Abstract
Background
The 2011 annual report of the North American Pediatric Renal Transplant Cooperative Study (NAPRTCS) registry comprises data on 6482 dialysis patients over the past 20 years of the registry.
Methods
The study compared clinical parameters and patient survival in the first 10 years of the registry (1992–2001) with the last decade of the registry (2002–2011).
Results
There was a significant increase in hemodialysis as the initiating dialysis modality in the most recent cohort (42% vs. 36%, p < 0.001). Patients in the later cohort were less likely to have a hemoglobin <10 g/dl [odds ratio (OR) 0.68; confidence interval (CI) 0.58–0.81; p < 0.001] and height z-score <2 standard deviations (SD) below average (OR 0.68, CI 0.59–0.78, p < 0.0001). They were also more likely to have a parathyroid hormone (PTH) level two times above the upper limits of normal (OR 1.39, CI 1.21–1.60, p < 0.0001). Although hypertension was common regardless of era, patients in the 2002–2011 group were less likely to have blood pressure >90th percentile (OR 1.39, CI 1.21–1.60, p < 0.0001), and a significant improvement in survival at 36 months after dialysis initiation was observed in the 2002–2011 cohort compared with the 1992–2001 cohort (95% vs. 90%, respectively). Cardiopulmonary causes were the most common cause of death in both cohorts. Young age, growth deficit, and black race were poor predictors of survival.
Conclusions
The survival of pediatric patients on chronic dialysis has improved over two decades of dialysis registry data, specifically for children <1year.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The North American Pediatric Renal Transplant Cooperative Study (NAPRTCS) was established in 1987 to follow children and adolescents in North American who underwent renal transplantation. In 1992, the registry grew to include patients receiving hemodialysis (HD) or peritoneal dialysis (PD). In 2001, a NAPRTCS report describing the dialysis registry and trends in the management of pediatric patients on dialysis was published [1]. Since that report, the National Kidney Foundation sponsored Kidney Disease Outcomes Quality Initiative (KDOQI) composed updated clinical practice guidelines for managing patients on dialysis with the aim of improving quality of life (QoL) and lowering the high mortality rates in patients with chronic kidney disease (CKD) and end-stage renal disease (ESRD) [2, 3]. In this report, we present data from the second decade of the NAPRTCS dialysis registry and compare outcomes of patients who initiated dialysis in the first (1992–2001) vs the second (2002–2011) decade of the registry to assess the possible impact of KDOQI guidelines and advances in ESRD management.
Patients and methods
NAPRTCS involves both a data registry and a prospective trials division. For the registry division, participating centers throughout North America submit data on patients younger than 21 years at the time of enrollment with CKD, initiated dialysis, or received a kidney transplantation. The analysis focuses on children enrolled in the dialysis registry. Local institutional review board approval was obtained at each center for data entry.
The data collected from each center are sent on a voluntary basis to a data coordinating center. An initial registration form is completed, with follow-up status forms submitted 30 days and 6 months after initiation of dialysis and then every 6 months thereafter. An independent course of dialysis therapy is defined as a patient being maintained on a given modality for ≥30 days. The index course is dialysis occurring at the time of enrollment to NAPRTCS. As such, this analysis included only incident patients. One hundred and thirty-five centers contributed data to this analysis, of which, eight were Canadian. One hundred and thirty-three centers (including the eight Canadian) contributed data to the 1992–2001 and 92 (including eight Canadian) to the 2002–2011 cohorts. Of these, 90 centers provided data throughout both decades of the registry.
Standard univariate and multivariate statistical methods were used for data analysis. Continuous variables were assumed to follow a Gaussian distribution. Chi-squared tests were performed to compare era in binary and categorical endpoints. Kaplan–Meier product-limit estimates of time to dialysis modality termination, peritonitis incidence, and survival were created by era and were compared using the log-rank test. Multivariate logistic regression controlling for race, sex, age group, primary diagnosis, and modality was used to assess the effect of era on outcome parameters measured at 6 months after dialysis initiation. Outcome parameters were anemia stratified by hemoglobin groups of <10 g/dl vs. 10–12 g/dl vs. >12 g/dl. We controlled for erythropoietin-stimulating agent use and iron supplementation; hyperparathyroidism stratified by parathyroid hormone (PTH) more than twice the upper limits of normal (ULN) vs. less than twice the ULN controlling for vitamin D supplementation; elevated blood pressure stratified by blood pressure ≥ 90th percentile vs. <90th percentile and use of blood pressure medications; growth stratified by height standardized score < −2 SD vs. ≥ − 2 SD, and for the use of growth hormones [4, 5]. If hemoglobin values were missing, comparable hematocrit ranges were used to evaluate anemia.
Patient survival was assessed in two ways: Death while on the first dialysis modality analyzes time of dialysis initiation to death, with censoring for dialysis termination or last follow-up. The second method calculated patient survival from dialysis initiation to the last NAPRTCS follow-up, where patients are followed through registry changes (i.e., transplant or change in dialysis modality) until death or their last NAPRTCS visit. Cox regression analysis was used to estimate the effect of anemia, hyperparathyroidism, and hypertension and growth deficit at 6 months on survival while on dialysis. Patients were required to be followed for 6 months. This model was also adjusted for era, age group, race, gender, primary diagnosis, growth hormone use, and modality. To control for center-specific effects, a frailty analysis was performed in which each center was assumed to have a random effect that indicated the possibility of different baseline risks for patients at different centers. Unobserved center-level factors common to all patients from that center were accounted for in such an analysis. All statistical analysis was performed using the SAS System for Windows, v9.2 or v9.3 (SAS Institute, Cary, NC, USA).
Results
Patient and dialysis characteristics
Through 2011, 6482 patients were enrolled in the NAPRTCS dialysis registry. Of these, 4373 were enrolled from 1992 to 2001 and 2109 from 2002 to 2011. Selected demographic characteristics of both are presented in Table 1. There was no difference gender distribution between cohorts, with a slight male predominance at 55.8%. Compared to the 1992–2001 cohort, fewer white patients initiated dialysis in the 2002–2011 cohort (46% vs. 49%, p = 0.006). While mean age at dialysis initiation was similar in both cohorts (10.8 years and 10.7 years in earlier and later cohorts, respectively), more patients aged 6–12 (32% vs. 28%) were noted in the earlier cohort and more aged 13–17 (38% vs. 41%) in the later (p = 0.002). The leading cause of ESRD was renal aplasia/hypoplasia/dysplasia in the early cohort compared with focal segmental glomerulosclerosis (FSGS) in the later (p = 0.047). A statistically significant trend toward increased use of HD as the initial dialysis modality was noted between cohorts, with 36% of patients initiating renal replacement therapy on HD in the earlier compared with 42% in the later cohort (p < 0.001).
One hundred and thirty-five centers contributed data, with 133 contributing to the 1992–2001 and 92 to the 2002–2011 cohorts; 90 contributed to both decades. To minimize selection bias, demographic data from those centers only were compared, and results were similar to the entire cohort. We limited data to 90 centers and 5734 patients (3641 in 1992–2001 and 2093 in 2002–2011). There was no difference in gender distribution between cohorts (p = 0.96). Fewer white patients initiated dialysis in the 2002–2011 cohort (46% vs. 51%; p = 0.001). Mean age at dialysis was similar between cohorts, although more patients aged 6–12 (32% vs 28%) were enrolled in the earlier cohort and more aged 13–17 (38% vs 41%) in the later (p < 0.002). The leading cause of ESRD remained renal aplasia/hypoplasia/dysplasia in the early cohort compared with FSGS in the later (p = 0.029). A statistically significant trend toward increased use of HD as the initial modality was noted, with 35% of patients in the earlier group compared with 42% in the later cohort (p < 0.001).
Dialysis termination
As of the end of 2011, 5111 (795) registry patients terminated dialysis, leaving 1371 cases of active dialysis in the registry; 82% of cases terminated in the earlier cohort and 73% in the later (p = 0.86). Regardless of cohort, most terminations were due to renal transplantation (69%) and subsequent changes in dialysis modality (17%) (Table 2) (p = 0.79). The primary reason for change in dialysis modality in the earlier cohort was excessive infection compared with patient/family choice in the later (p = 0.039). Regardless of cohort, PD (PD) patients were more likely to change modality due to infection, whereas HD dialysis patients were more likely to change modality due to patient choice (data not shown). Access failure, inadequate ultrafiltration, and inadequate solute clearance accounted for a combined 18% of modality changes in the earlier and 16% in the later era (Table 2) (p = 0.68). Similar results were observed when comparing the 90 centers that contributed data to both decades (data not shown).
Dialysis access
PD catheter characteristics are described in Table 3. A curled, single cuffed catheter with a straight tunnel and a lateral exit site was the most common access in the earlier cohort (15%) compared with a curled double-cuffed catheter with a swan-necked tunnel and downward-oriented exit site in the latter (20%) (p < 0.001). The proportion of catheters with a curled, intraperitoneal segment remained stable across both eras at >60% (p = 0.61), but more double-cuffed catheters were used in the more recent cohort (52% vs 41%; p < 0.001). In addition, catheters with a swan neck or curved vs straight tunnel were more common in the more recent group (p = 0.023). Transition away from upwardly and laterally oriented exit sites was also seen (p = 0.011). Similar results were observed when comparing data solely from the 90 centers that contributed data to both decades (data not shown).
In HD patients, regardless of era, central venous catheters were the most common form of access at the time of initiation (81% in the early cohort vs. 76% in the more recent cohort (p = 0.75). The use of jugular venous catheters was more common in the 2002–2011(69% vs. 32%, respectively; χ2 p < 0.001). A corresponding decrease in the use of subclavian catheters was also noted in the later cohort(26% vs. 63%; p < 0.001). The use of arteriovenous fistulae and arteriovenous grafts at dialysis initiation remained low regardless of era, at 12.8% vs 11.3% and 9.5% and 2.1% (p = 0.87). Similar results were observed when comparing data solely from the 90 centers that contributed data to both decades (data not shown).
Clinical performance measures
Anemia management
At 6 months following initiation of dialysis, patients in the 2002–2011 cohort were more likely to have a hemoglobin >10 g/dl (79%) compared with the earlier cohort (67%) (Table 4). In fact, a logistic regression model adjusting for age, race, gender, primary diagnosis, modality, erythropoietin stimulating agent (ESA) use, and iron supplementation showed that patients in the 2002–2012 cohort were more likely to maintain a hemoglobin >12 g/dl [odds ratio (OR) 2.06; confidence interval (CI) 1.77–2.39; p < 0.001) multivariate analysis showed those patients were less likely to a have hemoglobin <10 g/dl (OR 0.68; CI 0.58–0.81; p < 0.001) compared with those initiating dialysis between 1992 and 2001. ESA use was common in both cohorts (93% and 91%, respectively). Iron supplementation remained steady over the years (79% in 1992–2001 vs. 78% in 2002–2011); there was, however, a shift from iron supplementation orally (75% vs. 58%) to IV (12% to 24%) between the early and later eras.
Hyperparathyroidism
In the NAPRTCS registry, PTH levels are reported as <2× or >2× the ULN. At 6 months following dialysis initiation, there was a trend toward higher PTH levels in the 2002–2011 cohort, with 61% of patients with a PTH >2× the ULN compared with 54% in the earlier cohort (Table 4). More patients were also noted to have a PTH level <2× the ULN in the 1992–2001 group (46% vs.. 39%). A logistic regression model controlling for race, gender, primary diagnosis, modality, and vitamin D supplementation confirmed that patients in the 2002–2012 were more likely to have a PTH >2× the ULN (OR 1.39, CI 1.21–1.60, p < 0.001).
Hypertension management
Hypertension is defined in the registry by a blood pressure ≥90th percentile of standardized blood pressures for age, height, and gender according to the the Fourth Report on the Diagnosis, Evaluation and Treatment of High Blood Pressure in Children and Adolescents [4]. More patients in the 1992–2001 cohort were ≥90th percentile 6 months after dialysis initiation compared with the 2002–2011 group (64% vs. 58%). Similar results were obtained using the 95th and 99th percentiles for age, height, and gender; More patients in the later cohort were on antihypertensive therapy (59% vs 53%) (Table 4). A significant number of patients remained hypertensive in the 2002–2011 group (Table 4), but logistic regression modeling showed that they were less likely to be hypertensive than patients who initiated dialysis between 1992 and 2001 (OR 0.71, CI 0.62–0.81, p < 0.001). Results were similar when patients on PD and HD were compared. Regardless of era, a higher percentage of HD patients (64%) were on antihypertensive therapy compared with those on PD (51%).
Growth deficit
The use of recombinant human growth hormone (rhGH) at 6 months postdialysis initiation remained low, at 17% in the later and 12% in the earlier cohort. Standardized height z-scores were calculated by adjusting for the appropriate population-, age-, and sex-specific levels for the normal population provided by the 2000 US National Institutes of Health Centers for Disease Control growth charts [5]. The earlier cohort demonstrated a mean (SD) standardized z-score of −1.73 ± 1.63 [with 41% < −2 standard deviation scores (SDS)) compared with a significant improvement in mean standardized z-score in the later cohort of −1.49 ± 1.60 (with 33% < −2 SDS) (Table 4). Patients were less likely to have a height standardized z-score <2 SDS in the 2002–2012 compared with the 1992–2001 era (OR 0.68, CI 0.59–0.78, p < 0.001, Table 4).
Dialysis adequacy
Patient Kt/v data has only been collected by the registry since 2002, so dialysis eras were not compared for this parameter. At 6 months postdialysis initiation, 73% of patients on HD maintained a Kt/v >1.2 and 56% on PD a Kt/V of ≥2.0. When patients on PD and HD with goal Kt/v were compared to those below the goal, there was no difference in survival.
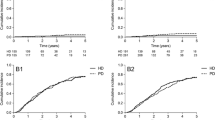
Patient survival
Of the 6482 patients in the dialysis registry, 539 (8.3%) died. Survival while on dialysis and overall survival (OS) are shown in Fig. 1a, b. Survival estimates were 98%, 96%, and 95% at 12, 24, and 36 months, respectively, in the 2002–2011 group compared with 95%, 91%, and 90% at 12, 24, and 36 months, respectively in the 1992–2001 cohort (Fig. 1a). Across both cohorts, patient survival remains lowest for patients <1 year at the time of initiation of dialysis, but there was a significant improvement in survival in the later cohort (p < 0.001) (Fig. 2).
Patient survival in the dialysis registry. a Patients on their first course of dialysis, with censoring for dialysis termination or last-follow-up. b Patients who initiated dialysis in the registry and were followed through registry changes, including transplant or change in dialysis modality, until death or their last follow-up
The leading specified cause of death remained cardiopulmonary regardless of age group (114/538, 21.1%); there was no difference in cause of death by time period (Table 5). At 6 months, there were 4343 dialysis patients still alive and receiving dialysis. Of those, 3389 had complete data on all covariables and were included in Cox regression analysis. In this group of 3389, there were 107 subsequent deaths (3.2%). In the adjusted model, young age, growth deficit, and black race were all poor predictors of survival (Table 6). Similar results were obtained using frailty analysis to model correlations between failures of the same cluster by using a random component for the hazard function. In this analysis, “center” was the random cluster; when it was added to the Cox regression model, it was not significant, and results of the other covariates were similar to the initial model (Table 7).
Discussion
This report summarizes data on >6000 children enrolled in the NAPRTCS dialysis registry since 1992. The results indicate improvements in several key clinical performance measures, such as anemia, growth, and blood pressure control, over the 2002–2011 decade collection compared with the 1992–2001 time period. A higher percentage of patients in the later cohort maintained a hemoglobin >10 g/dl at 6 months. The effects of uncontrolled anemia in pediatric patients on dialysis are well documented, including decreased QoL, development of left ventricular hypertrophy, increased risk of hospitalization, and increased mortality rates [6, 7]. A study from the International Pediatric Peritoneal Dialysis Network noted that a hemoglobin <11 g/dl was associated with increased mortality [8]. A separate study of 677 adolescents on HD using data from the US Centers for Medicare andMedicaid Services End-Stage Renal Disease Clinical Performance Measures (CMS-ESRD-CPM) project found that patients who did not achieve a hemoglobin target of 11–12 g/dl were at increased risk for mortality [9]. Using data from the US Renal Data System (USRDS), Dahlinghaus et al. found that increased dose of ESA (used as a marker of more significant anemia) was associated with increased hospitalizations and mortality [10]. Cognizant of these adverse outcomes in children with lower hemoglobin levels, current KDOQI and Kidney Disease–Improving Global Outcomes (KDIGO) guidelines recommend that a hemoglobin level of 11–12 g/dl should be achieved in infants, children, and adolescents on dialysis [2]. It is not clear whether these therapeutic targets are optimal, since there have been no prospective trials to evaluate the effect of different higher hemoglobin targets on outcomes in children and adolescents. In the absence of such data, current targets are mostly based on adult studies showing that a hemoglobin >13.5 g/dl was associated with increased cardiovascular and cerebrovascular events [11].
Similar to the improvement in anemia seen over time, a higher percentage of patients in the more recent cohort maintained blood pressures <90th percentile for age, height, and gender compared with the earlier cohort. In addition, more patients in the recent era were on antihypertensive therapy. However, registry data confirms previous findings that hypertension in the dialysis population remains undertreated, with >50% of registry patients continuing to demonstrate blood pressures >90th percentile despite most pediatric nephrologists intending to maintain lower targets [12]. Since hypertension is associated with intermediate outcomes on cardiovascular health, including development of left ventricular hypertrophy and cardiac dysfunction, ongoing improvements in hypertension management may lead to ongoing improvements in survival [13].
Data from the registry show that a higher percentage of patients in the latest era had a PTH level twice the ULN, suggesting that providers are tolerating higher PTH levels than in previous years. As with hemoglobin, the ideal serum PTH level in pediatric patients on dialysis is not known, but there has been increasing attention to data suggesting the need to allow a degree of hyperparathyroidism to encourage normal bone turnover; this is reflected in PTH targets found in KDOQI and KDIGO guidelines [14]. Maintaining a normal PTH level in the setting of dialysis is thought to lead to adynamic bone disease, but data also suggest that very high levels are linked to both bone and cardiovascular disease [15] and are specifically associated with impaired linear growth in children and in the development of myocardial fibrosis in some in vitro models [16, 17]. Despite the trend toward tolerating higher PTH levels, the percentage of doctors prescribing vitamin D in both oral and intravenous forms remained unchanged across eras.
This analysis noted changes in several other aspects of pediatric dialysis care over the past 20 years, including initial modality and access type. Specifically, more patients chose HD in the latest era, continuing a trend noted in a prior NAPRTCS registry report [1] and likely related in part to increased availability of HD services for children since the earlier era. Several factors other than availability are known to influence dialysis modality selection, including patient age, adherence to a prescribed home regimen, and patient/parental preference [7]. In fact, patients in the more recent cohort were more likely to change modality due to family choice, as opposed to medical complications such as excessive infection. The jugular vein remained the most common location for percutaneous HD catheters, similar to prior publications, and the use of arteriovenous (AV) grafts or AV fistulae at the time of dialysis initiation remain uncommon in children, despite guidelines emphasizing the benefits of permanent access over catheters. In children, numerous obstacles may exist to placing more definitive dialysis access, including technical difficulty given smaller blood vessels, fewer pediatric vascular-access specialists, and patient/family preference due to hopes to accomplish a renal transplant quickly. In terms of PD access, the increase in placement of swan-necked/curved, double-cuffed, downwardly oriented catheters is consonant with current recommendations that are largely based on data suggesting lower annualized peritonitis rates and longer times to first peritonitis episodes, with such access [18].
Registry data also demonstrates a difference in ESRD etiology between eras. Supplanting renal dysplasia and hypoplasia, FSGS is now the most common primary diagnosis. Recent reports indicate that the incidence of FSGS has increased over the last two decades and is especially problematic in black and Hispanic children [19]. Such children are less likely than non-Hispanic white children to be transplanted, and, as a result, they often spend longer periods on dialysis. There can also be a degree of medical-provider and parental reluctance to transplant children with FSGS given their high risk for recurrent disease, especially in children who may already have lost a renal allograft due to to recurrence. A recent registry report from European centers noted that Congenital Anomalies of the Kidney and Urinary Tract (CAKUT) were the most common cause of renal disease [20]. These discrepant findings may be due to several factors. The current registry included patients until the age of 21, compared with 14 in the European registry. Renal disease etiology was classified using different terminology: e.g, the European registry classified patients into CAKUT or glomerulonephritis groups, whereas the NAPRTCS registry allows data entry using multiple diagnoses that would fall under these more general disease categories. Finally, sampling bias may be present based on how individual centers enter data, as “Other” was the most commonly entered diagnosis in the NAPRTCS registry.
Registry data used in our report confirms an improvement in survival in children requiring chronic dialysis, which has recently been noted elsewhere [21]. In the NAPRTCS dialysis registry analysis, younger age, black race, and growth deficit were predictors of decreased survival, consistent with findings from several other registries, including USRDS [21,22,23,24,25,26]. Several studies have demonstrated an association between younger age and decreased survival [27, 28], though it is heartening that this NAPRTCS dialysis registry data shows significantly increased survival in children starting dialysis at <1 year of age between 2002 and 2011, compared with the earlier decade. Although speculative, improved dialysis equipment designed or adapted for smaller children, better surgical techniques, and improved clinical experience may have contributed to these improvements.
In prior analysis of NAPRTCS data, race influenced both the choice of modality and timing of initiation[29, 30]. Additional analysis focusing on clinical performance measures in PD patients has suggested that black patients are less likely to meet hemoglobin targets or achieve goal serum albumin levels [31, 32]. Differences have not been observed in dialysis adequacy [27, 31]. Because of its cross-sectional design, a causal relationship was not established in our analysis, but poor nutrition and heightened inflammation or differences in ESRD etiology are all possible factors influencing meeting these targets and which may account for differences in survival.
Growth deficit also negatively affected survival. A prior NAPRTCS study examining 2306 pediatric patients who initiated dialysis between 1992 and 2000 showed that poor growth in predialysis CKD was suggestive of a more complicated course following initiation [27]. Ku et al. recently analyzed data on 13,218 children in the USRDS and found that both short and tall stature increased mortality risk [28]. In prior studies, short stature in children with CKD and ESRD was associated with nonadherence to medical therapy, impaired access to care, and illness severity [33,34,35]. Growth failure in pediatric CKD is also associated with increased hospitalizations, poor school performance, and lower self-esteem [36, 37]. Although height improvement in the most recent dialysis cohort is reassuring, it remains concerning that only a small percentage of patients are on rhGH in the later cohort, a finding also observed in a prior NAPRTCS report [1]. Several barriers to the use of rhGH have been cited, including severe hyperparathyroidism, difficulty obtaining insurance approval, and noncompliance. However, rhGH is not the only option: recent studies demonstrated that aggressive nutritional management and use of biocompatible dialysate can improve growth [33, 38]. Intensified HD and hemodiafiltration protocols have also been useful [39, 40].
Since the NAPRTCS dialysis registry is a voluntary database, sampling bias is present and could influence results from our analysis. Specifically, 135 centers contributed data, eight of which were Canadian; 133 centers (including the eight Canadian) contributed to the 1992–2001 cohort and 92 (including the eight Canadian) to the 2002–2011. Therefore, there were fewer centers participating in the registry in the last decade. Reasons for this change are not certain; however, all centers enter data retrospectively, and there is no restriction on timing for data entry. Therefore, there may be some differences due to delays in data entry. In addition, centers were previously provided a stipend for data entry. To control for these effects, frailty analysis was conducted, and results of the adjusted model were similar. Moreover, demographic data did not change significantly when data only from centers that contributed to both decades were analyzed. Finally, data do not provide causation, although they do provide important associations. Specifically, given the relative rarity of pediatric ESRD, the NAPRTCS dialysis registry serves as an important source of information on children with ESRD as they transition between different treatment requirements. Given large number of pediatric centers contributing data to the registry allows a better understanding of how these children are cared for in pediatric dialysis units by pediatric providers.
In conclusion, survival of pediatric patients on chronic dialysis has improved over two decades of dialysis registry data, particularly in children <1 year. Although improvements in several clinical performance measures, such as anemia and hypertension, have been noted in data from the most recent era, poor linear growth, black race, and young age continue to be poor predictors of survival and underscore the need for ongoing improvements in care. Cardiopulmonary disease continues to be the most common causes of death, highlighting again the ongoing importance of improved blood control and management of cardiovascular risk in these patients.
References
Neu AM, Ho PL, McDonald RA, Warady BA (2003) Chronic dialysis in children and adolescents. The 2001 NAPRTCS annual report. Pediatr Nephrol 17:656–663
http://www.kidney.org/professionals/kdoqi/ Access date 4/24/2016
Levey AS (2012) A decade after the KDOQI CKD guidelines. Am J Kidney Dis 60:683–685
National High Blood Pressure Education Program Working Group On High Blood Pressure in Children and Adolescents (2004) The fourth report on the diagnosis, evaluation and treatment of high blood pressure in children and adolescents. Pediatrics 114(Suppl 4th Report):555–576
Kuczmarksi RJ, Ogler CL, Guo SS (2002) 2000 CDC growth charts for the United States: methods and development. National Center for Health Statistics. Vital Health Stat 11:246
Atkinson MA, Furth SL (2012) Anemia in children with chronic kidney disease. Nat Rev Nephrol 7:635–641
Warady BA, Neu AM, Schaefer F (2014) Optimal care of the infant, child and adolescent on dialysis: 2014 update. Am J Kidney Dis 64:128–142
Borzych-Duzalka D, Biginer Y, Ha IS, International Pediatric Peritoneal Dialysis Network (IPPN) Registry (2013) Management of anemia in children receiving chronic peritoneal dialysis. J Am Soc Nephrol 24:665–676
Amaral S, Hwang W, Fivush B, Neu A, Frankenfield D, Furth S (2006) Association of mortality and hospitalization with achievement of adult hemoglobin targets in adolescents maintained on hemodialysis. J Am Soc Nephrol 17:2878–2885
Dahlinghaus EK, Neu AM, Atkinson MA, Fadrowski JJ (2014) Hemoglobin level and risk of hospitalization and mortality in children on peritoneal dialysis. Pediatr Nephrol 29:2387–2394
Palmer SC, Saglimbene V, Mavridis D, Slanti G, Craig JC, Tonelli M, Wiebe N, Strippoli GF (2014) Erythropoiesis-stimulating agents for anaemia in adults with chronic kidney disease: a network meta-analysis. Cochrane Database Syst Rev 12:CD010590
Chavers BM, Solid CA, Daniels FX, Chen S-U, Frankenfield DL, Herzog CA (2009) Hypertension in pediatric long-tern hemodialysis patients in the United States. Clin J Am Soc Nephrol 8:1363–1369
Shroff R, Weaver DJ Jr, Mitsnefes MM (2011) Cardiovascular complications in children with chronic kidney disease. Nat Rev Nephrol 13:642–649
Haffner D, Schaefer F (2013) Searching the optimal PTH target range in children undergoing peritoneal dialysis: new insights from international cohort studies. Pediatr Nephrol 28:537–545
Borzych D, Rees L, Ha IS (2010) The bone and mineral disorder of children undergoing chronic peritoneal dialysis. Kidney Int 78:1295–1304
Jung S, Querfeld U, Muller D, Rudolph B, Peters H, Kramer S (2012) Submaximal suppression of parathyroid hormone ameliorate calcitriol-induced aortic calcification and remodeling and myocardial fibrosis in uremic rats. J Hypertens 30:2182–2191
Bacchetta J, Harambat J, Cochat P, Salusky IB, Wesseling-Perry K (2012) The consequences of chronic kidney disease on bone metabolism and growth in children. Nephrol Dial Transplant 27:3063–3071
Warady BA, Bakkaloglu S, Newland J, Cantwell M, Verrina E, Neu A, Chadha V, Yap H-K, Schaefer F (2012) Consensus guidelines for the prevention and treatment of catheter-related infections and peritonitis in pediatric patients receiving peritoneal dialysis: 2012 update. Perit Dial Int 32:S32–S86
Kim JS, Bellew CA, Silverstein DM, Aviles DH, Boineau FS, Vehashkari VM (2005) High incidence of initial and late steroid resistance in childhood nephrotic syndrome. Kidney Int 68:1275–1282
Chesnaye C, Bonthuis M, Schafer F, Groothoff JW, Verrin E, Heaf JG, Jankauskiene A, Lukosiene V, Molchanova EA, Mota C, Peco-Antic A, Ratsch I-M, Bjerre A, Roussinov DL, Sukalo A, Topaloglu R, Hoeck KV, Zagozdzon I, Jager KJ, Stralen KJV, on behalf of the ESPN/ERA-EDTA registry (2014) Demographics of paediatric renal replacement therapy in Europe: a report of the ESPN/ERA-EDTA registry. Pediatr Nephrol 29:2403–2410
Mitsnefes MM, Laskin BL, Dahhou M, Zhang X, Foster BJ (2013) Mortality risk among children initially treated with dialysis for end-stage kidney disease, 1990-2010. JAMA 309:1921–1929
Samuel SM, Tonelli MA, Foster BJ, Alexander RT, Nettel-Aguirre A, Soo A, Hemmelgam BR, Pediatric Renal Outcomes Canada Group (2011) Survival in pediatric dialysis and transplant patients. Clin J Am Soc Nephrol 6:1094–1099
McDonald SP, Craig JC, Australian and New Zealand Paediatric Nephrology Association (2004) Long-term survival of children with end-stage renal disease. N Engl J Med 350:2654–2662
Groothof JW, Gruppen MP, Offringa M (2002) Mortality and causes of death of end-stage renal disease in children: a Dutch cohort study. Kidney Int 61:621–629
Alexander RT, Foster BJ, Tonelli MA, Soo A, Nettel-Aguirre A, Hemmelgarn BR, Samuel SM, Pediatric Renal Outcomes Group Canada (2012) Survival and transplantation outcomes of children less than 2 years of age with end-stage renal disease. Pediatr Nephrol 27:1975–1983
Wedekin M, Ehrich JH, Offner G, Pape L (2010) Renal replacement therapy in infants with chronic renal failure in the first year of life. Clin J Am Soc Nephrol 5:18–32
Furth SL, Stablein D, Fine RN, Powe NR, Fivush BA (2002) Adverse clinical outcomes associated with short stature at dialysis initiation: a report of the north American Pediatric renal transplant cooperative study. Pediatrics 109:909–913
Ku E, Fine RN, Hsu C-Y, McCulloch C, Glidden DV, Grimes B, Johansen KL (2016) Height at first RRT and mortality in children. Clin J Am Soc Nephrol 11:832–839
Seikaly MG, Slhab N, Browne R (2005) Patterns and time of initiation of dialysis in US children. Pediatr Nephrol 20:982–988
Minnick ML, Boynton S, Ndirangu J, Furth S (2010) Sex, race, and socioeconomic disparities in kidney disease in children. Semin Nephrol 30:26–32
Atkinson MA, Am N, Fivush BA, Frankenfield DL (2007) Ethnic disparity in outcomes for pediatric peritoneal dialysis patients in the ESRD clinical performance measures project. Pediatr Nephrol 22:1939–1946
Atkinson MA, Neu AM, Fivush BA, Frankenfield DL (2008) Disparate outcomes in pediatric peritoneal dialysis patient by gender/race in the end-stage renal disease clinical performance measures project. Pediatr Nephrol 23:1331–1338
Parekh RS, Flynn JT, Smoyer WE (2001) Impaired growth in young children with severe chronic renal insufficiency who use specified nutritional therapy. J Am Soc Nephrol 12:2418–2426
Fine RN, Martz K, Stablein D (2010) What have 20 years of data from the North America Pediatric renal transplant cooperative study taught us about growth following renal transplantation in infants, children, and adolescents with end-stage renal disease? Pediatr Nephrol 25:739–746
Harambat J, Bonthuis M, van Stralen KJ, ESPN/ERA-EDTA Registry (2014) Adult height in patients with advanced CKD requiring renal replacement therapy during childhood. Clin J Am Soc Nephrol 9:92–99
Sander A, Borzych-Duzalka D (2012) Comorbidities in chronic pediatric peritoneal dialysis patients: a report of the international Pediatric peritoneal dialysis network. Perit Dial Int 32:410–418
Al-Uzri A, Matheson M, Gipson DS, Mendley SR, Hooper SR, Yadlin O, Rozansky DJ, Moxey-Mims M, Furth SL, Warady BA, Gerson AC, Chronic Kidney Disease in Children Study Group (2013) The impact of short stature on health-related quality of life in children with chronic kidney disease. J Pediatr 163:736–741
Rees L, Azocar M, Borzych D, Watson AR, Buscher A, Edefonti A, Bilge I, Askenazi D, Leozappa G, Gonzales C, van Hoeck K, Secker D, Zurowska A, Ronnholm K, Bouts AHM, Stewart H, Ariceta G, Ranchin B, Warady BA, Schaefer F, International Pediatric Peritoneal Dialysis Network (IPPN) registry (2011) Growth in very young children undergoing chronic peritoneal dialysis. J Am Soc Nephrol 22:2303–2312
Fishbach M, Terzic J, Menouer S, Dheu C, Seuge L, Zalosczic A (2010) Daily online haemodiafiltration promotes catch-up growth in children on chronic dialysis. Nephrol Dial Transplant 25:867–873
Muller D, Zimmering M, Chan CT, McFarlane PA, Pierratos A, Querfeld U (2008) Intensified hemodialysis regimens: neglected treatment options for children and adolescents. Pediatr Nephrol 23:1729–1736
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Local institutional review board approval was obtained at each center for data entry.
Conflict of interest
None of the authors have a conflict of interest to resolve related to the current manuscript.
Rights and permissions
About this article
Cite this article
Weaver, D.J., Somers, M.J.G., Martz, K. et al. Clinical outcomes and survival in pediatric patients initiating chronic dialysis: a report of the NAPRTCS registry. Pediatr Nephrol 32, 2319–2330 (2017). https://doi.org/10.1007/s00467-017-3759-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-017-3759-4