Abstract
Background
Chronic systemic hypertension has a well-known association with increased cardiovascular morbidity and mortality. One of the most important target organs affected in systemic hypertension is the heart. In addition, chronic kidney disease (CKD) further increases the mortality from cardiovascular disease. The aim of this study was to evaluate the differences in the cardiovascular changes in pediatric patients with primary hypertension (pHTN) vs. those with secondary hypertension from chronic kidney disease (CKD-HTN).
Methods
This was a retrospective chart review of patients with CKD-HTN and pHTN. The medical records were reviewed for anthropometric data, biochemical assessment of renal function, and for cardiovascular changes on echocardiogram.
Results
Twenty-three patients with pHTN and 29 patients with CKD-HTN were included in the study. There were no differences in age, gender, weight, height, body mass index, and blood pressure between the 2 groups. There was a high prevalence of left ventricular diastolic dysfunction among both the groups (CKD-HTN 25 vs. pHTN 26%). Reduced mitral valve inflow Doppler E/A ratio, a marker of left ventricular diastolic dysfunction in echocardiogram, was more pronounced in CKD-HTN patents, in comparison to those with pHTN (p = 0.042). Also, diastolic function worsened with declining glomerular filtration rate in patients with CKD-HTN. Similarly, patients with CKD-HTN had a larger aortic root dimension when compared to patients with pHTN (p = 0.049).
Conclusions
The prevalence of left ventricular diastolic dysfunction is similar in patients with pHTN and CKD-HTN. Patients with CKD-HTN appear to have more severe diastolic dysfunction and larger aortic root dimensions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic hypertension (HTN) is one of the major risk factors for cardiovascular morbidity and mortality. In adults, elevated blood pressure has been shown to be associated with stroke and coronary artery disease [1]. The severity and duration of HTN have an impact on target organ damage. Children diagnosed with HTN at an early age are at higher risk for developing adverse cardiovascular events in adulthood [2, 3]. Secondary hypertension is relatively more common in children when compared to adults. Chronic kidney disease (CKD) is one of the common causes of secondary hypertension in pediatric patients [4].
In children and adults with CKD, cardiovascular disease (CVD) is the leading cause of mortality. This is especially true in those with advanced CKD due to the higher prevalence of non-traditional risk factors, such as dysregulation of mineral metabolism, in addition to other traditional risk factors [5, 6]. However, there is evidence that CVD even occurs in early CKD which can progress with time [7, 8]. Thus, children with CKD and HTN (CKD-HTN) could have accelerated risk for CVD, when compared with subjects with pHTN. Understanding the early echocardiographic changes in these patients, when compared to those with pHTN may help in early recognition and prevention of CVD.
Increased afterload on the left ventricle due to HTN causes left ventricular hypertrophy (LVH) and remodeling [9]. LVH is the most common manifestation of cardiac involvement in patients with hypertension [10, 11]. It has been demonstrated in many studies that LVH is an independent predictor of adverse cardiovascular outcomes [12, 13]. In addition to LVH, left ventricular remodeling is also prevalent in patients with HTN [14]. Systolic function of the heart is rarely affected in pediatric patients with HTN. However, diastolic dysfunction, an indicator of the compliance of the heart, has been previously reported in children with HTN [14, 15]. Many studies have replicated an increase in the left ventricular mass in children with primary hypertension (pHTN) and secondary HTN due to chronic kidney disease (CKD-HTN) [10, 14,15,16,17,18]. Dilatation of the aortic root has been well described in adults with HTN. Approximately 10% of adults with HTN have dilatation of the aortic root [18, 19].
There is a relative paucity of literature comparing cardiovascular changes in patients with pHTN and CKD-HTN. Given this background, we tried to compare and analyze the markers of cardiovascular changes among pediatric patients with pHTN and CKD-HTN. We hypothesize that the patients with CKD-HTN might have an additional risk for cardiac abnormalities when compared to those with pHTN. We also evaluated the association of cardiovascular changes in these patients with variables related to CKD, including kidney function, proteinuria, and abnormal mineral metabolism.
Methods
This was a retrospective chart review of patients with pHTN and CKD-HTN followed at the Holtz Children’s/Jackson Memorial Hospital during the period of January 2009 through December of 2016. This review was approved by the Institutional Review Board of Human Subjects Research at the University of Miami and Holtz Children’s Hospital. Pediatric patients with HTN who underwent both renal and cardiac evaluation, including a transthoracic echocardiogram, were included in this study.
The patients with diagnosis of systemic HTN were obtained using the diagnosis code (ICD 9 codes 401-404 and ICD 10 codes I10-I15). Among these patients, those who had complete evaluation (cardiology visit, nephrology visit, echocardiogram, and laboratory evaluation), within a 6-month window were included in this study. HTN is defined as a blood pressure of ≥ 95th percentile for age, gender, and height percentile or history of hypertension on antihypertensive medications. Patients with history of congenital heart disease, genetic disorders, organ transplant recipients, and secondary hypertension not related with CKD were excluded. We also excluded the patients with advanced CKD (stages 4–5, dialysis, or kidney transplantation) since these patients might have fluid overload and marked anemia, confounding factors, contributing to cardiovascular changes. The patients included in this study were classified into 2 groups: pHTN and HTN due to CKD (CKD-HTN). pHTN is diagnosed in patients with no identifiable etiology for HTN. CKD is defined as abnormal renal structures and or function for > 3 months [20].
The medical records of the patients included in this study were then reviewed and data collected. The following variables were extracted from the medical records: weight, height, body mass index (BMI), systolic, and diastolic blood pressures during the nephrology evaluation. In general practice, the blood pressure was measured routinely by standard oscillometric equipment. If the blood pressure was elevated, there would be two more repeat measurements to confirm HTN, and the average value was recorded in the electronic medical record. The Z-scores for the blood pressure values were calculated using an online tool from the Baylor College of Medicine (Houston, TX) (www.bcm.edu/bodycomplab/Flashapps/BPVAgeChartpage.html). This online tool uses the data provided by the Fourth Report from the National High Blood Pressure Education Program (NHBPEP) working group on Children and Adolescents in 2004. Selected laboratory tests, including blood urea nitrogen (BUN), serum creatinine, calcium, phosphorus, alkaline phosphatase, intact parathyroid hormone (iPTH), 25-hydroxy vitamin D, uric acid, and low-density lipoprotein cholesterol concentrations, as well as hemoglobin A1C (HbA1C), were collected. The glomerular filtration rate (GFR) was calculated using bedside Schwartz formula from the available laboratory data.
The transthoracic echocardiograms were performed using one of the two available ultrasound systems in our laboratory (Vivid 9, GE Medical Systems, Milwaukee, WI; iE33, Philips USA, Bothell, WA). The data of interest in echocardiography were left ventricular systolic and diastolic function parameters, left ventricular mass index (LVMI), left ventricular geometry, and aortic root measurements. The Z-scores for weight, height, and BMI were calculated using CDC growth charts (www.cdc.gov/growthcharts/zscore.htm).
Left ventricular ejection fraction (EF) and shortening fraction (SF) were used as measurements of left ventricular systolic function. EF was calculated using biplane Simpson method in the apical views of the heart as recommended by the American Society of Echocardiography. SF was calculated in the parasternal short axis views using M-mode data. The other M-mode measurements calculated include interventricular septal thickness in diastole (IVSD), left ventricular end diastolic dimension (LVEDD), posterior wall thickness at end diastole (PWD), and left ventricular end systolic dimension (LVESD). The relative wall thickness (RWT) and indexed left ventricular mass (LVMI) were also calculated using the above M-mode measurements. RWT was calculated using the formula (2 × PWD)/LVEDD [21, 22]. The left ventricular mass was calculated using the Devereux formula [22]. The LVMI was then calculated by dividing the calculated left ventricular mass in grams by the patient’s height (in meters) raised to the power of 2.7 (LVMI = left ventricular mass (gm)/height (m)2.7).
The diastolic function of the left ventricle was calculated from left ventricular inflow pulsed Doppler and from tissue Doppler imaging (TDI) of the left ventricular lateral wall and the interventricular septum, as recommended by the American Society of Echocardiography. Normal left ventricular inflow Doppler has two components: an E wave which represents early filling of the ventricle and a smaller A wave which represents late diastolic filling during atrial contraction. The normal TDI is characterized by early (e’) and late (a’) diastolic myocardial excursion velocities.
The diameter of the aortic root was calculated in the parasternal long axis views during systole. It represents the maximal diameter of the aorta at the level of the sinuses of Valsalva [23]. The Z-scores for the aortic root were calculated using an online Boston Children’s Hospital Z-score calculator.
Definitions of echocardiographic data
An E/A ratio less than 1 [24] and/or an E/e’ ratio Z-score greater than + 2 [15] is defined as diastolic dysfunction of the left ventricle. The Z-scores for E/e’ were calculated using the reference values established by Eidem et al. in 2004 [25]. LVH is defined as LVMI of greater than 95th percentile for age and gender [26]. Using LVMI and RWT, left ventricular geometry is generally classified into four patterns: (1) normal geometry: normal LVMI and RWT; (2) concentric remodeling: normal LVMI and increased RWT; (3) eccentric hypertrophy: increased LVMI and normal RWT; and (4) concentric hypertrophy: increased LVMI and RWT [14].
Statistical analysis
Descriptive characteristics were expressed as mean (SD), median [interquartile range], and percentage of occurrence. A non-parametric Mann-Whitney (two-tail) test and one-way t test (parametric data) were employed to evaluate differences in variables between hypertensive children with or without CKD. Fisher’s exact test was used for non-parametric data, and chi-squared test was used to evaluate contingency tables between the two groups. Correlation analysis was also done to evaluate the relationship between the variables. Statistical analyses were performed using GraphPad Prism (La Jolla, CA) and IBM-SPSS Statistical software (IBM Corporation, Armonk, NY). A significance level (α) of 0.05 was used for each of the tests.
Results
From the cohort of 110 pediatric patients with a diagnosis of systemic HTN who had concurrent care with both pediatric cardiologist and pediatric nephrologist during the study, only 60 patients had laboratory tests performed and a comprehensive echocardiography evaluation done within a 6-month period. Of these 60 patients, we excluded 8 who had clinical course as expected in patients with pHTN, but laboratory tests revealed low GFR. A repeat laboratory evaluation could not be performed in these 8 patients to confirm the renal insufficiency as they were lost to follow up. The final group consisted of 23 patients with pHTN and 29 patients with CKD-HTN (Table 1). Among the 52 study subjects, 52% were Latinos and 46% were African Americans. Among the 29 subjects with CKD-HTN, 15 (53%), 10 (34%), and 4 (13%) had CKD stages 1, 2, and 3, respectively. The etiology of CKD included dysplastic, obstructive, or reflux nephropathy (n = 15; 8, 6, and 1 with stage 1, 2, and 3 CKD, respectively), cystic kidney disease (n = 5; 3 in stages 2, and 1 each with stage 1 and 3 CKD), diabetic nephropathy (n = 3, all with stage 1 CKD), focal segmental glomerulosclerosis (n = 2, both had stage 3 CKD), residual CKD following atypical hemolytic uremic syndrome (n = 2; 1 with stage 1 and the other with stage 2 CKD), and acquired atrophic kidney post perinatal complications (n = 2, both with stage 1 CKD). The median interval between biochemical assessment and echocardiogram was 9 weeks in the pHTN group and 4 weeks in the CKD-HTN group, respectively. There were no significant differences between the two groups in terms of age, gender, BMI, systolic and diastolic blood pressures, or percentage of patients with stage 2 HTN. The estimated GFR calculated was significantly lower for the CKD-HTN group when compared to the pHTN group (p = 0.03). Similarly, the urine protein/creatinine ratio was significantly higher in the CKD-HTN group compared to the pHTN group (p = 0.02). It was also noted that the number of antihypertensive medications used for treatment of HTN was higher in patients with CKD-HTN when compared to those with pHTN (p = 0.007). Serum calcium, phosphorus, 25-hydroxy vitamin D, uric acid, low-density lipoprotein cholesterol, and hemoglobin A1C levels were not significantly different between the groups. Three patients in the CKD-HTN group were diagnosed with secondary hyperparathyroidism, but none were severe enough to be treated with activated vitamin D. The iPTH levels in these patients were 106 pg/ml (patient 1), 109 pg/ml (patient 2), and 158 pg/ml (patient 3). Among these, patient 3 was noted to have diastolic dysfunction of the left ventricle with E/e’ ratio Z-score of + 2.13. The other two did not meet the criteria for diastolic dysfunction. Patients 1 and 3 met the criteria for LVH, with LVMI Z-scores of +2.06 and +3.49, respectively. None of these patients had dilatation of the aortic root. There was limited data on iPTH in the pHTN group, and therefore, a comparative analysis could not be performed.
Comparison of cardiac variables
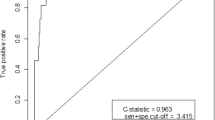
Table 2 shows the comparative data of cardiac variables between the two groups. There was no statistically significant difference in the systolic function of the left ventricle between the groups. There was a higher prevalence of diastolic dysfunction of the left ventricle in both the groups (pHTN 26% vs. CKD-HTN 25%). The absolute value of E/A at the left ventricular inflow, a marker of diastolic dysfunction, was lower in patients in the CKD-HTN group when compared to the pHTN group (p = 0.042). Also, patients with CKD-HTN had a larger aortic root dimension in comparison to patients with pHTN (p = 0.049) (Table 2 and Fig. 1). With no difference in BMI between the two study groups, these above results are unlikely to be influenced by obesity.
Comparison of aortic root diameter and diastolic dysfunction (E/A ratio) in patients with primary hypertension (pHTN) vs. chronic kidney disease hypertension (CKD-HTN). Patients with CKD-HTN had larger aortic root Z-score when compared to those with pHTN. Patients with CKD-HTN had lower E/A ratio, an indicator of diastolic dysfunction, when compared to those with pHTN
There was a higher prevalence of LVH in the CKD-HTN group compared to the pHTN group (35 vs. 26%), but this did not reach statistical significance (p = 0.56). The patterns of LV remodeling in the two groups were as follows (pHTN vs. CKD-HTN): (1) normal geometry 39 vs. 31%, (2) concentric remodeling 35 vs. 34%, (3) eccentric hypertrophy 13 vs. 7%, and (4) concentric hypertrophy 13 vs. 28% (Fig. 2).
Correlation analysis showed a strong association between BMI Z-score and LVMI Z-score in both the groups (CKD-HTN r = 0.68, p < 0.001; pHTN r = 0.44, p = 0.04) (Fig. 3). There was an inverse correlation between the GFR as estimated by the Schwartz method and septal E/e’ ratio (the higher the ratio, the worse the diastolic function) (Fig. 4). There was no significant association of GFR with systolic blood pressure (p = 0.79) and diastolic blood pressure (p = 0.37).
Discussion
HTN is relatively infrequent in the pediatric population. The spectrum of cardiovascular morbidity and mortality secondary to HTN in the pediatric population is different from that in adults. In the adult population, coronary artery disease is the most common condition coexisting with HTN, which increases the morbidity and mortality. Whereas in children with HTN, in particular those with CKD, arrhythmia and cardiomyopathy are the major causes of cardiovascular morbidity and mortality [27]. Alterations in neurohormonal and calcium metabolism play a role in development of HTN in children with CKD. This altered metabolism causes abnormal mineralization of the vascular smooth muscles contributing to increased vessel stiffness [27, 28]. Furthermore, alterations in lipoprotein, fibroblast growth factors, and homocysteine metabolism in addition to inflammation could contribute to early CVD [29, 30].
In this study, patients in the CKD-HTN group required a higher number of antihypertensive medications when compared to those in the pHTN group. While this could reflect more severe HTN in this group, patients with CKD may have been treated with renin angiotensin antagonists for amelioration of proteinuria, even in the absence of HTN. Also, the target systolic blood pressure for patients with CKD at our center is the 90th percentile, whereas the target for pHTN is < 95th percentile.
An increase in the afterload on the left ventricle in HTN causes LVH as a compensatory mechanism [13]. The increase in left ventricular mass related to the somatic growth, known as eutrophy, is regulated by growth factors like growth hormone and insulin-like growth factor. Pathological cardiac remodeling, known as hypertrophy, is regulated by neurohormonal signaling pathways and often involves fibrosis of the cardiac tissue [31]. In adults LVH is known to increase the incidence of adverse cardiovascular events by 4.1 fold. Severe LVH has been reported to be associated with longer duration of HTN [32]. Left ventricular remodeling, defined as change in the size, shape, structure, and function of the heart, is seen in patients with HTN [32]. The data on the prevalence of left ventricular remodeling patterns is conflicting. In a study by Radulescu et al., concentric hypertrophy was noted to be more prevalent in males whereas eccentric hypertrophy was common in females with HTN [33]. In that study, it was also noted that concentric hypertrophy was the most common pattern of left ventricular remodeling in patients with CKD. In another study on adult patients with HTN, eccentric hypertrophy was more prevalent than concentric hypertrophy [34]. Sladowska-Kozlowska et al. showed that eccentric hypertrophy is more prevalent in pediatric patients with pHTN [35]. In that study, the main determinants for left ventricular remodeling were visceral obesity and metabolic abnormalities. There is also a well-known association between obesity and increased left ventricular mass [36]. As shown in Fig. 3, our study was in agreement with this finding.
In our study, the most common form of abnormal geometry of the left ventricle was concentric remodeling in both the groups. We also noted that concentric hypertrophy was more prevalent in the CKD-HTN group (CKD-HTN 28% vs. pHTN 13%; p < 0.01). There were no significant associations between the type of left ventricular geometry and the other demographic factors evaluated in our study. We therefore hypothesize that additional factors not evaluated in our study might play a role in left ventricular remodeling in these patients.
Left ventricular remodeling can lead on to diastolic dysfunction [14]. Diastolic function is a measure of the compliance of the myocardium. As the diastolic function worsens, patients develop elevated end diastolic pressures in the left ventricle, which may lead on to increased left atrial pressure, putting them at higher risk for pulmonary edema with fluid overload. There is higher prevalence of diastolic dysfunction in pediatric patients with pHTN and CKD-HTN [11, 37]. Lindblad et al. showed that TDI is more sensitive in diagnosing ventricular diastolic dysfunction in comparison to pulsed-wave Doppler imaging [15]. In our study, there was a high prevalence of diastolic dysfunction in both the groups, with no significant difference. However, the absolute value of the E/A ratio at the left ventricular inflow was significantly lower in the CKD-HTN group in comparison to the pHTN group. This might point to a trend towards more severe diastolic dysfunction in the CKD-HTN group. Pearson correlation analysis showed direct correlation between the renal function and the left ventricular diastolic function.
Dilatation of the aortic root has a well-known association with HTN [38]. In our study, we found that aortic root dimension was higher in the CKD-HTN group when compared to the pHTN group (p = 0.049). We hypothesize that abnormal metabolism in patients with CKD-HTN might have contributed to this observation. Longitudinal studies are needed to confirm this association.
Limitations
The major limitation of this study is its retrospective and cross-sectional study design. Another limitation is the smaller number of study subjects due to exclusion of several subjects from the data analysis in view of missing biochemical results or extended lapse of time between the cardiac evaluation and the biochemical tests. The number of subjects included in regression analysis is also smaller in this study. In addition, there was no data on ambulatory blood pressure in most of the patients, due to its retrospective nature. Thus, it is probable that a significant proportion of subjects with pHTN could have had white coat hypertension, when compared to the CKD-HTN group.
Conclusions
From this study, we may conclude that there is an increased prevalence of diastolic dysfunction in patients with systemic HTN irrespective of whether it is pHTN or CKD-HTN. We found a trend towards more severe diastolic dysfunction in CKD-HTN in comparison to pHTN. There appears to be a direct correlation between the severity of diastolic dysfunction and worsening renal function as measured by GFR. Also, patients with CKD-HTN have larger aortic root dimension when compared to patients with pHTN. There is a need for larger longitudinal studies to confirm these findings.
References
MacMahon S, Peto R, Cutler J, Collins R, Sorlie P, Neaton J, Abbott R, Godwin J, Dyer A, Stamler J (1990) Blood pressure, stroke, and coronary heart disease. Part 1, prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet 335:765–774
Fuentes RM, Notkola IL, Shemeikka S, Tuomilehto J, Nissinen A (2002) Tracking of systolic blood pressure during childhood: a 15-year follow-up population-based family study in eastern Finland. J Hypertens 20:195–202
Burke V, Beilin LJ, Dunbar D (2001) Tracking of blood pressure in Australian children. J Hypertens 19:1185–1192
Flynn JT, Mitsnefes M, Pierce C, Cole SR, Parekh RS, Furth SL, Warady BA, Chronic Kidney Disease in Children Study Group (2008) Blood pressure in children with chronic kidney disease: a report from the Chronic Kidney Disease in Children study. Hypertension 52:631–637. https://doi.org/10.1161/HYPERTENSIONAHA.108.110635
Paoletti E, De Nicola L, Gabbai FB, Chiodini P, Ravera M, Pieracci L, Marre S, Cassottana P, Luca S, Vettoretti S, Borrelli S, Conte G, Minutolo R (2016) Associations of left ventricular hypertrophy and geometry with adverse outcomes in patients with CKD and hypertension. Clin J Am Soc Nephrol 11:271–279. https://doi.org/10.2215/CJN.06980615
Tanaka S, Fujita S, Kizawa S, Morita H, Ishizaka N (2016) Association between FGF23, alpha-klotho, and cardiac abnormalities among patients with various chronic kidney disease stages. PLoS One 11:e0156860. https://doi.org/10.1371/journal.pone.0156860
Leoncini G, Viazzi F, Parodi D, Ratto E, Vettoretti S, Vaccaro V, Ravera M, Deferrari G, Pontremoli R (2004) Mild renal dysfunction and cardiovascular risk in hypertensive patients. J Am Soc Nephrol 15(Suppl 1):S88–S90
Matteucci MC, Wuhl E, Picca S, Mastrostefano A, Rinelli G, Romano C, Rizzoni G, Mehls O, de Simone G, Schaefer F, ESCAPE Trial Group (2006) Left ventricular geometry in children with mild to moderate chronic renal insufficiency. J Am Soc Nephrol 17:218–226. https://doi.org/10.1681/ASN.2005030276
Casale PN, Devereux RB, Milner M, Zullo G, Harshfield GA, Pickering TG, Laragh JH (1986) Value of echocardiographic measurement of left ventricular mass in predicting cardiovascular morbid events in hypertensive men. Ann Intern Med 105:173–178
Richey PA, Disessa TG, Somes GW, Alpert BS, Jones DP (2010) Left ventricular geometry in children and adolescents with primary hypertension. Am J Hypertens 23:24–29. https://doi.org/10.1038/ajh.2009.164
Agu NC, McNiece Redwine K, Bell C, Garcia KM, Martin DS, Poffenbarger TS, Bricker JT, Portman RJ, Gupta-Malhotra M (2014) Detection of early diastolic alterations by tissue Doppler imaging in untreated childhood-onset essential hypertension. J Am Soc Hypertens 8:303–311. https://doi.org/10.1016/j.jash.2014.02.008
de Simone G, Devereux RB, Daniels SR, Koren MJ, Meyer RA, Laragh JH (1995) Effect of growth on variability of left ventricular mass: assessment of allometric signals in adults and children and their capacity to predict cardiovascular risk. J Am Coll Cardiol 25:1056–1062
KL MN, Gupta-Malhotra M, Samuels J, Bell C, Garcia K, Poffenbarger T, Sorof JM, Portman RJ, National High Blood Pressure Education Program Working Group (2007) Left ventricular hypertrophy in hypertensive adolescents: analysis of risk by 2004 National High Blood Pressure Education Program Working Group staging criteria. Hypertension 50:392–395. https://doi.org/10.1161/HYPERTENSIONAHA.107.092197
Alp H, Karaarslan S, Eklioglu BS, Atabek ME, Baysal T (2014) The effect of hypertension and obesity on left ventricular geometry and cardiac functions in children and adolescents. J Hypertens 32:1283–1292. https://doi.org/10.1097/HJH.0000000000000176
Lindblad YT, Axelsson J, Balzano R, Vavilis G, Chromek M, Celsi G, Barany P (2013) Left ventricular diastolic dysfunction by tissue Doppler echocardiography in pediatric chronic kidney disease. Pediatr Nephrol 28:2003–2013. https://doi.org/10.1007/s00467-013-2504-x
Kimball TR, Daniels SR, Loggie JM, Khoury P, Meyer RA (1993) Relation of left ventricular mass, preload, afterload and contractility in pediatric patients with essential hypertension. J Am Coll Cardiol 21:997–1001
Scavarda VT, Pinheiro AC, Costa SD, de Andrade ZM, Carvalhaes JT, Campos O, Carvalho AC, Moises VA (2014) Children with chronic renal disease undergoing dialysis or conservative treatment--differences in structural and functional echocardiographic parameters. Echocardiography 31:1131–1137. https://doi.org/10.1111/echo.12525
Cuspidi C, Meani S, Fusi V, Valerio C, Sala C, Zanchetti A (2006) Prevalence and correlates of aortic root dilatation in patients with essential hypertension: relationship with cardiac and extracardiac target organ damage. J Hypertens 24:573–580. https://doi.org/10.1097/01.hjh.0000209992.48928.1f
Milan A, Avenatti E, Tosello F, Iannaccone A, Leone D, Magnino C, Veglio F (2013) Aortic root dilatation in essential hypertension: prevalence according to new reference values. J Hypertens 31:1189–1195. https://doi.org/10.1097/HJH.0b013e32835f8fda
National Kidney Foundation (2002) K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 39(2 Suppl 1):S1–S266
Hietalampi H, Pahkala K, Jokinen E, Ronnemaa T, Viikari JS, Niinikoski H, Heinonen OJ, Salo P, Simell O, Raitakari OT (2012) Left ventricular mass and geometry in adolescence: early childhood determinants. Hypertension 60:1266–1272. https://doi.org/10.1161/HYPERTENSIONAHA.112.194290
Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, Reichek N (1986) Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol 57:450–458
Lopez L, Colan SD, Frommelt PC, Ensing GJ, Kendall K, Younoszai AK, Lai WW, Geva T (2010) Recommendations for quantification methods during the performance of a pediatric echocardiogram: a report from the Pediatric Measurements Writing Group of the American Society of Echocardiography Pediatric and Congenital Heart Disease Council. J Am Soc Echocardiogr 23:465–495; quiz 576-467. https://doi.org/10.1016/j.echo.2010.03.019
Singh GK, Holland MR (2010) Diastolic dysfunction in pediatric cardiac patients: evaluation and management. Curr Treat Options Cardiovasc Med 12:503–517. https://doi.org/10.1007/s11936-010-0086-5
Eidem BW, McMahon CJ, Cohen RR, Wu J, Finkelshteyn I, Kovalchin JP, Ayres NA, Bezold LI, O'Brian Smith E, Pignatelli RH (2004) Impact of cardiac growth on Doppler tissue imaging velocities: a study in healthy children. J Am Soc Echocardiogr 17:212–221. https://doi.org/10.1016/j.echo.2003.12.005
Khoury PR, Mitsnefes M, Daniels SR, Kimball TR (2009) Age-specific reference intervals for indexed left ventricular mass in children. J Am Soc Echocardiogr 22:709–714. https://doi.org/10.1016/j.echo.2009.03.003
Mitsnefes MM (2012) Cardiovascular disease in children with chronic kidney disease. J Am Soc Nephrol 23:578–585. https://doi.org/10.1681/ASN.2011111115
Li X, Yang HY, Giachelli CM (2008) BMP-2 promotes phosphate uptake, phenotypic modulation, and calcification of human vascular smooth muscle cells. Atherosclerosis 199:271–277. https://doi.org/10.1016/j.atherosclerosis.2007.11.031
Faul C, Amaral AP, Oskouei B, Hu MC, Sloan A, Isakova T, Gutierrez OM, Aguillon-Prada R, Lincoln J, Hare JM, Mundel P, Morales A, Scialla J, Fischer M, Soliman EZ, Chen J, Go AS, Rosas SE, Nessel L, Townsend RR, Feldman HI, St John Sutton M, Ojo A, Gadegbeku C, Di Marco GS, Reuter S, Kentrup D, Tiemann K, Brand M, Hill JA, Moe OW, Kuro OM, Kusek JW, Keane MG, Wolf M (2011) FGF23 induces left ventricular hypertrophy. J Clin Invest 121:4393–4408. https://doi.org/10.1172/JCI46122
Chien SJ, Lin IC, Hsu CN, Lo MH, Tain YL (2015) Homocysteine and arginine-to-asymmetric dimethylarginine ratio associated with blood pressure abnormalities in children with early chronic kidney disease. Circ J 79:2031–2037. https://doi.org/10.1253/circj.CJ-15-0412
Kehat I, Molkentin JD (2010) Molecular pathways underlying cardiac remodeling during pathophysiological stimulation. Circulation 122:2727–2735. https://doi.org/10.1161/CIRCULATIONAHA.110.942268
Daniels SR, Loggie JM, Khoury P, Kimball TR (1998) Left ventricular geometry and severe left ventricular hypertrophy in children and adolescents with essential hypertension. Circulation 97:1907–1911
Radulescu D, Stoicescu L, Buzdugan E, Donca V (2013) Patterns of left ventricular remodeling among patients with essential and secondary hypertension. Rev Med Chil 141:1520–1527. https://doi.org/10.4067/S0034-98872013001200004
Ganau A, Devereux RB, Roman MJ, de Simone G, Pickering TG, Saba PS, Vargiu P, Simongini I, Laragh JH (1992) Patterns of left ventricular hypertrophy and geometric remodeling in essential hypertension. J Am Coll Cardiol 19:1550–1558
Sladowska-Kozlowska J, Litwin M, Niemirska A, Wierzbicka A, Wawer ZT, Janas R (2011) Change in left ventricular geometry during antihypertensive treatment in children with primary hypertension. Pediatr Nephrol 26:2201–2209. https://doi.org/10.1007/s00467-011-1916-8
Dhuper S, Abdullah RA, Weichbrod L, Mahdi E, Cohen HW (2011) Association of obesity and hypertension with left ventricular geometry and function in children and adolescents. Obesity (Silver Spring) 19:128–133. https://doi.org/10.1038/oby.2010.134
Mitsnefes MM, Kimball TR, Border WL, Witt SA, Glascock BJ, Khoury PR, Daniels SR (2004) Impaired left ventricular diastolic function in children with chronic renal failure. Kidney Int 65:1461–1466. https://doi.org/10.1111/j.1523-1755.2004.00525.x
Covella M, Milan A, Totaro S, Cuspidi C, Re A, Rabbia F, Veglio F (2014) Echocardiographic aortic root dilatation in hypertensive patients: a systematic review and meta-analysis. J Hypertens 32:1928–1935; discussion 1935. https://doi.org/10.1097/HJH.0000000000000286
Author information
Authors and Affiliations
Contributions
Dr. Paris and Dr. Arenas-Morales performed the data collection, drafted the initial manuscript, and approved the final manuscript as submitted. Dr. Gorla critically reviewed and approved the final manuscript as submitted. Dr. Swaminathan and Dr. Seeherunvong have equally contributed to the manuscript preparation. Both together, conceptualized and designed the study, supervised the data collection and statistical analysis, edited, approved, and revised the final manuscript as submitted.
Corresponding author
Ethics declarations
Ethics
This was a retrospective chart review and was approved by the Institutional Review Board of Human Subjects Research at the University of Miami and Holtz Children’s Hospital.
Financial disclosure
The authors have no financial relationships relevant to this manuscript to disclose.
Conflict of interest
All authors declared that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Paris, G., Gorla, S.R., Arenas-Morales, A.J. et al. Comparison of echocardiographic changes in children with primary hypertension and hypertension due to mild to moderate chronic kidney disease. Pediatr Nephrol 34, 487–494 (2019). https://doi.org/10.1007/s00467-018-4096-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-018-4096-y