statistically significant changes in b-lines using the GEE model, we found that the b-line measurements post-dialysis were 2.27 (p < 0.001; 94%CI -3.31, -1.22) lower relative to the number of b-lines prior to dialysis. The number of b-lines was reduced by 1.69 (p < 0.001; -2.58, -0.80) between pre-dialysis and at the midpoint of dialysis, and b-lines were reduced by 0.58 (p = 0.001; -0.90, -0.24) between the midpoint of dialysis and post-dialysis. For each 1 mL/kg of fluid removed, we found a reduction in initial b-lines by 0.79 (p = 0.07) (Fig. 2).
The repeated-measures correlation used to assess the relationship between the b-lines and the patient’s hematocrit levels found a significant inverse relationship between the two measures when including all encounters (r = -0.54; 95% CI: -0.72, -0.34; p < 0.001) as well as when including those encounters with nonzero b-lines prior to dialysis (r = -0.66; 95% CI: -0.82, -0.42; p < 0.001) (Fig. 3). A 57.9-percentage-point increase in hematocrit was associated with a decrease in 1 b-line (p = 0.84) (Fig. 4).
Discussion
Our study indicates that fluid overload can be objectively quantified in infants and children receiving dialysis by investigating b-lines. Additionally, the correlation between number of b-lines and hematocrit is a novel finding from this study.
Our study quantified b-lines utilizing a simplified 8-zone protocol in the pediatric dialysis population. While lung ultrasound is a noninvasive, radiation-free technique which can easily be performed at the bedside, prior studies have utilized the 28-zone method as originally developed by Jambrik et al. or the 14-site scanning method for patients with weight < 20 kg [9]. Application of the 28-site lung ultrasound in pediatric patients can be challenging as ultrasound transducers have a relatively large footprint, which may lead to significant overlap between the scanning sites. Additionally, the 14- and 28-zone protocols require prolonged study time and manipulation of the patient’s position as compared to the simplified 8-zone method. Recently, the prognostic performance for death and cardiovascular events of the 28-site and a simplified 8-site b-lines score (4 on the right and 4 on the left hemithorax) in adult hemodialysis patients found that the two techniques were highly interrelated (Spearman’s rho 1⁄4 0.93, p < 0.001) and had a good concordance index (k 1⁄4 0.79, 95% confidence interval 0.74–0.84) [10]. As such, we sought to utilize a simplified 8-zone method in the volume assessment of pediatric dialysis patients. Our findings demonstrated a reduction in b-lines per volume of fluid removed, suggesting that this simplified protocol is sufficient to quantify fluid overload in infants and children on dialysis. Additionally, our study demonstrated the ability to detect changes in patient fluid status in real time, similar to the adult population in which b-line changes have been demonstrated to occur concurrently with ultrafiltration [1].
Our work is the first to quantify b-lines to volume per body weight of fluid removed. While Allinovi et al. and Fu et al. have previously correlated the number of b-lines with changes in body weight, our study gives a precise evaluation of volume status with regression analysis, which demonstrates a decrease in the original b-lines by 0.79 per 1 mL/kg fluid removed [7, 11]. This is of clinical importance as inadequate volume removal can lead to chronic volume overload with hypertension and left ventricular hypertrophy, which may evoke cardiovascular events and increase mortality.
Our study also expands upon prior work by Šrajer et al. who examined the association between the severity of lung congestion as detected by lung ultrasound b-lines and hematocrit in the adult population [12]. The CRIT-LINE®, a monitor which is attached to the hemodialysis blood tubing that continuously and accurately measures the hematocrit by optical absorbance, was utilized to give ongoing measure of hematocrit throughout the dialysis session [13]. Our study found a significant relationship between number of b-lines and hematocrit levels, with increases in hematocrit levels being associated with declines in b-lines.
This study of lung ultrasound as a fluid assessment tool in infants and children on dialysis had several limitations. The number of patients in our population was relatively small and was heterogeneous with respect to kidney disease. As a result, the potential for spectrum bias is an important limitation. The same physician performed all scans, and as such they were not blinded to the initial or subsequent scans and could have introduced a repeated-measures bias. Additionally, the generalizability to clinicians without extensive training and experience in lung ultrasound is not yet known. Lastly, this study was intended to have substantially more data points; however, due to the global COVID-19 pandemic, additional data collection was not able to be performed.
In conclusion, a simplified 8-zone lung ultrasound protocol can assess fluid volume status as represented by b-lines as it correlates with volume of fluid per body weight removed and hematocrit. This provides a valuable method for monitoring fluid status in volume overload pediatric patients. Future directions may include expansion and utilization of lung ultrasound and b-lines in the quantitative evaluation of volume status of other volume-sensitive populations such as those with heart failure.
References
Noble V, Murray A, Capp R, Sylvia-Reardon M, Steele D, Liteplo A (2009) Ultrasound assessment for extravascular lung water in patients undergoing hemodialysis: time course for resolution. Chest 2009:1433–1439. https://doi.org/10.1378/chest.08-1811
Enghard P, Rademacher S, Nee J, Hasper D, Engert U, Jorres A, Kruse J (2015) Simplified lung ultrasound protocol shows excellent prediction of extravascular lung water in ventilated intensive care patients. Crit Care 19:36. https://doi.org/10.1186/s13054-015-0756-5
Allinovi M, Hayes W (2021) Simplified 8-site lung ultrasound examination to assess fluid overload in children on haemodialysis. Clin Kidney J 25:1851–1852. https://doi.org/10.1093/ckj/sfab041
Lichtenstein D, Mézière G, Biderman P, Gepner A, Barré O (1997) The comet-tail artifact. An ultrasound sign of alveolar-interstitial syndrome. Am J Respir Crit Care Med 156:1640–1646
Volpicelli G, Elbarbary M, Blaivas M, Lichtenstein DA, Mathis G, Kirkpatrick AW, Melniker L, Gargani L, Noble VE, Via G, Dean A, Tsung JW, Soldati G, Copetti R, Bouhemad B, Reissig A, Agricola E, Rouby JJ, Arbelot C, Liteplo A, Sargsyan A, Silva F, Hoppmann R, Breitkreutz R, Seibel A, Neri L, Storti E, Petrovic T, International Liaison Committee on Lung Ultrasound (ILC-LUS) for International Consensus Conference on Lung Ultrasound (ICC-LUS) (2012) International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med 38:577–591. https://doi.org/10.1007/s00134-012-2513-4
Charalampos L, Pantelis S, Ferro C, Zoccali C (2021) Volume overload in hemodialysis: diagnosis, cardiovascular consequences, and management. Nephrol Dial Transplant 36:2182–2193
Allinovi M, Saleem M, Romagnani P, Nazerian P, Hayes W (2017) Lung ultrasound: a novel technique for detecting fluid overload in children on dialysis. Nephrol Dial Transplant 32:541–547. https://doi.org/10.1093/ndt/gfw037
Michael M, Brewer ED, Goldstein SL (2004) Blood volume monitoring to achieve target weight in pediatric hemodialysis patients. Pediatr Nephrol 19:432–437
Jambrik Z, Monti S, Coppola V, Agricola E et al (2004) Usefulness of ultrasound lung comets as a nonradiologic sign of extravascular lung water. Am J Cardiol 93:1265–1270. https://doi.org/10.1016/j.amjcard.2004.02.012
Torino C, Tripepi R, Loutradis C, Sarafidis P, Tripepi G, Mallamaci F, Zoccali C (2021) Can the assessment of ultrasound lung water in hemodialysis patients be simplified? Nephrol Dial Transplant 36:2321–2326
Fu Q, Chen Z, Fan J, Ling C, Wang X, Liu X, Shen Y (2021) Lung ultrasound methods for assessing fluid volume change and monitoring dry weight in pediatric hemodialysis patients. Pediatr Nephrol 36:969–976. https://doi.org/10.1007/s00467-020-04735-9
Lučič Šrajer L, Marko K, Vodošek Hojs N, Piko N et al (2021) Lung ultrasound, hemoglobin, and NT-proBNP in peritoneal dialysis patients. Clin Nephrol 96:85–88. https://doi.org/10.5414/CNP96S15
Garro R, Sutherland S, Bayes L, Alexander S, Wong C (2015) CRIT-LINE: a noninvasive tool to monitor hemoglobin levels in pediatric hemodialysis patients. Pediatr Nephrol 30:991–998. https://doi.org/10.1007/s00467-014-2986-1
Acknowledgements
The project described was supported by grant UL1 TR003107 from the Translational Research Institute (TRI) through the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Funding
The project described was supported by the grant UL1 TR003107 from the Translational Research Institute (TRI) through the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by LA, JA, and CB. The first draft of the manuscript was written by LA and PP, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
Patients signed informed consent regarding publishing their data.
Conflict of interest
None of the authors have any conflict of interest. The results presented in this paper have not been published previously in whole or part, except in abstract format.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Arthur, L., Prodhan, P., Blaszak, R. et al. Evaluation of lung ultrasound to detect volume overload in children undergoing dialysis. Pediatr Nephrol 38, 2165–2170 (2023). https://doi.org/10.1007/s00467-022-05723-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05723-x