Abstract
Secondary hyperparathyroidism is part of the complex of chronic kidney disease-associated mineral and bone disorders (CKD-MBD) and is linked with high bone turnover, ectopic calcification, and increased cardiovascular mortality. Therefore, measures for CKD-MBD aim at lowering PTH levels, but there is no general consensus on optimal PTH target values. This manuscript is part of a pros and cons debate for keeping PTH levels within the normal range in children with CKD, focusing on the cons. We conclude that a modest increase in PTH most likely represents an appropriate adaptive response to declining kidney function in patients with CKD stages 2–5D, due to phosphaturic effects and increasing bone resistance. There is no evidence for strictly keeping PTH levels within the normal range in CKD patients with respect to bone health and cardiovascular outcome. In addition, the potentially adverse effects of PTH-lowering measures, such as active vitamin D and calcimimetics, must be taken into account. We suggest that PTH values of 1–2 times the upper normal limit (ULN) may be acceptable in children with CKD stage 2–3, and that PTH levels of 1.7–5 times UNL may be optimal in patients with CKD stage 4–5D. However, standard care of CKD-MBD in children relies on a combination of different measures in which the observation of PTH levels is only a small part of, and trends in PTH levels rather than absolute target values should determine treatment decisions in patients with CKD as recommended by the 2017 KDIGO guidelines.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
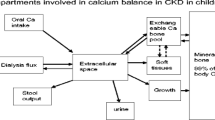
Secondary hyperparathyroidism (SHPT) is part of the complex chronic kidney disease-associated mineral and bone disorders (CKD-MBD) [1]. In early CKD, high plasma fibroblast growth factor 23 (FGF23) is the earliest detectable abnormality in mineral metabolism (Fig. 1) [2, 3]. FGF23 serum levels start to rise as early as CKD stage 2, most likely due to elevated phosphate load, in order to keep serum phosphate levels within the normal range by decreasing renal phosphate reabsorption and inhibiting renal synthesis of active vitamin D, which in turn reduces phosphate reabsorption from the gut. In addition, low levels of Klotho—the co-receptor for FGF23—may partially induce FGF23 resistance, resulting in a compensatory increase in FGF23 serum levels to maintain phosphate homeostasis. However, as renal function further declines calcitriol deficiency results in hypocalcemia which stimulates, together with an increasing phosphate load, the synthesis of parathyroid hormone (PTH) by the parathyroid gland [2]. Increased PTH stimulates phosphaturia, renal 1α-hydroxylase, and calcium resorption from the bone [4]. Indeed, elevated PTH levels are present in about 50% of pediatric CKD patients with an estimated glomerular filtration rate (eGFR) < 50 ml/min/1.73m2 [3]. This allows the body to counterbalance calcitriol deficiency-induced hypocalcemia and to keep serum phosphate levels within the normal range despite advanced CKD until the system decompensates and severe complications of CKD-MBD occur, i.e., renal osteodystrophy including bone pain, fractures, rickets, leg deformities, and growth failure, as well as ectopic calcification. Severe SHPT is associated with high bone turnover, ectopic calcification, anemia, left ventricular hypertrophy, and increased mortality [5,6,7,8,9,10,11]. However, recommended CKD stage-dependent PTH target range values differ widely (Table 1) [12,13,14,15,16]. The European Dialysis Working Group of the ESPN recommend that PTH levels should be maintained within normal limits in children with GFR > 29 ml/min/1.73m2, and within 2–3 times the upper normal limit (UNL) in CKD stages 4–5D [14]. By contrast, the US-based K/DOQI guidelines recommend a target range of 3–5 times the UNL in CKD stage 5 [12]. The Kidney Disease: Improving Global Outcomes (KDIGO) guidelines recommend a PTH target range of 2–9 times the UNL in CKD stage 5D, but the higher end of the range is rarely deemed acceptable in pediatric bone care [13]. However, most importantly is the acknowledgment that none of these recommendations have been validated in a large pediatric CKD cohort study/investigation. Most recently, data from the International Pediateric Dialysis Network (IPPN) has suggested that an optimal PTH target range of 1.7–3 times UNL in pediatric peritoneal dialysis patients is associated with lower CKD-MBD complications, such as growth failure [15]. This manuscript is based on the pros and cons debate held at the 51st Annual Scientific Meeting of the European Society for Paediatric Nephrology in Antalya in 2018 on the question of whether normal PTH levels should be aimed for in children with CKD, focusing on the cons.
Proposed time profile of changes in blood phosphate, calcium, Klotho, and hormones relevant to mineral metabolism in chronic kidney disease (CKD). The decrease in Klotho protein in the kidney and blood is an early event in CKD and is sustainably and progressively reduced along with the decline of renal function. Low Klotho may partially induce fibroblast growth factor 23 (FGF23) resistance, resulting in an initial compensatory increase in FGF23 serum levels to maintain phosphate homeostasis. Elevated FGF23 decreases vitamin D levels and is followed by elevation of parathyroid hormone (PTH). Hyperphosphatemia is a relatively late event in advanced CKD; normal range is shown in gray. The scale is not meant to be truly proportionate; e.g., the elevation of FGF23 is massive in CKD compared with the elevation of PTH. The X-axis represents decline in renal function from stage 1 to 5 of CKD based on estimated glomerular filtration rate (eGFR). Reproduced with permission from Hu et al. [2]
Elevated PTH levels represent an appropriate body response in CKD
In children with CKD, plasma PTH levels start to rise as early as CKD stage 2 in order to keep serum phosphate levels within the normal range and to counterbalance FGF23-induced calcitriol deficiency and hypocalcemia [3, 17]. This seems to be an important compensatory mechanism since hypocalcemia is associated with poor bone mineralization [18, 19]. Even more importantly, phosphate is a vascular toxin [20]. There is a wealth of evidence coming from in vitro and clinical studies, showing that increased phosphate is associated with ectopic (vascular) calcification and mortality. In vitro studies showed that when exposed to high phosphate conditions, vessels develop apoptosis, vascular smooth-muscle cells convert to bone-like cells, and thus vessels develop extensive calcification [21]. In children on dialysis, elevated serum phosphate levels are associated with increased vessel wall thickness, arterial stiffness, and vascular calcification [8, 9, 22,23,24,25]. Elevated phosphate is associated with increased mortality in dialysis patients and with cardiovascular changes even in pre-dialysis CKD [26, 27]. This data suggests that maintaining serum phosphate levels within the normal range is important to reduce cardiovascular risk and mortality. Therefore, moderately elevated PTH levels may be required to keep a balanced mineral metabolism despite progressive CKD. This mechanism may start as early as in CKD stage 2. Thus, elevated PTH in CKD patients may be primarily interpreted as an appropriate body response in order to survive, i.e., avoid phosphate toxicity, calcitriol deficiency, and symptomatic hypocalcemia.
PTH and bone metabolism
Maintenance of calcium homeostasis and bone remodeling is an important function of PTH. Both PTH pulses and sustained elevations in PTH stimulate calcium release from the bone. PTH elicits its bone anabolic and catabolic effects by stimulating both bone formation and resorption [28]. Adequate bone remodeling is a prerequisite for skeletal development and for attaining peak bone mass. PTH acts via PTH type 1 receptor (PTH1R) expressed in osteoblasts and osteocytes, and increases osteoanabolic Wnt signaling, e.g., via repression of the osteocytic sclerostin. However, severe SHPT may result in high bone turnover and overt renal osteodystrophy including demineralization of bone.
Interpretation of plasma PTH levels in CKD
High phosphate intake, low calcium intake, and/or vitamin D deficiency may cause SHPT even in patients with CKD stage 2–3. In addition, inadequate dialysis efficacy may result in low phosphate removal and thus promote SHPT as well. Therefore, we recommend considering these things first if a patient presents with elevated PTH levels. In addition, serum concentration of PTH generally overestimates biological activity, at least in patients with advanced CKD, due to: i) post-translational modification (oxidation) of PTH, since oxidized PTH is inactive, ii) PTH resistance in target tissue due to accumulation of inhibiting C-terminal fragments, which were shown to have a prolonged half-life in advanced CKD, and iii) end-organ hyporesponsiveness to PTH [28,29,30,31,32]. There is an increasing evidence that CKD impacts on PTH signaling by competitive inhibition between (1-84) PTH and its fragments, PTH1R downregulation, PTH1R dysfunction, e.g., due to FGF23-stimulated soluble Klotho which prevents binding of intact PTH to PTHR, and by inhibitory or competing downregulation signals, including sclerostin, osteoprotegerin, and inflammation [28]. This experimental data is supported by clinical studies in patients with end-stage CKD (ESKD), demonstrating that peripheral arterial disease, i.e., vascular stiffness, is associated with a more pronounced osteoblast resistance to PTH. In patients presenting with peripheral arterial disease, weaker correlation coefficients (slopes) between serum PTH and osteoblast surface were noted when compared with patients lacking vascular stiffness [33]. Therefore, PTH hyporesponsiveness in advanced CKD may explain why low bone turnover disease may be present in patients with PTH levels far above the upper normal limit, and the association between low bone turnover disease and vascular disease. Consequently, “normal” PTH levels cannot be called normal in the light of PTH resistance in advanced CKD.
PTH and growth
Although severe skeletal deformities can contribute to growth retardation, the relationship between longitudinal growth and serum PTH is unclear. Of course, growth is usually completely arrested when SHPT results in severe destruction of the metaphyseal bone architecture [12]. However, in a prospective randomized trial comparing daily or intermittent calcitriol for treatment of SHPT in pre-dialysis patients, a positive association between mean PTH levels and annual change in height SD score (SDS) was observed [34]. In a retrospective study in prepubertal children on long-term dialysis, no association between PTH levels and change in height SDS per year was noted [35]. The IPPN offers the most up-to-date information pertaining to the association between PTH and growth in a large cohort of children on peritoneal dialysis. The annual prospective change in standardized height of this patient cohort tended to correlate inversely with time-integrated mean PTH levels: patients with mean PTH levels > 500 pg/ml (i.e., > 9 times UNL) showed a significant loss in height SDS compared with children with lower PTH levels (−0.28 versus −0.05 SDS per year; p < 0.05) [6]. Thus, dialyzed children with normal or up to 9 times UNL elevated PTH levels retain the potential for normal growth, whereas patients with high PTH levels (> 500 pg/ml) are at an increased risk of growth failure.
PTH and bone histology
Although PTH is widely used for monitoring CKD-MBD, it is not a true marker of bone turnover. This is due to the fact that PTH is neither involved in the process of, nor is a direct product of, bone resorption or formation. Additionally, PTH levels have proved unreliable in independently predicting bone turnover, partly due to skeletal resistance to PTH and accumulation of long C-terminal fragments, as well as PTH assay variability as outlined above. Low bone turnover is generally associated with low or low-normal PTH levels in children as well as in adults with CKD [7, 18, 19, 36]. However, low bone turnover is rarely seen in children on dialysis nowadays (approx. 4%) [18]. In addition, low bone turnover may coincide with elevated levels of PTH and high bone turnover with low PTH levels [37]. There are several pediatric bone biopsy studies designed for correctly identifying bone turnover category by using PTH or a combination of biochemical parameters which showed highly variable PTH thresholds, as recently summarized by Lalayiannis et al. [38]. This is reflected by current guidelines for children which differ markedly with respect to the recommended PTH target levels ranging from 2–3 times UNL in the European guideline, to 2–9 times UNL in the KDIGO guideline. Taken together, cohort studies in children showed that only at extremes is PTH able to predict the bone turnover status with acceptable sensitivity and specifity.
PTH and ectopic calcification
In general, elevated PTH levels are thought to be associated with cardiovascular calcification in patients with ESKD [8,9,10, 23]. However, in one retrospective study evaluating the presence of coronary artery calcification in young adults with childhood-onset ESKD, high PTH levels (> 4 times UNL) were associated with an increased calcification score in combination with increased inflammation (elevated C-reactive protein) only [9]. This concept is further supported by recent ex vivo studies using vessels from children with CKD stage 5, with and without dialysis, demonstrating that calcifying conditions such as high phosphate and calcium promote vascular “inflammaging,” i.e., premature aging and inflammation [39]. In a cohort of 85 children who had received dialysis for at least 6 months, only a weak association between intact PTH serum levels and the degree of coronary artery calcification could be observed (r = 0.39; p = 0.03) [21]. Indeed, half of the patients presenting with PTH levels above 5 times UNL showed no coronary artery calcification at all. Important to note, in the same cohort, carotid intima-media thickness was associated with both PTH levels and vitamin D dosage. Thus, factors other than elevated PTH, such as inflammation and vitamin D medication, may be also important for the development of ectopic calcification in children with ESKD [40].
PTH and patient mortality
In adult dialysis patients, normal or slightly elevated (1–3 times UNL)—as well as very elevated PTH levels (> 5 times UNL)—were associated with increased mortality when compared with patients presenting with PTH levels between 3 and 5 times UNL [10]. Recently, the association of a CKD-MBD phenotype and risk of death was prospectively investigated in a cohort of 26,221 adult dialysis patients [41]. High PTH levels (> 5 times UNL) as well as low PTH levels (< 3 times UNL) were associated with increased risk of death and the composite endpoint of death or cardiovascular hospitalization. It is important to note that this association was much more pronounced in patients also showing high serum calcium and/or phosphate levels. The highest risk was noted in patients with high calcium and PTH (> 5 times UNL). Data from the IPPN registry indicates that PTH levels above 800 pg/ml (> 13 times ILN) are associated with increased mortality (hazard ratio 2.4, p < 0.05) in children on peritoneal dialysis (personal communication, Franz Schaefer). In addition, youth (< 6 years), defined syndrome, hypoalbuminemia (< 25 g/l), serum bicarbonate < 20 mM, and fluid overload (> 4%), were also independently associated with increased mortality in this cohort.
Taken together, studies in dialysis patients point to a U-shaped association between PTH levels and patient outcome (mortality, ectopic calcification). Modest increases in PTH (3–5 times UNL) are associated with a better outcome compared with normal or excessive PTH. Additional alterations of mineral metabolism, e.g., hyperphosphatemia and hypercalcemia also contribute to increased mortality in dialysis patients. Thus, “normal” PTH may be harmful in these patients.
Cardiovascular outcome of PTH decreasing measures (active vitamin D, calcimimetics)
There is no doubt that treatment with active vitamin D and/or calcimimetics improves bone health in patients with high bone turnover [42]. However, the currently available data on cardiovascular outcome is discouraging. Two trials, PRIMO and OPERA, demonstrated a significantly increased risk of hypercalcemia in adult patients with CKD stages 3–5 and PTH levels of 50–300 pg/ml (1–5 times UNL) treated with paricalcitol, compared with a placebo in the absence of beneficial effects on surrogate cardiac endpoints [43, 44]. The EVOLVE trial could not prove the beneficial effects of cinacalcet on patients with CKD stage 5D and SHPT (> 5 times UNL) with respect to the primary endpoint cardiovascular outcome, but demonstrated an increased risk of hypocalcemia [45].
Potential adverse clinical consequences of reducing PTH values to the normal range by use of active vitamin D or calcimimetics
Both treatment for SHPT with active vitamin D and calcimimetics may result in over-suppression of bone remodeling, i.e., low bone turnover disease in patients with advanced CKD, as outlined above. In addition, active vitamin D further stimulates FGF23 in a vicious circle which may promote the development of left ventricular hypertrophy in CKD patients [46]. Furthermore, active vitamin D is known to increase phosphate and calcium (re)absorption in the kidney and from the gut, which may promote ectopic vascular calcification [47]. The use of calcimimetics may cause clinically relevant hypocalcemia resulting in impaired bone mineralization and may cause arrhythmia [48]. Thus, both medications have, at least theoretically, long-term consequence for increased cardiovascular morbidity, especially when aiming for normal PTH levels.
Conclusions
Moderate increases in PTH most likely represent an appropriate adaptive response to declining kidney function in patients with CKD stages 3–5 and perhaps also in CKD stage 2, due to phosphaturic and calcitriol stimulating effects, and increasing bone resistance in advanced CKD. There is no hard evidence for strictly keeping PTH levels within the normal range in CKD patients with respect to bone health (mineralization, turnover, growth), cardiovascular outcome and patient survival. In addition, the potentially adverse effects of PTH-lowering measures, such as active vitamin D and calcimimetics, must be taken into account. In other words, it may even be dangerous to aim for normal PTH levels in patients with advanced CKD. Unfortunately, there is no precise CKD stage-dependent PTH level at which the positive effects of PTH (phosphaturia and stimulation of renal 1α-hydroxylase for prevention/amelioration of hyperphosphatemia and hypocalcemia) are offset by its negative effects (high bone turnover and associated cardiovascular damage). However, based on the available data, we suggest that normal or modest elevated PTH (up to 2 times UNL) may be acceptable in children with early CKD (stages 2–3), provided that measures for treatment of CKD-MBD, including adequate phosphate and calcium intake and vitamin D supplementation in vitamin D-deficient patients, are undertaken. We also suggest that PTH levels of 1.7–5 UNL in patients with advanced CKD (CKD stages 4–5D) may be optimal, and that higher levels should be avoided. Finally, it must be taken into account that the standard care of CKD-MBD in children relies on a combination of different measures in which the observation of PTH levels is only a small part, and it may be wiser to use trends in PTH levels rather than absolute target values to determine treatment decisions in patients with CKD, as recommended by the 2017 KDIGO guidelines [42].
Research recommendations
-
In a large cohort of pediatric patients with CKD stages 3–5D, do assessments of bone histomorphometry and cardiovascular status and correlate these results with various PTH target ranges.
-
Establish a readily available assay quantifying PTH1R signaling tone or sensitivity to PTH and use this test to asses PTH target-organ sensitivity in pediatric patients with advanced CKD. This may help to identify individual PTH target ranges in CKD patients.
-
Assess the sensitivity and specifity of specific biomarkers (or a panel of biomarkers) for bone and cardiovascular health by use of the gold standard bone biopsy and non-invasive measures of cardiovascular status (e.g., carotid intima-media thickness, central pulse wave velocity, cardiac ultrasound for assessment of left ventricular mass, and skin microvascular blood flow).
References
Moe S, Drueke T, Cunningham J, Goodman W, Martin K, Olgaard K, Ott S, Sprague S, Lameire N, Eknoyan G, Kidney Disease: Improving Global Outcomes (KDIGO) (2006) Definition, evaluation, and classification of renal osteodystrophy: a position statement from kidney disease: improving global outcomes (KDIGO). Kidney Int 69:1945–1953
Hu MC, Shiizaki K, Kuro-o M, Moe OW (2013) Fibroblast growth factor 23 and klotho: physiology and pathophysiology of an endocrine network of mineral metabolism. Annu Rev Physiol 75:503–533
Portale AA, Wolf M, Juppner H, Messinger S, Kumar J, Wesseling-Perry K, Schwartz GJ, Furth SL, Warady BA, Salusky IB (2014) Disordered FGF23 and mineral metabolism in children with CKD. Clin J Am Soc Nephrol 9:344–353
Hruska KA, Seifert M, Sugatani T (2015) Pathophysiology of the chronic kidney disease-mineral bone disorder. Curr Opin Nephrol Hypertens 24:303–309
Bakkaloglu SA, Borzych D, Soo Ha I, Serdaroglu E, Buscher R, Salas P, Patel H, Drozdz D, Vondrak K, Watanabe A, Villagra J, Yavascan O, Valenzuela M, Gipson D, Ng KH, Warady BA, Schaefer F, International Pediatric Peritoneal Dialysis Network (2011) Cardiac geometry in children receiving chronic peritoneal dialysis: findings from the international pediatric peritoneal dialysis network (IPPN) registry. Clin J Am Soc Nephrol 6:1926–1933
Borzych D, Rees L, Ha IS, Chua A, Valles PG, Lipka M, Zambrano P, Ahlenstiel T, Bakkaloglu SA, Spizzirri AP, Lopez L, Ozaltin F, Printza N, Hari P, Klaus G, Bak M, Vogel A, Ariceta G, Yap HK, Warady BA, Schaefer F, International Pediatric PD Network (IPPN) (2010) The bone and mineral disorder of children undergoing chronic peritoneal dialysis. Kidney Int 78:1295–1304
Salusky IB, Ramirez JA, Oppenheim W, Gales B, Segre GV, Goodman WG (1994) Biochemical markers of renal osteodystrophy in pediatric patients undergoing CAPD/CCPD. Kidney Int 45:253–258
Goodman WG, Goldin J, Kuizon BD, Yoon C, Gales B, Sider D, Wang Y, Chung J, Emerick A, Greaser L, Elashoff RM, Salusky IB (2000) Coronary-artery calcification in young adults with end-stage renal disease who are undergoing dialysis. N Engl J Med 342:1478–1483
Oh J, Wunsch R, Turzer M, Bahner M, Raggi P, Querfeld U, Mehls O, Schaefer F (2002) Advanced coronary and carotid arteriopathy in young adults with childhood-onset chronic renal failure. Circulation 106:100–105
Kalantar-Zadeh K, Kuwae N, Regidor DL, Kovesdy CP, Kilpatrick RD, Shinaberger CS, McAllister CJ, Budoff MJ, Salusky IB, Kopple JD (2006) Survival predictability of time-varying indicators of bone disease in maintenance hemodialysis patients. Kidney Int 70:771–780
Denburg MR, Kumar J, Jemielita T, Brooks ER, Skversky A, Portale AA, Salusky IB, Warady BA, Furth SL, Leonard MB (2016) Fracture burden and risk factors in childhood CKD: results from the CKiD cohort study. J Am Soc Nephrol 27:543–550
KDOQI Work Group (2009) KDOQI clinical practice guideline for nutrition in children with CKD: 2008 update. executive summary. Am J Kidney Dis 53:S11–S104
Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group (2009) KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD). Kidney Int Suppl 113:S1–S130
Klaus G, Watson A, Edefonti A, Fischbach M, Ronnholm K, Schaefer F, Simkova E, Stefanidis CJ, Strazdins V, Vande Walle J, Schroder C, Zurowska A, Ekim M, European Pediatric Dialysis Working Group (EPDWG) (2006) Prevention and treatment of renal osteodystrophy in children on chronic renal failure: European guidelines. Pediatr Nephrol 21:151–159
Haffner D, Schaefer F (2013) Searching the optimal PTH target range in children undergoing peritoneal dialysis: new insights from international cohort studies. Pediatr Nephrol 28:537–545
Rees L (2008) What parathyroid hormone levels should we aim for in children with stage 5 chronic kidney disease; what is the evidence? Pediatr Nephrol 23:179–184
Norman ME, Mazur AT, Borden S, Gruskin A, Anast C, Baron R, Rasmussen H (1980) Early diagnosis of juvenile renal osteodystrophy. J Pediatr 97:226–232
Bakkaloglu SA, Wesseling-Perry K, Pereira RC, Gales B, Wang HJ, Elashoff RM, Salusky IB (2010) Value of the new bone classification system in pediatric renal osteodystrophy. Clin J Am Soc Nephrol 5:1860–1866
Pereira RC, Bischoff DS, Yamaguchi D, Salusky IB, Wesseling-Perry K (2016) Micro-CT in the assessment of pediatric renal osteodystrophy by bone histomorphometry. Clin J Am Soc Nephrol 11:481–487
Shroff R (2013) Phosphate is a vascular toxin. Pediatr Nephrol 28:583–593
Shroff RC, Donald AE, Hiorns MP, Watson A, Feather S, Milford D, Ellins EA, Storry C, Ridout D, Deanfield J, Rees L (2007) Mineral metabolism and vascular damage in children on dialysis. J Am Soc Nephrol 18:2996–3003
Civilibal M, Caliskan S, Adaletli I, Oflaz H, Sever L, Candan C, Canpolat N, Kasapcopur O, Kuruoglu S, Arisoy N (2006) Coronary artery calcifications in children with end-stage renal disease. Pediatr Nephrol 21:1426–1433
Briese S, Wiesner S, Will JC, Lembcke A, Opgen-Rhein B, Nissel R, Wernecke KD, Andreae J, Haffner D, Querfeld U (2006) Arterial and cardiac disease in young adults with childhood-onset end-stage renal disease-impact of calcium and vitamin D therapy. Nephrol Dial Transplant 21:1906–1914
Groothoff JW, Gruppen MP, Offringa M, de Groot E, Stok W, Bos WJ, Davin JC, Lilien MR, Van de Kar NC, Wolff ED, Heymans HS (2002) Increased arterial stiffness in young adults with end-stage renal disease since childhood. J Am Soc Nephrol 13:2953–2961
Mitsnefes MM, Kimball TR, Kartal J, Witt SA, Glascock BJ, Khoury PR, Daniels SR (2005) Cardiac and vascular adaptation in pediatric patients with chronic kidney disease: role of calcium-phosphorus metabolism. J Am Soc Nephrol 16:2796–2803
Block GA, Hulbert-Shearon TE, Levin NW, Port FK (1998) Association of serum phosphorus and calcium × phosphate product with mortality risk in chronic hemodialysis patients: a national study. Am J Kidney Dis 31:607–617
Voormolen N, Noordzij M, Grootendorst DC, Beetz I, Sijpkens YW, van Manen JG, Boeschoten EW, Huisman RM, Krediet RT, Dekker FW, PREPARE study group (2007) High plasma phosphate as a risk factor for decline in renal function and mortality in pre-dialysis patients. Nephrol Dial Transplant 22:2909–2916
Evenepoel P, Bover J, Urena Torres P (2016) Parathyroid hormone metabolism and signaling in health and chronic kidney disease. Kidney Int 90:1184–1190
Wesseling-Perry K, Harkins GC, Wang HJ, Elashoff R, Gales B, Horwitz MJ, Stewart AF, Juppner H, Salusky IB (2010) The calcemic response to continuous parathyroid hormone (PTH)(1-34) infusion in end-stage kidney disease varies according to bone turnover: a potential role for PTH(7-84). J Clin Endocrinol Metab 95:2772–2780
Hocher B, Armbruster FP, Stoeva S, Reichetzeder C, Gron HJ, Lieker I, Khadzhynov D, Slowinski T, Roth HJ (2012) Measuring parathyroid hormone (PTH) in patients with oxidative stress—do we need a fourth generation parathyroid hormone assay? PLoS One 7:e40242
Hruska KA, Korkor A, Martin K, Slatopolsky E (1981) Peripheral metabolism of intact parathyroid hormone. Role of liver and kidney and the effect of chronic renal failure. J Clin Invest 67:885–892
Vervloet MG, Brandenburg VM, CKD-MBD working group of ERA-EDTA (2017) Circulating markers of bone turnover. J Nephrol 30:663–670
London GM, Marchais SJ, Guerin AP, de Vernejoul MC (2015) Ankle-brachial index and bone turnover in patients on dialysis. J Am Soc Nephrol 26:476–483
Schmitt CP, Ardissino G, Testa S, Claris-Appiani A, Mehls O (2003) Growth in children with chronic renal failure on intermittent versus daily calcitriol. Pediatr Nephrol 18:440–444
Cansick J, Waller S, Ridout D, Rees L (2007) Growth and PTH in prepubertal children on long-term dialysis. Pediatr Nephrol 22:1349–1354
Sprague SM, Bellorin-Font E, Jorgetti V, Carvalho AB, Malluche HH, Ferreira A, D'Haese PC, Drueke TB, Du H, Manley T, Rojas E, Moe SM (2016) Diagnostic accuracy of bone turnover markers and bone histology in patients with CKD treated by dialysis. Am J Kidney Dis 67:559–566
Diamond T, Elder GJ (2017) Is there a practical role for bone biopsy in chronic kidney disease? Nephrology (Carlton) 22(Suppl 2):22–26
Lalayiannis AD, Crabtree NJ, Fewtrell M, Biassoni L, Milford DV, Ferro CJ, Shroff R (2019) Assessing bone mineralisation in children with chronic kidney disease: what clinical and research tools are available? Pediatr Nephrol. https://doi.org/10.1007/s00467-019-04271-1
Sanchis P, Ho CY, Liu Y, Beltran LE, Ahmad S, Jacob AP, Furmanik M, Laycock J, Long DA, Shroff R, Shanahan CM (2019) Arterial "inflammaging" drives vascular calcification in children on dialysis. Kidney Int 95:958–972
Querfeld U, Schaefer F (2018) Cardiovascular risk factors in children on dialysis: an update. Pediatr Nephrol. https://doi.org/10.1007/s00467-018-4125-x
Block GA, Kilpatrick RD, Lowe KA, Wang W, Danese MD (2013) CKD-mineral and bone disorder and risk of death and cardiovascular hospitalization in patients on hemodialysis. Clin J Am Soc Nephrol 8:2132–2140
Ketteler M, Block GA, Evenepoel P, Fukagawa M, Herzog CA, McCann L, Moe SM, Shroff R, Tonelli MA, Toussaint ND, Vervloet MG, Leonard MB (2017) Executive summary of the 2017 KDIGO chronic kidney disease-mineral and bone disorder (CKD-MBD) guideline update: what's changed and why it matters. Kidney Int 92:26–36
Wang AY, Fang F, Chan J, Wen YY, Qing S, Chan IH, Lo G, Lai KN, Lo WK, Lam CW, Yu CM (2014) Effect of paricalcitol on left ventricular mass and function in CKD—the OPERA trial. J Am Soc Nephrol 25:175–186
Thadhani R, Appelbaum E, Pritchett Y, Chang Y, Wenger J, Tamez H, Bhan I, Agarwal R, Zoccali C, Wanner C, Lloyd-Jones D, Cannata J, Thompson BT, Andress D, Zhang W, Packham D, Singh B, Zehnder D, Shah A, Pachika A, Manning WJ, Solomon SD (2012) Vitamin D therapy and cardiac structure and function in patients with chronic kidney disease: The PRIMO randomized controlled trial. JAMA 307:674–684
Trial Investigators EVOLVE, Chertow GM, Block GA, Correa-Rotter R, Drueke TB, Floege J, Goodman WG, Herzog CA, Kubo Y, London GM, Mahaffey KW, Mix TC, Moe SM, Trotman ML, Wheeler DC, Parfrey PS (2012) Effect of cinacalcet on cardiovascular disease in patients undergoing dialysis. N Engl J Med 367:2482–2494
Haffner D, Leifheit-Nestler M (2017) Extrarenal effects of FGF23. Pediatr Nephrol 32:753–765
Haffner D, Hocher B, Muller D, Simon K, Konig K, Richter CM, Eggert B, Schwarz J, Godes M, Nissel R, Querfeld U (2005) Systemic cardiovascular disease in uremic rats induced by 1,25(OH)2D3. J Hypertens 23:1067–1075
Warady BA, Iles JN, Ariceta G, Dehmel B, Hidalgo G, Jiang X, Laskin B, Shahinfar S, Vande Walle J, Schaefer F (2019) A randomized, double-blind, placebo-controlled study to assess the efficacy and safety of cinacalcet in pediatric patients with chronic kidney disease and secondary hyperparathyroidism receiving dialysis. Pediatr Nephrol 34:475–486
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
DH and MLN received a research grant from Amgen. DH received consultant fees from Amgen.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Haffner, D., Leifheit-Nestler, M. Treatment of hyperphosphatemia: the dangers of aiming for normal PTH levels. Pediatr Nephrol 35, 485–491 (2020). https://doi.org/10.1007/s00467-019-04399-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-019-04399-0