Abstract
Background
Steroids and/or steroid-sparing medications are commonly used for nephrotic syndrome treatment; however, the impact of these medications on health-related quality of life over time is not well described.
Methods
Longitudinal cohort is up to 5 years where children were assessed with baseline and annual Pediatric Quality of Life Inventory questionnaire. A mixed-effects linear regression determined differences in scores among children receiving steroids and/or steroid-sparing agents for at least 30 days compared with those not on medication at 1, 3, 6, and 12 months prior to assessment.
Results
Among 295 children, 64% were male, with a median age of 3.7 (interquartile range [IQR], 2.7, 5.9) years at diagnosis, and comprised 25% Europeans, 40% South Asians, and 8% East/Southeast Asians. Adjusted HRQOL scores were reduced among children taking steroids and steroid-sparing agents among 705 HRQOL measures (median 2 [IQR, 1, 3] per child). Compared to children without medication, steroid and steroid-sparing agent use up to 12 months prior to assessment were associated with an overall HRQOL drop of 3.17 (95% confidence interval [CI], − 5.25, − 1.08) and 3.18 (95% CI, − 5.24, − 1.12), respectively, after adjustment. Functioning domain scores were reduced by 4.41 points (95% CI, − 6.57, − 2.25) in children on steroids, whereas fatigue domain scores were reduced by 5.47 points (95% CI, − 9.28, − 1.67) in children on steroid-sparing agents after adjustment.
Conclusions
HRQOL is consistently decreased in children receiving steroids and steroid-sparing agents, with differential effects on functioning and fatigue. Counseling families on possible effects of prolonged treatment periods is important in the management of childhood nephrotic syndrome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Childhood nephrotic syndrome is a relapsing and remitting kidney disorder defined by proteinuria, hypoalbuminemia, edema, and hypercholesteremia. Annual incidence of nephrotic syndrome is 1.15–16.9 per 100,000 children and varies by ethnicity [1,2,3]. Children with nephrotic syndrome receive glucocorticoids (steroids—commonly prednisone) as the first line of treatment at diagnosis and each relapse [4, 5]. Prolonged steroid use is associated with behavioral changes including depression, anxiety, aggression, and/or sleep disturbances [6,7,8]. We expect that the episodic relapses of nephrotic syndrome and intermittent treatments may not necessarily be detrimental to a child’s health-related quality of life (HRQOL); however, this hypothesis has not been tested longitudinally. Assessment of the HRQOL score among children with nephrotic syndrome over time will allow clinicians and families to better understand the specific impact of medications on quality of life and seek appropriate counseling interventions [9]. Moreover, steroids are commonly used for many pediatric chronic diseases; thus, findings can impact other affected children.
Several studies have reported lower social competency and behavioral disturbances in children with nephrotic syndrome [7, 10,11,12,13,14,15]. These studies included selected cases of children with nephrotic syndrome who had undergone biopsy, or had advanced focal segmental glomerulosclerosis approaching kidney failure. Also, these studies had small study populations with limited power or were cross-sectional in design. In a study of 127 children with nephrotic syndrome, there was an observed association of disease duration and quality of life; however, differences in types of symptoms between incident and prevalent children were not described [14]. This cross-sectional study did not provide comprehensive assessment of medication exposure over time. Additional factors that were not studied which may negatively influence quality of life in children with nephrotic syndrome include medication exposure, steroid dependency, and frequency of relapse [11,12,13, 15]. Most studies to date have focused on the association of steroid use with behavior. Few studies have assessed other aspects of HRQOL secondary to the effect of steroid-sparing agent use, which is critical to fully understand the spectrum of medication effects [16, 17]. For instance, sleep disturbances may impact daily functioning, which could lead to interruptions in schooling and everyday physical activities, critical to child development.
Understanding the effects of nephrotic syndrome treatment, either steroids or steroid-sparing agents, on a child’s HRQOL will provide information to clinicians, which can be used to develop counseling strategies and inform parents on how to address these issues. We sought to determine the effects of treatments commonly used in other childhood chronic diseases on a child’s HRQOL over the clinical course of the disease, and the impact of steroids and steroid-sparing agents on HRQOL overall and by specific domains.
Methods
Study design and population
Insight into Nephrotic Syndrome: Investigating Genes, Health, and Therapeutics (INSIGHT) is a cohort study established in 2011 at The Hospital for Sick Children (SickKids) in Toronto, Canada. Recruitment for the INSIGHT has been reported previously [18]. We assessed HRQOL at time of enrollment and annually up to 5 years using the age-appropriate Pediatric Quality of Life Inventory—Version 4 (PedsQL-V4), a validated questionnaire to assess subject’s quality of life in the past month [19]. A total of 325 incident and prevalent children with nephrotic syndrome were enrolled from February 2011 to December 2015 and completed an initial questionnaire. Participants were recruited from within the Greater Toronto Area. Children between 1 and 18 years of age were enrolled if able to provide informed assent and/or consent, and willing to complete questionnaires at baseline and annually. Participants were excluded from the study if they had disease with multiple organ involvement, conditions such as systemic lupus erythematosus or vasculitis, and/or biopsy-proven membranous glomerulonephritis, or membranoproliferative glomerulonephritis [18]. Of the 325 study participants, 30 were excluded due to limited longitudinal follow-up, resulting in a final cohort of 295 participants. SickKids Research Ethics Board approved the study.
Exposure—steroids and steroid-sparing agents
Medication data were collected from electronic medical records at baseline and annually. As per standard clinical protocol for nephrotic syndrome at SickKids, all children were treated with steroids (either prednisone or prednisolone) at clinical presentation, involving a 16-week regimen of 60 mg/m2 per day for 6 weeks (~ 42 days) followed by an alternate day taper for 10 weeks (~ 70 days). The regimen for relapses consists of ~ 48 days of medication after entering remission, defined as negative protein for 5 consecutive days [2]. Based on common treatment protocol, all children were typically prescribed 16 weeks (~ 112 days) for initial therapy and a minimum of 8 weeks (~ 53 days) for a relapse [2]. Use of second-line medication was defined as prescribed steroid-sparing agent for the treatment of nephrotic syndrome in steroid-resistant, frequently relapsing, or steroid-dependent cases. Steroid-sparing agents included calcineurin inhibitors (tacrolimus, cyclosporine), oral cyclophosphamide, and mycophenolate mofetil (MMF)/mycophenolate sodium. Participants were grouped by medication exposure, based on a minimum of at least 30 days on a medication up to 1, 3, 6, and 12 months prior to HRQOL assessment. These lag times were established to understand the duration of medication use prior to assessment [20]. Medication use was categorized into those on no medication, steroids alone, both steroids and one or more steroid-sparing agent(s), and those on one or more steroid-sparing agent(s).
Outcome—health-related quality of life
HRQOL was measured at baseline and annually via self-report or parental report using PedsQL-V4 [19]. The PedsQL evaluates five domains: physical functioning, emotional functioning, social functioning, educational functioning, and fatigue (general, sleep, and cognitive). Questions were answered on a 5-point Likert scale (0–4; 0 = never a problem, 4 = almost always a problem) and were reverse-scored and linearly transformed to a 0–100 point scale (0 = 100, 1 = 75, 2 = 50, 3 = 25, 4 = 0), with higher scores signifying a relatively greater HRQOL as per PedsQL standard scaling and scoring [19]. For reference, healthy children have been shown to score 84 points on average [21]. As per standard PedsQL protocol, educational functioning data were not captured during the summer months; thus, < 3% of the remaining PedsQL questionnaire data were missing based on timing of clinic visits. Questionnaire score data were averaged by domain and by total score to account for any missing data during the summer months.
Covariates
Covariates included age at diagnosis (years), sex, ethnicity, income, relapse rates, initial steroid resistance, and duration from diagnosis to enrollment (years). Ethnicity was based on self-report of grandparents’ ancestries classified as per Statistics Canada’s definitions. Self-reported family income data was dichotomized based on Statistics Canada’s low-income cut-off score of $35,000 [22]. Frequent relapses were defined as ≥ 2 relapses in the 6 months or ≥ 4 relapses during the 12 months prior to HRQOL assessment. Initial steroid resistance was defined as use of a steroid-sparing agent during the initial steroid course [2]. Data were obtained through administered questionnaires, self-report, and electronic medical records, and were validated using double-data entry.
Statistical analysis
Clinical and demographic characteristics were represented using means (standard deviation [SD]) and medians (interquartile range [IQR]). HRQOL was assessed by comparing PedsQL questionnaire data between children, focusing on total and specific domain scores. Mixed-effects linear regression was used to determine the association between immunosuppressive medications and HRQOL scores, accounting for multiple measures per child over time. Models were adjusted for confounders determined a priori: age at diagnosis (years), sex, ethnicity, income, frequent relapses, initial steroid resistance, and duration from diagnosis to enrollment. Additional analyses were conducted to assess improvements in HRQOL scores after discontinuation of medication. All statistical analyses were conducted using STATA 14 (Stata-Corp, College Station, TX, USA) and a p value ≤ 0.05 was considered statistically significant.
Results
Participants
Participants were actively followed for up to 5 years as part of the longitudinal study with variable follow-up; 289 assessed at baseline, 194 at 1 year, 132 at 2 years, 68 at 3 years, and 22 at 4 years of follow-up. Among the 295 children with incident and prevalent nephrotic syndrome, the cohort was predominantly male, and median age at diagnosis was 4 years with a median duration from diagnosis to enrollment of 1.5 years (Table 1). The majority of families were above the low-income cut-off and came from ethnically diverse ancestries including European, South Asian, and Southeast Asian (Supplementary data, Table S1). At study enrollment, the majority of participants were on steroids and, at subsequent annual visits, were not taking any medications. In the 12 months prior to enrollment, 33.9% were on no medications, 46.1% were on steroids, 5.5% were on steroid-sparing agents, and 14.5% were on both steroids and steroid-sparing agents.
Cumulative medication exposure
At 1, 3, 6, and 12 months prior to assessment, the proportion of children on steroids decreased throughout follow-up. In contrast, the proportion on steroid-sparing agents increased at each annual visit. Across the 1-, 3-, and 6-month time spans prior to HRQOL assessment and during each annual visit, most children were not taking any medication. Those on steroids at 1, 3, 6, and 12 months prior to assessment were on treatment for a median of 30, 57, 93, and 108 days, respectively (Supplementary data, Table S2). Generally, median cumulative exposure in the 12 months prior to questionnaire administration among children on steroids was approximately 2.5 months. Among children on steroid-sparing agents in the 12 months prior to HRQOL assessment, average medication exposure was 1 year consistently across all visits.
Overall health-related quality of life
The average total HRQOL score was 86.9 out of 100 at baseline and increased to 90.2 by the 4th year of follow-up (Table 1). We had a total of 705 measures with a median of 2 (IQR, 1, 3) measures per child. More than 99% of HRQOL data comprised parental answers to the PedsQL questionnaire. Prior to HRQOL assessment, steroid use up to 6 months was associated with a decrease in the overall HRQOL score, reflecting a worse HRQOL, but the difference was not statistically significant even after adjustment (Table 2). Taking steroids up to 12 months prior to HRQOL assessment was associated with a drop in the overall HRQOL score ranging from 1.08 to 5.25, which remained significant after controlling for age at diagnosis, sex, ethnicity, income status, frequent relapses, initial steroid resistance, and duration from diagnosis to enrollment.
Among children on steroid-sparing agents, overall HRQOL score was significantly reduced by 0.18–6.02 at 6 months of medication exposure when compared with those on no medication, and remained significant even after adjustment. Similar estimates were seen at the 12-month lag time even after adjustment. Consistent patterns with medication exposure for only 1 and 3 months prior to HRQOL assessment were seen; however, the decrease was modestly lower (Supplementary data, Table S3). The combination of steroid-sparing agents and steroids was associated with a similar decrease in HRQOL scores ranging from 1.26 to 7.46 in the 6 months prior to assessment and the association was attenuated after adjustment.
Health-related quality of life scores by functioning and fatigue domains
Children on steroids had a significant reduction in the functioning domains of the HRQOL score (physical, emotional, social, and educational functioning). The functioning domain scores were even lower at 12 months compared with 6 months of exposure (Table 3). Steroid-sparing agents had no association with functioning domains. Additionally, there was no significant association with fatigue domains (general, sleep, and cognitive fatigue) among children taking steroids in the 6 and 12 months prior to HRQOL assessment as compared with those on no medication. Use of steroid-sparing agents, however, did have a significant association with fatigue domains at both 6 and 12 months prior to HRQOL assessment with decreased scores from as low as 1.41 to as high as 9.05 after adjustment.
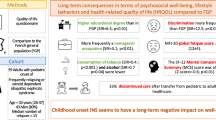
In Fig. 1, we demonstrate that general, sleep, and cognitive fatigue are consistently affected by steroid-sparing agents but not steroids. There was also no clear additive effect of the combination of both steroids and steroid-sparing agents. Various functioning domains were predominantly affected by steroids, especially the educational, social, emotional, and physical subdomains at 12 months. This association was not significant at 6 months. (Supplementary data, Fig. 1; Table S2). The largest decrease in HRQOL score was observed for sleep fatigue in those using steroid-sparing medication.
Average HRQOL score change by domain for each medication group, duration up to 6 months (panel a) and 12 months (panel b) prior to the assessment: Models were adjusted for participant age at diagnosis, sex, ethnicity, frequent relapses, initial steroid resistance, income, and duration from diagnosis to enrollment
Additional analyses were performed to assess changes in HRQOL score after discontinuing medication. At any given time point, 54 children went from taking steroids at one visit to not taking any medication for the full year prior to the subsequent visit. The overall HRQOL scores improved by a median of 4.28 (IQR, − 3.93, 12.89). In children who went from steroid-sparing agents to no medications (n = 12), a median score increase of 7.46 (IQR, − 1.59, 19.67) was observed. Moreover, children who changed medication status from steroids and steroid-sparing agents to no medications (n = 12) were found to have a median score increase of 2.14 (IQR, − 4.21, 8.13).
Discussion
This study evaluated the impact of medications on HRQOL in children with nephrotic syndrome and demonstrated a reduction in overall HRQOL up to 5% for both steroid and steroid-sparing agents among a large and diverse cohort of children with incident and prevalent nephrotic syndrome. We extend prior findings of the impact of steroids on behavior and show that extended use of steroids results in a significant reduction in physical, emotional, social, and educational functioning. We also demonstrate a significant, consistent, and independent association between steroid-sparing agent use and HRQOL overall, and specifically with general fatigue, sleep, and cognition. Interestingly, these findings suggest that while steroids predominantly yield adverse physical events, steroid-sparing agents negatively impact fatigue in childhood nephrotic syndrome. We also found that short periods of steroid and/or steroid-sparing medication affects HRQOL, but longer periods over 6 months results in significantly lower scores.
Notably, our study cohort had an overall healthier mean HRQOL score of 86, which is slightly higher than that of healthy children of 84, and considerably higher than that of children suffering from chronic illness such as cancer, kidney failure, and diabetes whose scores range between 71 and 81 [21]. Our study population, as previously described, may represent a generally healthier group of children with very few having advanced kidney disease unlike other cohorts reported. Furthermore, we have shown previously a higher health literacy reported than in the USA among parents of children with chronic disease, and perhaps healthier overall given the access to universal healthcare [23]. The nature of nephrotic syndrome along with its continuous management and monitoring contributes to interruptions in daily activities and functioning. We demonstrated a significant and independent association of steroid-sparing agents irrespective of 1, 3, 6, or 12 months duration with a reduction in the general, sleep, and cognitive fatigue domains, as children who were reported to be noticeably tired throughout the day have difficulty sleeping throughout the night or experience difficulty remaining attentive, or difficulty with memory. Often, children with nephrotic syndrome are given steroid-sparing agents to avoid the toxic side effects of prolonged steroid use, such as obesity, poor growth, and hypertension; however, little is known about the impact of steroid-sparing agents on HRQOL [24]. The effect on HRQOL has not been reported previously despite the frequent use of steroid-sparing agents in numerous conditions such as inflammatory bowel disease or lupus. Interestingly, there was no evidence of an additive effect of taking a combination of steroids and steroid-sparing medication on HRQOL.
Steroids significantly affect physical, emotional, social, and educational functioning domains, especially in children taking medication for greater than 2 months. Reduced physical functioning scores would commonly present as impairment of daily activities such as running or playing, in comparison with children of the same age. Lower emotional and social functioning scores suggest that the child is experiencing emotional disturbances affecting mood and may have difficulty socializing with other children. A relatively lower educational functioning score would indicate that the child may have poorer school performance and a high rate of school absences due to conflicting medical appointments or feeling too unwell to attend. Prior studies have demonstrated an association with steroids and aggressive behavior [7, 8, 25, 26]. A prospective study of 10 children with steroid-sensitive nephrotic syndrome followed for 16 months found a strong correlation between steroid dose and behavior, particularly aggression [26]. Similarly, another report in 12 children on steroids highlighted the significant negative impact on behavior, specifically aggression and attention. Further, they also identified the negative association between steroids and school performance [7]. Our results demonstrate a significant reduction in emotional functioning in children on steroids. Moreover, we demonstrate that longer medication exposure results in a greater reduction in HRQOL score. We had repeated measures in many children whereas the majority of previous studies used only a single measure [8, 12, 15, 16, 26, 27].
Numerous questionnaires, including the PedsQL, Child Behavior Checklist, PROMIS, Child Health Utility 9D, and Children Depression Inventory, have been previously used to assess HRQOL changes in children with nephrotic syndrome [7,8,9, 11, 15,16,17, 27,28,29]. Most questionnaires focus on specific aspects of HRQOL and require more time for the detailed assessments. Our study assessed HRQOL with a standardized and validated measure: the Pediatric Quality of Life Inventory—Version 4, which was chosen based on the specific domains and the ability to screen given time constraints during annual clinical assessments. Although, the PedsQL serves as an excellent screening tool to assess HRQOL overall, other questionnaires such as the PROMIS measurement provide a more in-depth evaluation of domains, such as aggressive behavior, anxiety, and depression to thoroughly assess specific gaps in literature [7]. In a recent study of 151 children with prevalent nephrotic syndrome, PROMIS effectively discriminated between children and adolescents with active and inactive nephrotic syndrome, and was found to be an accurate tool for thoroughly assessing HRQOL; however, this tool did not assess all aspects of HRQOL [29]. Our study extends the current findings, showing a significant correlation of steroid use and duration with physical, emotional, social, and educational functioning domains that may significantly impact daily activities and functioning.
Impact on HRQOL may not only be a result of the disease activity but also duration of medication. This is especially relevant for diseases such as nephrotic syndrome, where the episodic nature of relapses and remissions results in ongoing management and treatment with repeated courses or maintenance immunosuppressive medication. Most studies have focused on disease duration and not duration of medication exposure when assessing behavior and quality of life [8, 14, 30, 31]. In our study, longer use of steroid medication led to a proportionally lower HRQOL, and in contrast, steroid-sparing agents reduced HRQOL regardless of the duration of treatment. This suggests that duration of treatment may be a factor to consider when using steroids. In the few children that were not on any medication at their subsequent follow-up visit, we observed an increase in HRQOL score, suggesting a direct relationship between medication and HRQOL.
Additional factors that confound the association of medication and HRQOL include frequent relapses and initial steroid resistance; however, our findings remained consistent even after adjustment with little attenuation. The results were robust and indicate an independent association of medications and HRQOL specifically independent of relapsing disease. There may be, however, confounding by indication, as those on steroid-sparing agents are presumed to have frequently relapsing disease or steroid resistance.
The strengths of this study include the large, ethnically diverse cohort, consisting of both incident and prevalent nephrotic syndrome patients with over 700 repeated measures of HRQOL for up to 5 years. We were able to adjust for severity of disease (initial steroid resistance and frequently relapsing status) and duration of medication exposure. Limitations of our study include potential residual confounding from environmental or social factors not captured at the time of questionnaire completion such as moving to a new house or changing schools. Additionally, parent recall bias may be a limitation; however, this is similar to other types of questionnaires. The study also had limited educational functioning data during summer-break months as children were not in school. As there is a relatively low incidence of hypertension and steroid-related side effects in our patients, these factors were not included in the analyses. Although there is data available to assess other factors and their impact on quality of life, our main objective was to address parental observations of chronic medication exposure on physical functioning, emotional functioning, social functioning, and educational functioning and fatigue (general, sleep, and cognitive). Furthermore, given standard treatment protocols [2], our population has a limited number of children treated with rituximab and therefore did not analyze the effects of rituximab on HRQOL; however, a recent study found the QOL in children with nephrotic syndrome treated with rituximab was comparable with those treated with oral steroid-sparing agents [32].
Medications necessary for treatment of childhood nephrotic syndrome play a key role in lowering HRQOL that is not entirely attributable to disease activity. Exposure to both steroids and/or steroid-sparing agents significantly reduces HRQOL with differential effects on specific domains. Our results emphasize the importance of addressing physical and psychosocial needs of children with nephrotic syndrome on steroids and/or steroid-sparing agents on an ongoing basis throughout the duration of therapy. Furthermore, our results can aid in identifying children on steroids and/or steroid-sparing agents who may be at risk for a poor quality of life and employ preventative and therapeutic interventions as well as provide informative counseling on the effects of prescribed medications to the families.
Data availability
The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
References
Eddy AA, Symons JM (2003) Nephrotic syndrome in childhood. Lancet 362:629–639
Banh TH, Hussain-Shamsy N, Patel V, Vasilevska-Ristovska J, Borges K, Sibbald C, Lipszyc D, Brooke J, Geary D, Langlois V, Reddon M, Pearl R, Levin L, Piekut M, Licht CP, Radhakrishnan S, Aitken-Menezes K, Harvey E, Hebert D, Piscione TD, Parekh RS (2016) Ethnic differences in incidence and outcomes of childhood nephrotic syndrome. Clin J Am Soc Nephrol 11:1760–1768
Noone DG, Iijima K, Parekh R (2018) Idiopathic nephrotic syndrome in children. Lancet 392:61–74
Trompeter RS, Lloyd BW, Hicks J, White RH, Cameron JS (1985) Long-term outcome for children with minimal-change nephrotic syndrome. Lancet 1:368–370
Greenbaum LA, Benndorf R, Smoyer WE (2012) Childhood nephrotic syndrome--current and future therapies. Nat Rev Nephrol 8:445–458
Neuhaus TJ, Langlois V, Licht C (2010) Behavioural abnormalities in children with nephrotic syndrome--an underappreciated complication of a standard treatment? Nephrol Dial Transplant 25:2397–2399
Hall AS, Thorley G, Houtman PN (2003) The effects of corticosteroids on behavior in children with nephrotic syndrome. Pediatr Nephrol 18:1220–1223
Youssef DM, Abdelsalam MM, Abozeid AM, Youssef UM (2013) Assessment of behavior abnormalities of corticosteroids in children with nephrotic syndrome. ISRN Psychiatry 2013:921253
Mishra K, Ramachandran S, Firdaus S, Rath B (2015) The impact of pediatric nephrotic syndrome on parents’ health-related quality of life and family functioning: an assessment made by the PedsQL 4.0 family impact module. Saudi J Kidney Dis Transpl 26:285–292
Vance JC, Pless IB (1983) The effect of chronic nephrotic syndrome on the affected child. J Dev Behav Pediatr 4:159–162
Mehta M, Bagga A, Pande P, Bajaj G, Srivastava RN (1995) Behavior problems in nephrotic syndrome. Indian Pediatr 32:1281–1286
Ruth EM, Landolt MA, Neuhaus TJ, Kemper MJ (2004) Health-related quality of life and psychosocial adjustment in steroid-sensitive nephrotic syndrome. J Pediatr 145:778–783
Guha P, De A, Ghosal M (2009) Behavior profile of children with nephrotic syndrome. Indian J Psychiatry 51:122–126
Selewski DT, Troost JP, Massengill SF, Gbadegesin RA, Greenbaum LA, Shatat IF, Cai Y, Kapur G, Hebert D, Somers MJ, Trachtman H, Pais P, Seifert ME, Goebel J, Sethna CB, Mahan JD, Gross HE, Herreshoff E, Liu Y, Song PX, Reeve BB, DeWalt DA, Gipson DS (2015) The impact of disease duration on quality of life in children with nephrotic syndrome: a Midwest Pediatric Nephrology Consortium study. Pediatr Nephrol 30:1467–1476
Soliday E, Moore KJ, Lande MB (2002) Daily reports and pooled time series analysis: pediatric psychology applications. J Pediatr Psychol 27:67–76
Manti P, Giannakopoulos G, Giouroukou E, Georgaki-Angelaki H, Stefanidis CJ, Mitsioni A, Stergiou N, Mihas C, Chrousos GP, Magiakou MA, Kolaitis G (2013) Psychosocial and cognitive function in children with nephrotic syndrome: association with disease and treatment variables. Biopsychosoc Med 7:10
Gipson DS, Trachtman H, Kaskel FJ, Radeva MK, Gassman J, Greene TH, Moxey-Mims MM, Hogg RJ, Watkins SL, Fine RN, Middleton JP, Vehaskari VM, Hogan SL, Vento S, Flynn PA, Powell LM, McMahan JL, Siegel N, Friedman AL (2011) Clinical trials treating focal segmental glomerulosclerosis should measure patient quality of life. Kidney Int 79:678–685
Hussain N, Zello JA, Vasilevska-Ristovska J, Banh TM, Patel VP, Patel P, Battiston CD, Hebert D, Licht CP, Piscione TD, Parekh RS (2013) The rationale and design of Insight into Nephrotic Syndrome: Investigating Genes, Health and Therapeutics (INSIGHT): a prospective cohort study of childhood nephrotic syndrome. BMC Nephrol 14:25
Varni JW, Seid M, Kurtin PS (2001) PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care 39:800–812
Gasparrini A (2014) Modeling exposure–lag–response associations with distributed lag non-linear models. Stat Med 33:881–899
Varni JW, Limbers CA, Burwinkle TM (2007) Impaired health-related quality of life in children and adolescents with chronic conditions: a comparative analysis of 10 disease clusters and 33 disease categories/severities utilizing the PedsQL 4.0 Generic Core Scales. Health and quality of life outcomes 5:43
Statistics Canada (2012) In: Low income lines, 2010 to 2011. Industry (ed). Ottawa: Authority of the Minister Responsible for Statistics Canada. pp 28–30
Borges K, Sibbald C, Hussain-Shamsy N, Vasilevska-Ristovska J, Banh T, Patel V, Brooke J, Piekut M, Reddon M, Aitken-Menezes K, McNaughton A, Pearl RJ, Langlois V, Radhakrishnan S, Licht CPB, Piscione TD, Levin L, Noone D, Hebert D, Parekh RS (2017) Parental health literacy and outcomes of childhood nephrotic syndrome. Pediatrics 139:e20161961
Zhang H, Wang Z, Dong LQ, Guo YN (2016) Children with steroid-resistant nephrotic syndrome: long-term outcomes of sequential steroid therapy. Biomed Environ Sci 29:650–655
Ghobrial EE, Fahmey SS, Ahmed ME, Botrous O (2013) Behavioral changes in Egyptian children with nephrotic syndrome. Iran J Kidney Dis 7:108–116
Soliday E, Grey S, Lande MB (1999) Behavioral effects of corticosteroids in steroid-sensitive nephrotic syndrome. Pediatrics 104:e51
Soliday E, Kool E, Lande MB (2000) Psychosocial adjustment in children with kidney disease. J Pediatr Psychol 25:93–103
Webb NJ, Frew E, Brettell EA, Milford DV, Bockenhauer D, Saleem MA, Christian M, Hall AS, Koziell A, Maxwell H, Hegde S, Finlay ER, Gilbert RD, Booth J, Jones C, McKeever K, Cook W, Ives NJ, PREDNOS 2 study group (2014) Short course daily prednisolone therapy during an upper respiratory tract infection in children with relapsing steroid-sensitive nephrotic syndrome (PREDNOS 2): protocol for a randomised controlled trial. Trials 15:147
Gipson DS, Selewski DT, Massengill SF, Wickman L, Messer KL, Herreshoff E, Bowers C, Ferris ME, Mahan JD, Greenbaum LA, MacHardy J, Kapur G, Chand DH, Goebel J, Barletta GM, Geary D, Kershaw DB, Pan CG, Gbadegesin R, Hidalgo G, Lane JC, Leiser JD, Plattner BW, Song PX, Thissen D, Liu Y, Gross HE, DeWalt DA (2013) Gaining the PROMIS perspective from children with nephrotic syndrome: a Midwest pediatric nephrology consortium study. Health Qual Life Outcomes 11:30
Rahman M, Afroz S, Ali R, Hanif M (2016) Health related quality of life in children with nephrotic syndrome in Bangladesh. Mymensingh Med J 25:703–709
Agrawal S, Krishnamurthy S, Naik BN (2017) Assessment of quality of life in children with nephrotic syndrome at a teaching hospital in South India. Saudi J Kidney Dis Transpl 28:593–598
Roussel A, Delbet JD, Micheland L, Deschenes G, Decramer S, Ulinski T (2019) Quality of life in children with severe forms of idiopathic nephrotic syndrome in stable remission-a cross-sectional study. Acta Paediatr 108:2267–2273
Acknowledgments
We thank the participants and their families for their time and effort as well as the nurses and staff from the Nephrology Clinic at The Hospital for Sick Children and William Osler Health System (Brampton Civic Hospital and Peel Memorial Centre, Brampton, ON, Canada). We also thank Richard Child for his advice and insight into the electronic patient record.
Funding
This study received financial support from The Hospital for Sick Children Research Institute, Physicians’ Services Incorporated (grant number N/A [to R.S.P]); Canada Research Chair in CKD epidemiology; Canada Research Chairs Program. RSP is funded by the Canada Research Chair in CKD epidemiology. This research was undertaken, in part, thanks to the Canada Research Chairs program for funding.
Author information
Authors and Affiliations
Contributions
Shawn Khullar drafted the initial manuscript.
Corresponding author
Ethics declarations
SickKids Research Ethics Board approved the study.
Disclaimer
The study sponsor had no role in the study design, data collection, data analysis, data interpretation, writing of the report, or in the decision to submit the paper for publication. No honorarium, grant, or other form of payment was given to anyone to produce the manuscript.
Conflict of interest
The authors declare that they have no conflicts of interest
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 47 kb)
Rights and permissions
About this article
Cite this article
Khullar, S., Banh, T., Vasilevska-Ristovska, J. et al. Impact of steroids and steroid-sparing agents on quality of life in children with nephrotic syndrome. Pediatr Nephrol 36, 93–102 (2021). https://doi.org/10.1007/s00467-020-04684-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-020-04684-3