Abstract
Background
Primary hyperoxaluria type 3 (PH3) is characterized by mutations in the 4-hydroxy-2-oxoglutarate aldolase (HOGA1) gene. PH3 patients are thought to present with a less severe phenotype than PH1 and PH2 patients. However, the clinical characteristics of PH3 patients have yet to be defined in sufficient detail. The aims of this study were to report HOGA1 mutations of PH3 in Chinese children, and to analyze the genotype and clinical characteristics of these PH3 patients.
Methods
Genetic analysis (targeted gene panel-based and/or whole-exome sequencing) of HOGA1 was performed in 52 patients with a high suspicion of PH3, and DNA was obtained from the patient and both the parents. The clinical, biochemical, and genetic data of these 12 patients identified with HOGA1 mutations were subsequently retrospectively reviewed.
Results
These 12 patients were identified with HOGA1 mutation. The median onset of clinical symptoms was 18.25 (range 5–38) months. In total, 14 different mutations were identified including 9 novel mutations in these 12 patients with PH3. All of these 12 patients initially presented with urolithiasis, and 3 patients among them comorbid urinary tract infection (UTI) as another initial symptom. Ten patients experienced hyperoxaluria (average oxalate 0.77 mmol/1.73 m2/24h). In contrast, urine calcium excretion was normal in 8 patients and 2 patients with hypercalciuria (urine calcium > 4 mg/kg/24 h). At the time of diagnosis, estimated GFR was 155.6 ml/min per 1.73 m2, and at last follow-up time (17.3 months later from diagnosis on average), estimated GFR was 157.5 ml/min per 1.73 m2. To date, none of the patients has impaired renal function based on and progressed to ESRD.
Conclusions
We found that PH3 was significantly diagnosed in our urolithiasis patients during childhood. Nine novel HOGA1 mutations were identified in association with PH3, which provide a first-line investigation in Chinese PH3 patients. The eGFR was normal in all children with PH3. This finding is in contrast to the early impairment of renal function in PH1 and PH2.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nephrolithiasis is a major public health predicament with diverse and convoluted etiology. In China, the incidence of urinary stones in children has been increasing in the last decade. Many factors can induce nephrolithiasis, and these encompass extremes of urinary pH, dehydration, hypercalciuria, particular medications, hyperoxaluria, and hereditary disorders [1]. Hyperoxaluria is either acquired or inherited. Primary hyperoxalurias (PHs) are rare inborn errors of metabolism that are inherited in an autosomal recessive manner. They are the result of monogenic disorders of glyoxylate metabolism and lead to increased endogenous oxalate production by the liver and the formation of calcium oxalate kidney stones [1, 2].
To date, three distinct genetic forms of PH have been defined: PH1–3. PH1 (MIM# 259900), the most common and the most severe form, is due to the mutation in the alanine–glyoxylate aminotransferase gene (AGXT), and patients typically progress to end-stage renal disease (ESRD) [3]. PH2 (MIM# 260000) is due to a mutation in the glyoxylate reductase–hydroxypyruvate reductase (GRHPR); 20% of patients develop ESRD [3, 4]. PH3 (MIM# 613616) is due to the mutation in the recently identified 4-hydroxy-2-oxoglutarate aldolase (HOGA1) gene; it does not develop ESRD generally [5]. Compared with PH1 and PH2, PH3 might be the least severe form with a milder phenotype with good preservation of kidney function in most patients [6]. This often leads to delay in diagnosis. Up to the present time, most of the literatures focus on PH1 and PH2. However, few PH3 patients among Asians have been reported, but the clinical features and renal outcomes of patients with PH3 are not sufficiently characterized, especially in Chinese children. In this article, we report a series of 12 PH3 children with clinical manifestations ranging from asymptomatic nephrolithiasis to acute kidney injury (AKI) in whom genetic analysis was done. The aims of this study were to report HOGA1 mutations with PH3 in Chinese children, and to describe the genotype and the clinical characteristics of these PH3 patients.
Patients and methods
Patients
From routine inquiries and referrals to the clinic center, we first selected for HOGA1 screening patients who met the clinical criteria for primary hyperoxaluria (urine oxalate > 0.5 mmol/1.73 m2/24 h in the absence of gastrointestinal disease or other identifiable secondary causes), in whom ultrasonography of the urinary system revealed nephrolithiasis in kidneys and/or urethral stones, nephrocalcinosis included; 52 patients with urolithiasis were enrolled in this study. Urinary oxalate was analyzed only once before diagnosis. Informed consent was given for a genetic analysis to be performed on the patients, their family members, and healthy controls to confirm the diagnosis. Each patient was informed about the aims of the study, and the consent to genetic testing was obtained. After an initial survey of HOGA1 gene mutations responsible for PH3, gene sequencing was performed on all patients with a high clinical and biological suspicion of PH at our clinic center. From this group of patients, we identified 12 patients (23%), aging from 5 to 38 months, from different regions of East China with HOGA1 mutations: six male patients and six female patients. The median age of onset of clinical symptoms was 18.25 (range 5–38) months.
The diagnosis of PH was based on clinical findings (urolithiasis, nephrocalcinosis, and end-stage renal failure), elevated plasma oxalate, and urinalysis (raised oxalate) in combination with spectrophotometric analysis of the calculi. Demographic characteristics, serum creatinine, blood electrolytes, urinary oxalate, and calcium were assessed. We tried many methods to detect plasma oxalate but all failed, so the data on this cannot be provided in this paper. The estimated glomerular filtration rate (eGFR) in children was estimated by Schwartz equation [7]. Clinical, biochemical, and genetic data were reviewed retrospectively by the referring physicians and centralized by one investigator (LA). Results were compared to age-related reference ranges.
Study design
This is an observational study conducted in Department of Pediatric Urology, during the period January 2016 to December 2017. This clinical study was evaluated and approved by the Institutional Ethics Committee on Human Studies at Xinhua Hospital.
Molecular approach
Blood and DNA samples from patients and both the parents with suspected PH were received for analysis by Shanghai Institute for Pediatric Research. Genomic DNA was extracted from peripheral blood leukocytes using guanidinium chloride standard procedures. All the samples were subjected to exome sequencing using the SureSelect Human All Exon V5 probe (Agilent, Santa Clara, CA, USA). Part of the patient samples were subjected to targeted gene panel-based and others were subjected to whole-exome sequencing. Sanger sequencing was used to examine the cosegregation of the candidate variants. Amplified fragments were sequenced by Applied Biosystems 96-capillary 3730XL system. Mutations have been identified in various populations (refer to the Human Gene Mutation Database, HGMD professional 2018.3, http://www.hgmd.org/).
Results
First, we sequenced the entire HOGA1 coding region in 52 unrelated hyperoxaluric patients meeting the criteria of marked hyperoxaluria. No patient had nephrocalcinosis. Fourteen different mutations in HOGA1 were detected including 9 novel changes in 12 patients with PH3; no specific mutations of PH were found among these parents. Five mutations, c.769 T > G, c.834G > A, c.715G > A, c.208C > T, and c.834_834 + 1GG > TT, have been reported previously. Nine novel mutations, c.290G > A, c.554C > T, c.110G > A, c.812G > A, c.841C > T, c.811C > T, c.70delG, c.406G > C, and c.418C > T, were not reported previously. A summary of genotype and the clinical and biochemical characteristics of these PH3 patients are presented in Table 1.
One mutation was a successive 2-nucleotide substitution at the last position of exon 6 and the first position of intron 6, respectively (c.834_834 + 1GG > TT), including the change of classical donor splicing site (GT → TT) combined with the alteration of its upstream close neighbor nucleotide; both sites may play an important role as a splicing modulator. Seven patients were heterozygous for this mutation. The second variant found in the patient was a guanine to adenine substitution of the last nucleotide of exon 6 (c.834G > A), which results in a synonymous mutation (p.Ala278Ala). We found that the father carried the heterozygous c.834G > A variant, while the mother carried the heterozygous c.834_834 + 1GG > TT mutation in 3 patients. The in-frame c.70delG (p.V24Sfs*19) mutation was detected in a heterozygous state in one patient. Seven missense mutations were found also: the previously documented c.769 T > G (p.CyS257Gly) and c.715G > A (p.Val239Ile) mutations; and five novel c.110G > A (p.Gly37Asp), c.290G > A (p.Arg97His), c.554C > T (p.Thr185Met), c.812G > A (p.Arg271His), and c.841C > T (p.R281W) mutation. Moreover, we found two patients with a missense mutation (c.290G > A p.Arg97His and c.715G > A p.V239I, respectively) inherited from the father. PolyPhen-2 (available at http://genetics.bwh.harvard.edu/pph2) analysis predicted that this variant is “benign.” Another patient was heterozygote for one novel nonsense mutation within exon 1: c.208C > T (p.Arg70X), which led to premature termination.
Most PH3 patients did not have a positive family history for urolithiasis. All PH3 patients presented with urolithiasis, but the clinical symptoms of the PH3 are different; 3 patients first suffered from urinary tract infection (UTI) leading to a further diagnosis of bilateral kidney stones, and one of them had anuria caused by acute kidney injury (AKI), 4 patients had hematuria, 1 patient presented with abdominal pain, and 4 patients had no symptoms. Eleven patients presented with bilateral stones; only one patient had a unilateral stone. An average level of urinary oxalate excretion was detected in 10 patients with hyperoxaluria according to age-related local values (average urine oxalate 0.77 mmol/1.73 m2/24 h, normal < 0.5 mmol/1.73 m2/24 h), and was not detected in time in 2 other patients with bilateral multiple urinary calculi with a high suspicion of PH, due to machine failure. During follow-up, we reexamined the urinary oxalate of the 2 patients with values of 0.57 mmol/1.73 m2/24 h and 0.65 mmol/1.73 m2/24 h. Urine calcium excretion was determined in 10 patients with levels observed above the reference range in 2 patients with hypercalciuria (urine calcium > 4 mg/kg/24 h). Most of the cases in Chinese children were found to have normal urine calcium excretion.
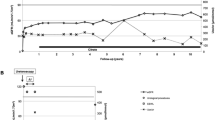
All patients received supportive therapy, based on high fluid intake and oral citrate, as recommended by international guidelines [8]. Most patients can remove urinary stone by less traumatic surgical methods (such as extracorporeal shock wave lithotripsy (ESWL), ureteroscopy, retrograde intrarenal surgery (RIRS)), thus avoiding percutaneous nephrolithotomy and open surgery, thereby reducing the damage to the kidney of the stone removal procedure itself. The outcomes of 12 patients with PH3 are presented in Table 2. Two of the children with hypercalciuria were also given oral hydrochlorothiazide, and another child received antibiotic prophylaxis for UTI. The urinary stones in 5 patients were completely removed; none recurred, but in 2 patients were recurred during follow-up. Five other patients had residual stone; one of them was an insignificant residual stone. Stone analysis showed predominantly calcium oxalate monohydrate. At diagnosis, estimated GFR was 155.6 ml/min per 1.73 m2, and at last follow-up (median 17.3 months from diagnosis), estimated GFR was 157.5 ml/min per 1.73 m2. To date, all patients have normal renal function; none of the patients has displayed impaired renal function and progressed to ESRD.
Discussion
The estimated prevalence of PH is around 1–3 per million of the population. Phenotypic heterogeneity and non-availability of mutational analysis universally have led to its underdiagnosis. Short of mutational analysis, other investigations such as plasma and urine oxalate levels are not confirmatory. The molecular mechanisms of PH1 and PH2 were identified in 1988 and 1999, respectively [4, 9]. PH1 is the most severe form, accounting for 80% of all the cases. PH2 shows a less severe phenotype with the absence of infantile oxalosis and ESRD occurring in about 20% of patients. However, the association of PH3 and mutations in HOGA1 gene was not established until 2010 [6]. Both PH2 and PH3 may have similar prevalence of about 10% of total genetically characterized PH cases [10]. Four other publications have focused on this disease, leading to the description of a total of 60 cases [5, 6, 11,12,13]; PH3 was first described in Ashkenazi Jewish pedigrees [6], then in Caucasians. Up to now, most of the described PH3 mutations came from the population of European Americans and rarely in the Chinese population [14, 15].
To date, more than 200 mutations have been described in PH patients, including 26 variants in PH3 with the 2 most common alleles (c.700 + 5G > T and p.E315del) accounting for more than 70% of the total [5, 11, 16]. Fourteen different HOGA1 gene mutations were detected in 12 patients with PH3. However, the most common alleles had not been detected in our study. We detect the mutation of c.834_834 + 1GG > TT is most common in the Chinese population, which accounts for 50% of the total. This result was different from the previously reported common mutations. The reason for this difference in results may be that most PH3 mutations previously reported came from the population of European Americans. So, a relationship between HOGA1 and ethnic distribution may be suspected. Different ethnic groups may have different genetic mutations. With the mutations being population specific, sequencing of the entire gene rather than targeted analysis will be required.
We investigate a series of children with clinical manifestations ranging from nephrolithiasis to infantile oxalosis in whom genetic analysis was done. The results of the genetic analysis confirmed PH1 in six children, PH2 in one children, and PH3 in 12 children [17]. According to the study by Hopp et al. [16], the overall carrier frequency of PH is approximately 1:70, and the inferred prevalence is approximately 1:58,000. Surprisingly, the frequency of PH3 in our clinic center is higher than PH1 and PH2; however, the difference between the expected and observed prevalences for PH3 may be due to the underdiagnosis of this disease which has overall milder phenotypes, is usually asymptomatic, and is much less likely than PH1 to result in ESRD [16]. Additionally, Monico et al. [12] found that some HOGA1 carriers present with mild hyperoxaluria or idiopathic urinary stone disease; they suppose this may be related to haploinsufficiency. Therefore, gene analysis of HOGA1 is informative to the diagnoses of PH3 cases who have idiopathic calcium oxalate urolithiasis or PH phenocopies [18, 19].
To further characterize the PH3 phenotype, we pooled our clinical experience, assembling patients from 12 unrelated families. Genetic analysis is invaluable in deciding the appropriate management, prognostication, prenatal diagnostic testing, and sibling screening. Bilateral multiple renal stones were found in a majority of PH3 children with normal renal function followed by serum creatinine and echogenic kidneys on ultrasound examination. Hence, children with multiple renal stones, especially bilateral, should be thoroughly investigated for PH. The urine oxalate was higher at presentation in PH3 patients compared with locally established reference values, and PH3 patients displayed persistent hyperoxaluria at examination, as previously reported [5, 20]. The urinary oxalate levels of the 10 Chinese children were higher in our clinic center and were elevated: the mean value being 0.77 mmol/1.73 m2/24h. These patients presented hyperoxaluria according to international reference values. Hypercalciuria was found in half of published cases [6, 11, 21], but only 2 patients from our series presented with this abnormality. The excretion of 4-hydroxyglutamate—a potential biomarker for PH3—was not investigated in our patients, which is known to be relatively unstable [20, 22] and is metabolized either enzymatically or non-enzymatically to glyoxylate and/or oxalate. Stone analysis showed predominantly calcium oxalate monohydrate. All patients with PH3 described in previous studies displayed a normal eGFR during follow-up consistent to these previous data reporting a favorable outcome in PH3 patients. No patient experienced impaired eGFR in our study. However, the PH3 patient with ESRD was recently reported [14, 23, 24], suggesting that PH3 may not be as clinically benign as previously thought. These studies have reported that the GFR was significantly impaired in some patients with PH3 diagnosed during childhood. This finding is in contrast to the early impairment of renal function in PH1 and PH2 patients and appears to refute preliminary reassuring data on renal function in PH3. However, the underlying reason of the decline in kidney function remains unclear. They analyzed that the severity of PH3 in their series was also demonstrated by a high rate of urological procedures, with some patients even requiring open surgery to remove stones. Speculatively speaking, it may not be hyperoxaluria or urolithiasis per se but the repeated stone removal procedures [14, 16]. Therefore, we suggest that each stone removal procedure should be carefully evaluated and discussed to avoid potential additional damage. All of these urological procedures may have hampered renal function. However, it is impossible to determine whether the renal impairment seen in patients is secondary to PH3 itself, to kidney damage secondary to urological procedures, or to both possibilities. These data reinforce the need for long-term renal function follow-up of patients with PH3, and show that PH3 should no longer be regarded as a benign condition. We showed the stone removal procedures in the 12 patients in Table 2. Obviously, there were few stone removal procedures, so that this should be commented a little better, as with regard to kidney function over time. In order to better understand the prognosis of PH3, we plan to follow these PH3 patients prospectively through a registry or some other mechanism.
The information derived from our detailed analysis (i.e., genetic, clinical, and biochemical analyses) of this series of 12 patients with PH3 starting during childhood includes (1) the first report of a series of HOGA1 gene mutation in 12 Chinese children patients with PH3. Fourteen different mutations were identified including nine novel mutations. The mutation of c.834_834 + 1GG > TT is most common in this Chinese population, which accounts for 50% of the total. (2) Most patients presented with bilateral stones. Patients presented with hyperoxaluria according to age-related local values, and urine calcium excretion was normal for most. There was no significant impairment of eGFR in all patients; none of the patients developed ESRD. (4) The diagnostic procedure we would recommend in patients to examine for primary hyperoxaluria is that every child with urolithiasis should have a complete metabolic assessment, and if the urinary oxalate level is higher or multiple urolithiasis is on both sides, then we recommend genetic analysis for these patients.
Abbreviations
- PH:
-
Primary hyperoxaluria
- AGXT:
-
Alanine–glyoxylate aminotransferase
- ESRD:
-
End-stage renal disease
- GRHPR:
-
Glyoxylate reductase–hydroxypyruvate reductase
- HOGA1:
-
4-Hydroxy-2-oxoglutarate aldolase
- eGFR:
-
Estimated glomerular filtration rate
- UTI:
-
Urinary tract infection
- CaOx:
-
Calcium oxalate
- CaPhos:
-
Calcium phosphate
References
Harambat J, Fargue S, Bacchetta J, Acquaviva C, Cochat P (2011) Primary hyperoxaluria. Int J Nephrol 2011:864580
Cochat P, Rumsby G (2013) Primary hyperoxaluria. N Engl J Med 369:649–658
Hoppe B (2012) An update on primary hyperoxaluria. Nat Rev Nephrol 8:467–475
Cramer SD, Ferree PM, Lin K, Milliner DS, Holmes RP (1999) The gene encoding hydroxypyruvate reductase (GRHPR) is mutated in patients with primary hyperoxaluria type II. Hum Mol Genet 8:2063–2069
Beck BB, Baasner A, Buescher A, Habbig S, Reintjes N, Kemper MJ, Sikora P, Mache C, Pohl M, Stahl M, Toenshoff B, Pape L, Fehrenbach H, Jacob DE, Grohe B, WolfMT NG, Yigit G, Salido EC, Hoppe B (2013) Novel findings in patients with primary hyperoxaluria type III and implications for advanced molecular testing strategies. Eur J Hum Genet 21:162–172
Belostotsky R, Seboun E, Idelson GH, Milliner DS, Becker-Cohen R, Rinat C, Monico CG, Feinstein S, Ben-Shalom E, Magen D, Weissman I, Charon C, Frishberg Y (2010) Mutations in DHDPSL are responsible for primary hyperoxaluria type III. Am J Hum Genet 87:392–399
Schwartz GJ, Muñoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637
Cochat P, Hulton S-A, Acquaviva C, Danpure CJ, Daudon M, Demarchi M, Fargue S, Groothoff J, Harambat J, Hoppe B, Jamieson NV, Kemper MJ, Mandrile G, Marangella M, Picca S, Rumsby G, Salido E, Straub M, van Woerden CS, OxalEurope: Primary hyperoxaluria type 1: indications for screening and guidance for diagnosis and treatment. Nephrol Dial Transplant 2012; 27:1729–1736
Danpure CJ, Jennings PR (1986) Peroxisomal alanine: glyoxylate aminotransferase deficiency in primary hyperoxaluria type I. FEBS Lett 201:20–24
M'dimegh S, Aquaviva-Bourdain C, Omezzine A, Souche G, M'barek I, Abidi K, Gargah T, Abroug S, Bouslama A (2017) HOGA1 gene mutations of primary hyperoxaluria type 3 in Tunisian patients. J Clin Lab Anal 31(3):1–5. https://doi.org/10.1002/jcla.22053
Williams EL, Bockenhauer D, van’t Hoff WG, Johri N, Laing C, Sinha MD, Unwin R, Viljoen A, Rumsby G (2012) The enzyme 4-hydroxy-2-oxoglutarate aldolase is deficient in primary hyperoxaluria type 3. Nephrol Dial Transplant 27:3191–3195
Monico CG, Rossetti S, Belostotsky R, Cogal AG, Herges RM, Seide BM, Olson JB, Bergstrahl EJ, Williams HJ, Haley WE, Frishberg Y, Milliner DS (2011) Primary hyperoxaluria type III gene HOGA1 (formerly DHDPSL) as a possible risk factor for idiopathic calcium oxalate urolithiasis. Clin J Am Soc Nephrol 6:2289–2295
Jacob DE, Grohe B, Gessner M, Beck BB, Hoppe B (2013) Kidney stones in primary hyperoxaluria: new lessons learnt. PLoS One 8:e70617
Allard L, Cochat P, Leclerc AL, Cachat F, Fichtner C, De Souza VC, Garcia CD, Camoin-Schweitzer MC, Macher MA, Acquaviva-Bourdain C, Bacchetta J (2015) Renal function can be impaired in children with primary hyperoxaluria type 3. Pediatr Nephrol 30(10):1807–1813. https://doi.org/10.1007/s00467-015-3090-x
Xinsheng Wang, Xiangzhong Zhao, Xiaoling Wang, Jian Yao, Feifei Zhang, Yanhua Lang, Sylvie Tuffery-Giraud, Irene Bottillo, Leping Shao: Two novel HOGA1 splicing mutations identified in a Chinese patient with primary hyperoxaluria type 3. Am J Nephrol 2015;42:78–84.DOI: https://doi.org/10.1159/000439232
Hopp K, Cogal AG, Bergstralh EJ, Seide BM, Olson JB, Meek AM, Lieske JC, Milliner DS, Harris PC (2015) Rare kidney stone consortium: phenotype-genotype correlations and estimated carrier frequencies of primary hyperoxaluria. J Am Soc Nephrol 10:2559–2570
Jiang D, Geng H (2017) Primary hyperoxaluria. N Engl J Med 376:e33. https://doi.org/10.1056/NEJMicm1609986
Greed L, Willis F, Johnstone L, Teo S, Belostotsky R, Frishberg Y, Pitt J (2018) Metabolite diagnosis of primary hyperoxaluria type 3. Pediatr Nephrol 33(8):1443–1446. https://doi.org/10.1007/s00467-018-3967-6
Richard E, Blouin JM, Harambat J, Llanas B, Bouchet S, Acquaviva C, de la Faille R (2017) Late diagnosis of primary hyperoxaluria type III. Ann Clin Biochem 54(3):406–411. https://doi.org/10.1177/0004563216677101
Pitt JJ, Willis F, Tzanakos N, Belostotsky R, Frishberg Y (2015) 4-Hydroxyglutamate is a biomarker for primary hyperoxaluria type 3. JIMD Rep 15:1–6
Riedel TJ, Knight J, Murray MS, Milliner DS, Holmes RP, Lowther WT (2012) 4-Hydroxy-2-oxoglutarate aldolase inactivity in primary hyperoxaluria type 3 and glyoxylate reductase inhibition. Biochim Biophys Acta 1822:1544–1552
Aronson LD, Rosso R, GAdams E. A constitutive aldolase for 4-hydroxy-2-ketoglutarate in soil bacteria. Biochim Biophys Acta 1967;132:200–203
Ventzke A, Feldkötter M, Wei A, Becker J, Beck BB, Hoppe B (2017) Systematic assessment of urinary hydroxy-oxo-glutarate for diagnosis and follow-up of primary hyperoxaluria type III. Pediatr Nephrol 32(12):2263–2271. https://doi.org/10.1007/s00467-017-3731-3
Zhao F, Bergstralh EJ, Mehta RA, Vaughan LE, Olson JB, Seide BM, Meek AM, Cogal AG, Lieske JC, Milliner DS (2016) Predictors of incident ESRD among patients with primary hyperoxaluria presenting prior to kidney failure. Clin J Am Soc Nephrol 11(1):119–126
Acknowledgments
We acknowledge the efforts of the entire clinical and non-clinical staff of the Department of Pediatric Urology, Xinhua Hospital, in identifying potential patients, and procuring and transporting the blood samples. We thank Dr. Yu Yongguo and his study group, Shanghai Institute for Pediatric Research, whose research has benefitted our patients and their families to a great extent.
Financial support and sponsorship
This study was supported by grants from the National Natural Scientific Foundation of China (81770702).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no competing interests exist.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fang, X., He, L., Xu, G. et al. Nine novel HOGA1 gene mutations identified in primary hyperoxaluria type 3 and distinct clinical and biochemical characteristics in Chinese children. Pediatr Nephrol 34, 1785–1790 (2019). https://doi.org/10.1007/s00467-019-04279-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-019-04279-7