Abstract
Background
In 1998, a survey of the European Society for Paediatric Nephrology (ESPN) revealed substantial disparities in pediatric renal care among European countries. Therefore, ESPN aimed at harmonizing renal care in all European countries in the following 20 years. In 2017, we conducted a survey to evaluate the current status of renal health policies for children in Europe.
Methods
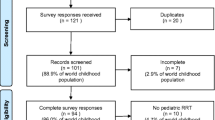
A 33-question web-based survey was designed and sent to presidents or representatives of national societies of pediatric nephrology in 44 European countries.
Results
Data was reported from 42 (95.5%) countries. The number of pediatric nephrologists per million child population increased from 1998 to 2017 in 70% of countries. Pediatric dialysis facilities for acute kidney injury and end-stage kidney disease were available in 95% of countries. The availability of pediatric kidney transplantation increased from 55 to 93% of countries. Considerable variation was found in the current availability of allied health professionals, including psychosocial and nutritional support, high-tech diagnostic methods, and treatment with expensive drugs for children with kidney diseases between different European countries.
Conclusions
The 20-year follow-up analysis of pediatric renal care services in European countries revealed that pediatric nephrology has become a well-established subspecialty in pediatrics and nephrology in 2017. The ESPN will continue its efforts to further improve pediatric renal care for European children by harmonizing remaining disparities of renal care services.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Following acceptance of pediatrics as a distinct specialty in the early 20th century, different pediatric subspecialties started to develop [1]. In 1967, 36 pediatric nephrologists from 22 countries gathered in Glasgow to establish the European Society for Paediatric Nephrology (ESPN) heralding the beginning of pediatric sub-specialization in nephrology in Europe [2]. While the primary goal of the ESPN was to harmonize pediatric renal care across Europe, a survey performed in 1998 revealed substantial disparities among European countries [3]. Therefore, in the following years, the ESPN aimed at further improving pediatric nephrology training and care in all European countries.
Fifty years after establishing the ESPN and 20 years after the previous survey, we sent a follow-up questionnaire to evaluate the current status of pediatric renal health policies in Europe and to identify the most relevant needs in order to further improve renal care for children and adolescents.
One of the main focus points of the European health policy framework, Health 2020, is to significantly reduce health inequalities and ensure universal, equitable, and high-quality health services across Europe [4]. Although all European member states have made commitments towards this goal, considerable international disparities in treatment and mortality rates have been described. Disparities in pediatric renal care have been explained by the differences in country’s macroeconomics, the distribution of underlying causes of kidney diseases, the quality of renal care, the access to treatment, and the attitudes to acceptance or withdrawal from treatment [5].
Up-to-date and detailed epidemiologic data regarding the pediatric renal care in Europe is vital for policymakers, physicians, and healthcare providers. In addition, national or single-center studies are often unable to provide sufficient statistical power to accurately assess the quality of renal care.
On behalf of the ESPN, in 2017, we sent a follow-up questionnaire on pediatric renal care in order to evaluate the current status of renal health policies for children in different European countries. The study had two aims: (1) to compare European pediatric renal care in 1998 and 2017; (2) to identify the most relevant pediatric nephrology needs in various European countries in order to further improve pediatric kidney care in Europe by harmonizing remaining disparities in renal care for children and adolescents.
Patients and methods
Survey content and participants
On behalf of the ESPN, we designed an online survey with 33 questions regarding demographics, delivery of care, treatment policy, renal replacement therapy (RRT), and organization of kidney health service in 2017 in Europe. We included to the survey part of the same questions from the study of demography of pediatric renal care in 1998 in Europe to perform comparative analysis [3]. Ethics committee approval was deemed unnecessary for this study, as the survey did not contact patients or require any specific patient data.
The survey was sent to the presidents or representatives of national societies of pediatric nephrology in 44 countries where pediatric nephrologists can be members of the ESPN.
Definitions
“Pediatric nephrologistˮ was defined as a licensed pediatrician with a minimum 3 years of training in pediatrics including experience in neonatology and intensive care plus a higher 3-year specialty training in pediatric nephrology in out- and in-patient settings, working full time in general pediatric nephrology, dialysis, and pediatric kidney transplantation (Tx) [3]. “Pediatrician with a special interest/activity in pediatric nephrology” was defined as a general pediatrician devoting part of the time to the care of children with common renal diseases in settings without facilities for dialysis or kidney Tx [3].
Data collection and statistical analysis
Comparative analysis of the results from the ESPN survey in 2017 was conducted in comparison with the data from the ESPN survey performed in 1998 [3].
Statistical data about children population aged 14 years in each European country were available from the US Bureau of the Census based on statistics from population censuses and vital statistics registration systems [6]. Countries were classified according to gross national income (GNI) level estimated per capita/year from the World Bank database (2017) and divided into two groups according to their income level per capita/year:
- 1.
Lower and upper-middle-income countries (LUMICs) (n = 14) with $996–12,055 GNI/capita/year, included one lower (Ukraine) and 13 upper-middle-income countries (Albania, Armenia, Azerbaijan, Belarus, Bosnia and Herzegovina, Bulgaria, Georgia, Kazakhstan, Macedonia, Romania, Russia, Serbia, Turkey);
- 2.
High-income countries (HICs) (n = 28) with ≥ $12,056 GNI/capita/year (Austria, Belgium, Croatia, Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Ireland, Israel, Italy, Lithuania, Luxembourg, Malta, Netherlands, Norway, Poland, Portugal, Slovak Republic, Slovenia, Spain, Sweden, Switzerland, UK) [4].
The estimated numbers of additionally required pediatric nephrologists and dialysis nurses were determined by the presidents or representatives of national societies of pediatric nephrology according to the categorized question of the survey with different options, including “none”, “< 10”, “11–20”, and “> 20”. Validation of the collected data was achieved by personal contacts with reporting presidents or representatives and by discussions among the ESPN council members representing various European regions.
Standard descriptive statistics were used: continuous variables were presented as medians (Me) with interquartile range (IQR), and categorical variables were expressed as frequencies. Comparisons were performed using Fisher’s exact test for categorical variables and Mann–Whitney test for continuous variables. To compare paired continuous data, a nonparametric Wilcoxon signed-rank test was used. All tests were two-sided and two-tailed. P values < 0.05 were considered statistically significant. Statistical analyses were performed using GraphPad Prism (GraphPad Software Inc., San Diego).
Results
Participating countries
Data was reported from 42 out of the 44 countries (95.5% response rate). We did not receive responses from Latvia and Moldova.
Physicians and nurses
The total number of pediatric nephrologists in the 42 European countries increased from 842 in 1998 to 1719 in 2017. There were no pediatric nephrologists in Estonia in 2017.
The median number of pediatric nephrologists per million child population (pmcp) aged < 14 years in Europe doubled from 1998 compared with 2017 (5.2 (IQR 0–14.8) vs. 10.5 (IQR 0–35.7) (p < 0.0001)) (Table 1). In 2017, the number of pediatric nephrologists across Europe was not significantly different between LUMICs and HICs (14.4 (5.7; 18.8) vs. 10.1 (7.1; 14.4) (p = 0.58)).
The total number of pediatric nephrologists pmcp increased from 1998 to 2017 in 70% of European countries and remained stable in 21% of countries. A pediatric renal care service was newly established in 9% of countries, including Azerbaijan, Belarus, Kazakhstan, and Serbia.
The total number of pediatricians with a special interest/activity in pediatric nephrology in Europe increased from 1087 in the year 1998 to 1274 in the year 2017. The median number of pediatricians with a special interest/activity in pediatric nephrology with lack of training in dialysis and Tx pmcp remained stable (6.0 (3.2; 13.3) vs. 7.7 (2.0; 16.0) (p = 0.29)) (Table 1).
In 2017, the estimated number of lacking pediatric workforce comprised less than 10 pediatric nephrologists in 66% of countries and more than 10 in 14% of countries (Table 2). No extra nephrologists were required in 20% of European countries. According to the estimation of reporting national experts, less than 10 pediatric dialysis nurses were required in 51% of countries, more than 10 nurses in 35%, and no extra need was reported in 14% of European countries.
Pediatric nephrology centers
The total number of pediatric dialysis centers for acute kidney injury (AKI) increased from 224 centers in 1998 to 299 centers in 2017. There were no pediatric centers offering treatment for end-stage kidney disease (ESKD) in 2017 in Azerbaijan and Luxembourg. Patients from Luxembourg are routinely referred to Belgium for dialysis and kidney Tx.
The availability of pediatric dialysis facilities for AKI increased from 83% of countries in 1998 to 95% of countries in 2017 (p = 0.16) and for ESKD from 81% to 95% of European countries, respectively (p = 0.049) (Fig. 1).
The total number of pediatric dialysis centers for ESKD in European countries increased from 179 in 1998 to 266 in 2017.
The total number of pediatric kidney Tx centers increased from 99 in 1998 to 135 in 2017. The availability of pediatric kidney Tx increased from 55% in 1998 to 93% of countries in 2017 (p < 0.0001) (Fig. 1). Three of the 42 European countries (Bulgaria, Luxembourg, Malta) had no pediatric kidney Tx programs in 2017. Patients from Malta are routinely referred to the UK for kidney Tx.
In 2017, children on RRT were followed by pediatric nephrologists in 93% of European countries, except of Bosnia and Herzegovina and Ukraine. The proportion of European countries reporting their data to the ESPN/ERA-EDTA Registry for RRT rose from 70% in 1998 to 86% in 2017.
Organization of pediatric renal care services
Multi-disciplinary care
In 2017, multi-disciplinary care was provided for young patients in 211 specialized pediatric nephrology centers in Europe, including 63 in LUMICs and 148 in HICs.
The psychosocial support was available in specialized pediatric nephrology European centers in 83% of countries; however, it was present only in 58% of LUMICs compared with 100% of HICs (p = 0.0001) (Table 3).
Even larger disparity was found in availability of renal nutritional support which was present in 62% of European countries, the majority of which were HICs (89%). Strikingly, only 7% of LUMICs reported the availability of pediatric renal dieticians (p < 0.0001).
In 2017, transition programs from pediatric to adult renal care services existed in 52% of European countries. A difference was found in availability of these programs between LUMICs and HICs (21% vs. 68% (p = 0.008)).
Recognition of subspecialty
In 2017, pediatric nephrology was recognized as a subspecialty in 69% of European countries, including 93% of LUMICs and 57% of HICs (p = 0.032) (Table 3). In 57% of European countries, pediatric nephrology was recognized as a subspecialty by the government, in 27% by the scientific societies, and in 16% by both the government and scientific society.
In 2017, national societies of pediatric nephrology existed in 60% of European countries, including 36% of LUMICs and 71% of HICs (p = 0.045).
Pediatric nephrology sessions at national pediatric congresses were organized in 71% of the countries, including 50% of LUMICs and 82% of HICs (p = 0.067).
Support for scientifically active pediatric nephrologists
Institutional or hospital support for scientifically active pediatric nephrologists to attend international meetings for presenting their research was provided in 49% of European countries, including 14% of LUMICs and 64% of HICs (p = 0.003) (Table 3). Access of hospital library to medical information data bank systems online (such as PubMed) was available for free via internet access in 76% of European countries, including 57% of LUMICs and 86% of HICs (p = 0.059).
Access to diagnostic facilities/screening programs
Screening for arterial hypertension in healthy children by casual blood pressure measurement was done in 38% of European countries, including 29% of LUMICs and 43% of HICs (Table 4). All the 42 European countries offered access to 24-h ambulatory blood pressure monitoring (ABPM) for children.
Screening for renal diseases using urinary dipsticks was performed in preschool children in 19% of European countries, including 29% of LUMICs and 14% of HICs and in school children in 17% of countries, including 14% of LUMICs and 18% of HICs.
In 86% of countries, histopathological kidney examination involving light, immunofluorescence, and electron microscopy was implemented. Kidney biopsies in children were performed by pediatric nephrologists in 52% of countries, adult nephrologists in 17%, radiologists in 11%, urologists in 10%, and surgeons in 10% of countries.
Access to high-tech diagnostic methods
DNA tests for inherited kidney diseases were available in 76% of European countries, including 64% of LUMICs and 82% of HICs. Sanger sequencing for single genes causing hereditary kidney diseases was routinely available in 48% of countries, including only 14% of LUMICs and 65% of HICs (p = 0.003) (Table 5). We found that next-generation sequencing was available only in HICs in comparison with LUMICs (54% vs. 0% (p = 0.001)). Significant difference was found in availability of GFR measuring by isotopic tests between LUMICs and HICs (14% vs. 54% (p = 0.02)).
Dynamic and static nuclear scans were also more frequently available in HICs in comparison with LUMICs (92% vs. 43% (p = 0.001)). Contrast-enhanced kidney ultrasound was available in 31% of countries, including 15% of LUMICs and 39% of HICs (p = 0.27). Metabolomics was the least accessible diagnostic method in 2017 (available only in Switzerland). Therapeutic drug monitoring of commonly used immunosuppressants (such as cyclosporine or tacrolimus) was available in 83% of European countries, including 64% of LUMICs and in 92% of HICs in 2017 (p = 0.039).
Access to therapy with expensive drugs
Table 6 demonstrates data on availability of expensive drugs in 2017. Most of the expensive drugs, including growth hormone, erythropoietin, active vitamin D, rituximab, eculizumab, and IL-2 receptor antagonists, were more frequently available in HICs in comparison with LUMICs (Table 6).
Discussion
ESPN is one of more than 30 European pediatric societies aiming at promoting knowledge for the benefit of children with severe, complex, and rare diseases [7, 8]. Our 2017 data clearly show that during the last 20 years, the pediatric nephrology workforce has substantially grown in Europe. RRT for AKI and ESKD is now available in almost all European countries, and its quality and outcome are regularly monitored by the ESPN/ERA-EDTA Registry [9]. However, there are still several gaps in training and disparities in the level of care provided which should be addressed in the near future.
One of the essential needs is the shortage of well-trained pediatric nephrologists and dialysis nurses reported from more than 80% of European countries. Our numbers are higher than anticipated by a recent survey of the International Pediatric Nephrology Association (IPNA) which reported that 42% of respondents from Europe described a mild to severe shortage of pediatric nephrology workforce [10].
Though training curricula and duration varied from country to country, most European countries, the USA, and Australia/New Zealand recommended 3-year subspecialty training after a 3-year basic training in general pediatrics [8, 11, 12]. In 2017, pediatric nephrology was accredited as a subspecialty in near than two-thirds of European countries. However, national criteria for accreditation were not well standardized according to international recommendations. National societies of pediatric nephrology existed in only 60% of European countries; these societies are important driving force to tailor training requirements according to regional- and country-level needs/expectations without sacrificing well-functioning organizational structures [13]. Sharif et al. analyzed the global nephrology workforce and recommended “effective training programs at the undergraduate and postgraduate level, adoption of novel recruitment strategies, flexible workforce practices, greater ownership of the traditional nephrology landscape and enhanced opportunities for research” [14]. In the future, ESPN will prioritize further harmonization of training curricula and develop European recognition criteria for pediatric nephrologists. The ESPN and IPNA training courses and Master for Junior Classes have proved to be successful in connecting physicians in developing countries with high standard pediatric nephrology training across Europe and around the globe [8, 15].
The quality of care for children with kidney diseases is dependent not only on the number of fully trained health care providers but also on their dedication and organization of care, as well as access to medical technologies and treatments. In this regard, a major improvement was achieved by cross-border renal care and research organized by the ESPN working groups, and last, but not least, by friendly cooperation between groups of nephrologists working in different countries [16]. Nevertheless, we demonstrated that considerable variation still exists in the current availability of high-tech diagnostic methods and treatment with expensive drugs for children with kidney diseases between LUMICs and HICs in Europe. Most of the revealed differences may be explained by disparities in public health expenditure, which seems to limit the availability and quality of pediatric renal care. Our findings can be used by the policymakers and health care providers to explore potential strategies to help reduce these financial and organizational health care disparities. Cross-border care and online consultation system for patients with rare kidney diseases within the frame of the European Reference Kidney Network gives access to diagnostics and care for patients from countries not yet offering the full spectrum of therapeutic modalities to their young patients [17].
Another important observation of our survey was the diversity of organizing multi-disciplinary care in pediatric renal health services in different European countries. The main finding was the lack of allied health professionals in many LUMICs including low availability of psychosocial and nutritional support, and of well-planned transition programs from pediatric to adult renal care services. Therefore, ESPN will focus its educational activities not only on medical but also on reducing fragmented care by increasing integrated care which has to be provided by an alliance of all health professionals when preparing and empowering young patients for adult life.
Based on our reported findings, ESPN will intensify the cooperation between national pediatric nephrology societies in order to further improve pediatric renal care in Europe by harmonizing training/education and stimulating cross-border collaboration between pediatric nephrologists and allied professionals.
References
Zipursky A (2002) A history of pediatric specialties. Pediatr Res 52:617. https://doi.org/10.1203/00006450-200211000-00002
Tse Y, Maxwell H, Watson AR, Coward R, Levtchenko E, Christian M, European society for paediatric nephrology (2018) preserving oral history: 50 years of paediatric nephrology in Europe. Arch Dis Child 103:1010–1012. https://doi.org/10.1136/archdischild-2018-315308
Ehrich JHH, Gendi AA, Drukker A, Janda J, Stefanidis C, Verrier-Jones K, Collier J, Katz M (2005) Demography of paediatric renal care in Europe: organization and delivery. Nephrol Dial Transplant 20:297–305 https://doi.org/10.1093/ndt/gfh299
The World Bank database (2017). https://datahelpdesk.worldbank.org/knowledgebase/articles/906519. Accessed 24 August 2019
Kramer A, Stel VS, Caskey FJ, Stengel B, Elliott RF, Covic A, Geue C, Cusumano A, Macleod AM, Jager KJ (2012) Exploring the association between macroeconomic indicators and dialysis mortality. Clin J Am Soc Nephrol 7:1655–1663. https://doi.org/10.2215/CJN.10461011
US Bureau of the Census (2017). https://www.indexmundi.com. Accessed 24 August 2019
Ehrich J, Kerbl R, Pettoello-Mantovani M, Lenton S (2015) Opening the debate on pediatric subspecialties and specialist centers: opportunities for better care or risks of care fragmentation. J Pediatr 167:71–74. https://doi.org/10.1016/j.jpeds.2015.07.060
ESPN. www.espn-online.org. Accessed 24 August 2019
ESPN / ERA-EDTA Registry for children on renal replacement therapy. https://www.espn-reg.org. Accessed 24 August 2019
Glenn D, Ocegueda S, Nazareth M, Zhong Y, Weinstein A, Primack W, Cochat P, Ferris M (2016) The global pediatric nephrology workforce: a survey of the International Pediatric Nephrology Association. BMC Nephrol 17:1–11. https://doi.org/10.1186/s12882-016-0299-2
Primack WA, Glenn DA, Meyers KEC (2016) Pediatric nephrology training worldwide 2016: Quantum Educatus? Kidney Int Rep 18:144–147. https://doi.org/10.1016/j.ekir.2016.07.002
Paediatric Section of the Union of European Medical Specialists (2018). https://espn-online.org/training_doc.pdf. Accessed 24 August 2019
Phadke K, Bagga A (2005) Training in pediatric nephrology for developing countries. Pediatr Nephrol 20:1205–1207. https://doi.org/10.1007/s00467-005-1972-z
Sharif MU, Elsayed ME, Stack AG (2016) The global nephrology workforce: emerging threats and potential solutions! Clin Kidney J 9:11–22. https://doi.org/10.1093/ckj/sfv111
International Pediatric Nephrology Association IPNA Online/Fellowship Program. https://www.ipna-online.org/education/fellowship-program. Accessed 24 August 2019
IPNA-ESPN Master for Junior Classes. https://espn-online.org/2_ipna_espn.php. Accessed 24 August 2019
European Reference Kidney Network. https://www.erknet.org. Accessed 24 August 2019
Acknowledgments
The authors would like to thank the representatives from European national pediatric nephrology societies who answered the survey and provided the data reported in this paper. We thank all ESPN council members in 2017 for their input and support: Ariceta G. (Spain), Bacchetta J. (France), Duzova A. (Turkey), Haffner D. (Germany).
European Society for Paediatric Nephrology collaborators (in alphabetical order) Anton-Gamero M. (Spain), Arikoski P. (Finland), Aufricht C. (Austria), Awan A. (Ireland), Bakkaloglu SA (Turkey), Baylarov R. (Azerbaijan), Bjerre A. (Norway), Brandström P. (Sweden), Chafai R. (Luxembourg), Lotan D. (Israel), Davitaia T. (Georgia), Dlin V. (Russia), Golubovic E. (Serbia), Hadjipanayis A. (Cyprus), Hoyer P. (Germany), Hughes DA (UK), Ivanov D. (Ukraine), Jankauskiene A. (Lithuania), Kamperis K. (Denmark), Kersnik Levart T. (Slovenia), Laube G. (Switzerland), Lungu A. (Romania), Milosevic D. (Croatia), Murer L. (Italy), Nigmatullina N. (Kazakhstan), Podraska L. (Slovak Republic), Pokrajac D. (Bosnia and Herzegovina), Reusz G.S. (Hungary), Roussey G. (France), Roussinov D. (Bulgaria), Said Conti V. (Malta), Sarkissian A. (Armenia), Schreuder M. (The Netherlands), Seeman T. (Czech Republic), Shtiza D. (Albania), Simão C. (Portugal), Stefanidis C.J. (Greece), Tasic V. (Macedonia), Toots Ü. (Estonia), Tur N. (Belarus), Walle JV (Belgium), Zurowska A. (Poland).
Author information
Authors and Affiliations
Consortia
Contributions
All authors participated to the designing of the questionnaire. LP, JE, and EL checked the data, analyzed the results, and drafted the manuscript with the help of all other authors, who revised it critically. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Prikhodina, L., Ehrich, J., Shroff, R. et al. The European Society for Paediatric Nephrology study of pediatric renal care in Europe: comparative analysis 1998–2017. Pediatr Nephrol 35, 103–111 (2020). https://doi.org/10.1007/s00467-019-04378-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-019-04378-5