Abstract
Background
The aim of this study was to investigate whether dalteparin is a safe and effective anticoagulant for paediatric home haemodialysis (HD) and to assess the determinants of dosing.
Methods
Data were collected for all children (< 18 years) undergoing home HD from 2011 to 2017 at one large paediatric nephrology centre in the UK. All children had anticoagulation with dalteparin sodium according to a standardised protocol. Dalteparin safety was assessed by monitoring for accumulation, adequate clearance of dalteparin and adverse events. Dalteparin efficacy was assessed through monitoring for clot formation in dialysis circuits. Potential determinants of dalteparin dosing were assessed.
Results
Eighteen children were included, their median age at start was 12 years, and 50% were male. Eighty-three percent of children had four home HD sessions each week, with a median total dialysis hours of 20 h/week. Thirty-three percent of children had nocturnal home HD. Median dalteparin dose at 12-month follow-up was 40 IU/kg (range 8–142 IU/kg). Factors associated with higher dalteparin dosing requirements included a younger age of the child (p < 0.01), a lower blood flow rate (p < 0.01) and the use of a central venous line for dialysis access (p = 0.038). No children had evidence of bioaccumulation of dalteparin or inadequate clearance. No significant bleeding or adverse events were reported.
Conclusions
Dalteparin is a safe and effective anticoagulant when used for paediatric home HD. In this study, there was no evidence of bioaccumulation or significant adverse events. Further research is required to directly compare dalteparin with unfractionated heparin (UFH) and evaluate anticoagulant choice for paediatric home HD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Children with chronic kidney disease (CKD) stage 5 will eventually require a form of renal replacement therapy (RRT). Although renal transplantation is the gold-standard form of RRT, this may not be immediately possible for a variety of reasons. Some children will therefore require treatment with chronic dialysis. In the United Kingdom (UK), most children on chronic dialysis will have peritoneal dialysis (PD), but approximately a third of children will be on haemodialysis (HD). Worldwide, the proportion of children on HD is higher [1].
Peritoneal dialysis is generally preferred for children with CKD for a number of reasons, one of the main ones being the ability to perform PD at home, while most HD is performed a number of times each week in the hospital setting. Home HD is a relatively underutilised option for children, with limited experience of this technique in many centres. Despite this, home HD has shown to have significant advantages compared to traditional hospital HD, including increased flexibility, quality of life and other positive health measures [2].
Compared to PD performed at home, patient selection criteria for home HD are more stringent [2]. HD is inherently a more risky method of dialysis, and there are more potential technical complications with both equipment and the process itself. Therefore, patients on home HD need to be very motivated and undergo intensive training [2]. One important technical consideration in HD is the risk of clotting and the methods to prevent this.
HD circuits are prone to clotting due to activation of both the intrinsic and extrinsic pathways of the coagulation cascade. Thrombin formation occurs after tissue factor is expressed on the surface of leukocytes and other cells. This occurs at a number of points of potential shear stress and turbulence in the dialysis circuit, including the vascular access or the blood pump [3]. This effect is exaggerated in paediatric HD circuits due to their smaller diameter and potentially lower flow rates, particularly in smaller children and infants [4].
Clotting in an HD circuit can affect the quality and quantity of dialysis provided and can prematurely stop the dialysis process. Traditionally unfractionated heparin (UFH) has been used, often as an initial bolus dose and then a continuous infusion or a second bolus dose [5]. Unfractionated heparin does have a number of disadvantages in this context, including the risk of heparin-inducted thrombocytopenia (HIT) and the need to give more than one initial bolus dose [6].
Over the past 20 years, there is an increasing body of adult patient literature supporting the use of low-molecular-weight heparins (LMWHs) for anticoagulation during HD. LMWHs provide substantial advantages over UFH, including a more reliable clinical effect and ease of administration with a single bolus dose at the start of HD, all that is required [3]. In paediatric practice, however, UFH remains the most common anticoagulant during dialysis. There have been concerns with the potential for accumulation of LMWH, more difficult reversal of clinical effect and less readily available monitoring tests [3].
There is a paucity of paediatric literature on the use of LMWH in HD, and the literature on home HD is generally limited to a number of single-centre case series [7, 8]. To our knowledge, there have been no previous studies reporting the use of LMWH in paediatric home HD. The aim of this study was to assess whether dalteparin (a LMWH) is a safe and effective anticoagulant for home HD and to determine the factors affecting the dose required.
Methods
Study design
This was a retrospective observational study of all children (aged < 18 years) undergoing home HD treatment from 2011 to 2017 at a large paediatric nephrology unit in the UK. All children were given dalteparin sodium as the LMWH for anticoagulation during home HD treatment.
Patient clinical data
Data was collected from patient case records and dialysis records and inputted into a standardised proforma. The following data were collected: baseline demographic characteristics, underlying renal pathology, dialysis regimen including equipment and flow rate, initial dose of dalteparin used, changes to dalteparin dose. The method of dialysis access was recorded, either as arteriovenous fistula (AVF) or central venous line (CVL). In children who used an AVF, bleeding times after needle removal were recorded. Clot formation was assessed after each dialysis session. Patient records of clot formation and dialysis interruption were also examined, and any adverse events were recorded.
Protocol for dalteparin prescribing
Dalteparin anticoagulation has not previously been used in paediatric home HD, and so our institution started this practice in a small number of paediatric home HD patients under close supervision. The prescribing and monitoring protocol followed institutional guidelines and was developed in consultation with clinical haematology staff. Dalteparin dosing was limited below maximum safe dosages for the use of this medication in our institutional guidelines. The first five patients started on dalteparin for paediatric home HD were capped at a maximum starting dose of 1000 IU to ensure safety. Doses were increased as below for subsequent patients.
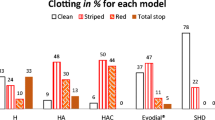
There was a standardised protocol for using dalteparin in this setting at our unit; each child was administered a single intravenous dose of 50 IU/kg through the arterial arm of the dialysis circuit within the first 15 min of treatment, unless there was a clinical reason to start with a different dose. Doses were rounded to a sensible administration dose. At the end of the first dialysis treatment, the circuit and dialyser were analysed for clot formation. If more than 25% clots were present in the dialyser or several large clots were present in the circuit, the dalteparin dose was increased by 10% for the subsequent treatment. This process was repeated until a final dose of dalteparin was achieved that resulted in minimal clot formation (defined as < 25% clots present in dialyser and no large clots in the dialysis circuit). The dalteparin dose was reduced if there was any evidence of significant bleeding events or prolonged bleeding from an AVF in children dialysed in this way. The dalteparin dose was increased if a child was moving from daytime to nocturnal home HD.
Follow-up data and laboratory monitoring
Follow-up data was collected at 3, 6 and 12 months after starting home HD. Laboratory monitoring data was also collected, including factor anti-Xa levels at the start and end of dialysis session. Anti-Xa activity was measured using a chromogenic assay; the lower limit of detection was 0.05 IU/ml. An anti-Xa level of < 0.2 IU/ml at the end of dialysis was considered adequate clearance. In addition, an anti-Xa level of > 0.2 IU/ml at the start of dialysis was considered to be evidence of accumulation. The level of 0.2 IU/ml is used as it is the lower reference limit in our institutional laboratory. Blood platelet levels were measured pre- and post-dialysis, as well as blood haemoglobin levels pre-dialysis.
Determinants of dalteparin dosing
Starting and final dalteparin dose required to ensure effective home HD (an absence of clotting) was recorded and expressed as IU/kg. Data was collected on potential determinants of dalteparin dosing at follow-up, this included age of child, duration of dialysis session and blood flow rate for dialysis. The final dalteparin dose required was also compared between dialysis access methods (AVF vs. CVL).
Statistical analysis
Baseline characteristics and clinical data are presented as summary statistics. Laboratory data and anti-Xa monitoring are also expressed as summary statistics. Medians were used due to the small number of children included in this study. Potential determinants of dalteparin dosing were assessed for a correlation using Spearman’s rank test, these included age of child, duration of dialysis session and blood flow rate for dialysis. The final dalteparin dose required for different dialysis access methods was compared using the Mann-Whitney U test. All statistical tests were two-tailed, and a significance level of p < 0.05 was used. Statistical tests were performed using SPSS version 22.0 (SPSS Inc., Chicago, IL).
Results
Study population
Twenty-two children were started on home HD treatment during the study period; follow-up data is available for 18 children (some children were subsequently managed in different paediatric nephrology centres). Table 1 shows the summary of baseline characteristics and clinical data for the 18 children included in this study.
Determinants of dalteparin dosing
Table 2 shows the median and range of dalteparin doses (expressed as IU/kg) at the start of home HD and at 12-month follow-up. These data have been split to show differences between children dialysed by AVF vs. CVL, as well as across different age groups. During the follow-up period, 9/18 children (50%) had their dalteparin dose increased, 5 of these were because the child was moving from daytime to nocturnal home HD, 3 were due to clots being found in the dialysis circuit and one reason was not recorded. Three of seven (43%) children dialysed through an AVF had a prolonged bleeding time during the 12-month follow-up period, requiring a dalteparin dose reduction. There were no significant bleeding events causing patient harm during the study.
Possible determinants of dalteparin dosing were assessed by using the final dalteparin dose (IU/kg) and correlating against the age of the child, duration of dialysis (duration of each session) and blood flow rate of dialysis.
Using Spearman’s rank test, age was significantly associated with final dalteparin dose (R = − 0.8, p < 0.01). The negative correlation demonstrates that children of a younger age generally require a higher dalteparin dose to achieve adequate anticoagulation for home HD.
The duration of dialysis session was not significantly associated with final dalteparin dose (R = 0.11, p = 0.66).
Blood flow rate was significantly associated with final dalteparin dose (R = − 0.76, p < 0.01). The negative correlation demonstrates that children on lower blood flow rates generally require a higher dalteparin dose to achieve adequate anticoagulation for home HD.
The method of access was also assessed as a possible determinant of dalteparin dosing. The median final dose of dalteparin required for children on home HD with an AVF was 22 IU/kg, while the median final dose of dalteparin required for children on home HD through a CVL was 44 IU/kg. Using the Mann-Whitney U test, value was p = 0.038; therefore, dalteparin dosing was significantly higher in the CVL group compared to the AVF group.
Follow-up data and laboratory monitoring
All children on home HD were monitored for anti-Xa levels before dialysis (to detect dalteparin accumulation) and after dialysis (to assess for adequate clearance). As well as this, platelet counts were measured, and clots in the dialysis circuit were recorded to assess for adverse events and adequacy of anticoagulation.
The median anti-Xa level before dialysis was 0 (range 0–0.17) IU/ml, and no children had evidence of dalteparin accumulation. The median anti-Xa level after dialysis was 0 (0–0.08) IU/ml, with no children showing inadequate clearance. The median platelet count at 12-month follow-up was 233.5 × 109/l. Three of eighteen children (17%) were thrombocytopenic (platelet count < 150 × 109/l) at 12-month follow-up.
Discussion
This study describes the use of LMWH (dalteparin) for anticoagulation in children on home haemodialysis. Although limited by a small number of children and its retrospective nature, this study has demonstrated that dalteparin can be safely and effectively used instead of unfractionated heparin for anticoagulation in paediatric home HD. In addition, this study has identified a number of factors that are associated with the dose of dalteparin required, including the age of the child, blood flow rate and dialysis access type. These factors may be of assistance when determining dalteparin dosing levels.
In this study of 18 children on home HD with 12-month follow-up, there were no significant patient adverse events reported. There was one record of significant clotting in the dialysis circuit for one child and two occurrences of minor clots in the dialysis circuit, these all resolved with an increased dalteparin dose in future dialysis sessions. Three children were thrombocytopenic at 12-month follow-up, but one of these children had known ITP. Although three children had prolonged bleeding from AV fistulae in this study requiring a dalteparin dose reduction, there were no significant bleeding events reported in any children in this study.
Anti-Xa levels were monitored before and after dialysis sessions, to assess for bioaccumulation (a high anti-Xa level pre-dialysis) and inadequate clearance (high anti-Xa level at the end of dialysis). None of the children in this study had any evidence of bioaccumulation or inadequate clearance of dalteparin from their laboratory monitoring during this study. This is relevant as some of the reluctance to use LMWH for paediatric HD stems around concerns about bioaccumulation.
In this study, we considered a number of potential determinants of dalteparin dosing, and although the small number of children included in this study limits the conclusions we can draw, a number of factors were significantly associated with dalteparin dosing. We found that younger children and those on lower blood flow rates required a higher dose of dalteparin to maintain adequate anticoagulation. In addition, children with a central venous line required higher dalteparin doses compared to children with an AV fistula, but this was of borderline statistical significance.
There are several possible explanations for these findings; firstly, smaller children often require a proportionally higher dose per kilogramme of body weight to achieve the same effect. In addition, in smaller children, the ratio of dialysis circuit to total body volume is higher, potentially increasing the risk of clotting and increasing the required dose of dalteparin. Those children on lower blood flow rates required higher doses of anticoagulation, which may be explained by the fact that lower flows provide more blood stasis and therefore a higher risk of thrombosis. The higher dalteparin dose required for children with a CVL compared to those with an AVF may be explained by the dose reductions in children with an AVF who had prolonged bleeding. In addition, higher blood flow rates are generally achieved through an AVF, and this may be contributing.
There are a number of potential advantages to using LMWH for paediatric home HD, including a single bolus dose administration and a more reliable clinical effect. Clearly, it is of paramount importance that safety is guaranteed, and bleeding events are minimised, and this is emphasised in the home setting where immediate medical assistance is not available. We believe that the results of our study can provide confidence to clinicians who are considering LMWH for home HD, as they have not raised any significant safety concerns in this study.
As mentioned previously, our study is substantially limited by the small number of children on home HD treatment. However, home HD is likely to increase in availability with time as clinical services adapt, and we believe these results will help to guide clinicians in deciding which anticoagulant to choose. A further limitation to our results is that although we have identified some determinants of dalteparin dosing, the final range of doses required is very wide in our study (8–142 IU/kg); therefore, there are clearly many other factors that mean that dalteparin dosing must remain patient-specific and must be carefully adjusted over time to achieve adequate and safe anticoagulation.
In conclusion, this retrospective study of 18 children on home HD demonstrates that dalteparin is a safe and effective anticoagulant for this setting. The dosing of dalteparin is difficult to predict and must be carefully monitored. This study has identified the age of the child, blood flow rate and dialysis access type as factors affecting dalteparin dosing. Further research is required in a larger population to more accurately assess the pharmacodynamics and pharmacokinetics of dalteparin in the context of paediatric home HD. In particular, an experimental study comparing the use of LMWH with UFH in this setting would help to give further reassurance that dalteparin and other LMWH’s are safe and effective anticoagulants in this context, as well as to demonstrate whether there is any superiority to using LMWHs over UFH.
References
Kaur A, Davenport A (2014) Hemodialysis for infants, children and adolescents. Hemodial Int 18:573–582
Hothi DK, Stronach L, Sinnott K (2016) Home hemodialysis in children. Hemodial Int 20:349–357
Davenport A (2009) Review article: low-molecular-weight heparin as an alternative anticoagulant to unfractionated heparin for routine outpatient haemodialysis treatments. Nephrology 14:455–461
Davenport A (2012) Alternatives to standard unfractionated heparin for pediatric hemodialysis treatments. Pediatr Nephrol 27:1869–1879
Sagedal S, Hartmann A, Sundstrøm K, Bjørnsen S, Brosstad F (1999) A single dose of dalteparin effectively prevents clotting during haemodialysis. Nephrol Dial Transplant 14:1943–1947
Hofbauer R, Moser D, Frass M, Oberbauer R, Kaye AD, Wagner O, Kapiotis S, Druml W (1999) Effect of anticoagulation on blood membrane interactions during hemodialysis. Kidney Int 56:1578–1583
Goldstein SL, Silverstein DM, Leung JC, Feig DI, Soletsky B, Knight C, Warady BA (2008) Frequent hemodialysis with NxStage system in pediatric patients receiving maintenance hemodialysis. Pediatr Nephrol 23:129–135
Geary DF, Piva E, Tyrrell J, Gajaria MJ, Picone G, Keating LE, Harvey EA (2005) Home nocturnal hemodialysis in children. J Pediatr 147:383–387
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics
This study was approved through institutional audit and did not require separate ethical approval as it was retrospective. All data extraction and analysis were performed by members of the clinical care team.
Disclosures
None.
Rights and permissions
About this article
Cite this article
Lutkin, M., Stronach, L., Yadav, P. et al. Dalteparin anticoagulation in paediatric home haemodialysis. Pediatr Nephrol 33, 2337–2341 (2018). https://doi.org/10.1007/s00467-018-4032-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-018-4032-1