Abstract
Background
The etiology of idiopathic nephrotic syndrome (INS) remains partially unknown. Viral infections have been reported to be associated with INS onset and relapse. The aim of this study was to describe the epidemiology of a population-based cohort of children with INS and propose a spatiotemporal analysis.
Methods
All children aged 6 months to 15 years with INS onset between December 2007 and May 2010 and living in the Paris area were included in a prospective multicenter study. Demographic and clinical features at diagnosis and 2 years were collected.
Results
INS was diagnosed in 188 children, 93 % of whom were steroid sensitive. Annual incidence was 3.35/100,000 children. Standardized incidence ratio (SIR) was higher in one of the eight counties: Seine-Saint-Denis, with SIR 1.43 [95 % confidence interval (CI) 1.02–1.95]. A spatial cluster was further identified with higher SIR 1.36 (95 % CI 1.09–1.67). Temporal analysis within this overincidence area showed seasonal variation, with a peak during the winter period (p <0.01). In addition, partition of the Paris area into quintiles of the population showed that the average delay of occurrence, with regard to the first study case, followed a longitudinal progression (p <0.0001).
Conclusion
The clustering of cases, the seasonal variation within this particular area, and the progression over the Paris area altogether suggest that INS may occur on an epidemic mode.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic nephrotic syndrome (INS) is the most common acquired glomerulopathy in children. It has been described worldwide but remains a rare condition. Population-based epidemiological data are scarce, and the etiologic mechanisms of the disease remain largely unknown. INS is likely a primary immune disorder, and viral infections—especially upper respiratory tract infections—have been reported as a trigger of first manifestation and relapses [1]. Some authors have also reported a seasonal periodicity in the occurrence of both onset and relapses [2, 3]. Furthermore, only four prospective epidemiological studies have been reported: a French region-wide study (1985–1992) (Bouissou et al., ESPN 1993), and three nationwide studies from Australia (1998–2000) [4], New Zealand (2001–2004), and The Netherlands (2003–2006), showing an annual incidence between 1.15 and 2.10 cases per 100,000 children [5, 6]. In addition, other retrospective studies show variations in INS incidence regarding ethnicity [7–9], urban versus rural areas [10], and socioeconomic level [11].
The aim of this work was initially to study the annual incidence in a prospective, population-based cohort of children with newly diagnosed INS over a 30-month period in a limited geographical area: the Paris area. Spatial and temporal clustering of the first cases suggested a link between cases and led us to complete the analysis with recent tools of dynamic epidemiology and geographical information systems applied to health issues. Consequently, this study looked for the temporospatial epidemiology of the disease and aimed at describing the timing and direction of spread of the cases, as well as the geographic pattern of the disease. A better understanding of the underlying mechanisms of INS may result from this novel and complementary approach.
Material and methods
Definitions
INS was defined by proteinuria >0.25 g/mmol (2 g/g) of urinary creatinine, hypoalbuminemia <30 g/L (3 g/dl) (all patients had a serum albumin <25 g/l at presentation), negative hepatitis serology, and normal C3 value. Treatment protocol of the first flare, as well as definitions of steroid dependency and resistance, are those of the French Société de Néphrologie Pédiatrique [12, 13]. Steroid dependency is defined by the occurrence of a relapse during steroid therapy or within 2 weeks of steroid withdrawal. Steroid resistance is defined by the absence of remission after 4 weeks of prednisone taken orally at 60 mg/m2 and three methylprednisolone pulses at 1 g/1.73 m2.
Study design
Our study was population based and assessed all children between 6 months and 15 years (i.e. <16 years) and living in one of the eight counties of the Paris area and presenting with a first episode of INS between 3rd December 2007 and 1st June 2010. The study population was based on a prospective multicentric case–control study titled NEPHROVIR [14]. In the Paris area, medical organization is such that newly diagnosed children are systematically referred to a hospital pediatric unit. Consequently, all 39 pediatric units in the Paris area managing patients with acute NS participated and comprised the 3 specialized pediatric nephrology units and the 36 general pediatric units in the Ile-de-France area. In order to reach exhaustiveness, we looked for possible unregistered cases by personal phone calls, email contacts, and site visits to all the pediatric units in the area. The study was reviewed and accepted by the local ethic committee. Written informed consent was systematically signed by parents and, when possible, the patient (age >10 years).
Statistical analysis and mapping
Patients’ addresses were geocoded with a geographic positioning system (GPS) and used to study spatial distribution of cases. The incidence of INS was calculated by relating the number of patients newly diagnosed with INS to the number of children up to 15 years who were alive during the 30 months of registration in the whole Paris area, in the eight counties separately, and in each municipality. The population numbers were extracted from the official statistical data from the National Institute for Statistics and Economic Studies (INSEE). These data can be found on the website and are freely available. Because of heterogeneity in population density and structure in the area, we also used indirect standardization with sex- and age-controlled standardized incidence ratio (SIR) [15]. SIR in an area is the ratio between observed and expected numbers of cases in this area. Expected number is calculated by multiplying each age- and sex-specific incidence rate of the reference population (whole Paris area) by each age- and sex-specific population and then totalling the results. A standardized risk ratio (SRR) was defined for the whole study period as the ratio between SIRs in two different areas in order to measure the increased risk and observe a case in a given area compared with other areas combined [16]. Time-varying SRRs were defined as the ratio between the SIR in a given period and area and the SIR outside this period and/or area. For all counties of the Paris area, standardized incidences were compared with the use of the Wald tests applied to the SRR. Variation of the SIR inside versus outside the overincidence area over time was studied using a 4-month running average.
Characteristics of patients inside and outside the overincidence area were described: quantitative covariates as number and percentage of available data, and categorical covariates as median and interquartile range (IQR). Distributions inside versus outside the area were compared with Mann–Whitney and Wilcoxon tests for quantitative covariates and Fisher exact tests for categorical covariates.
The temporospatial pattern was studied, and the area was divided into quintiles according to patients’ longitudinal and latitudinal coordinates. Each quintile represents a set of 20 % of cases. The median delay of occurrence, according to the first case (that was located in quintile 4 of longitude), was computed in each quintile, and we conducted a linear regression analysis to estimate the association between delay of occurrence and quintile of patients.
The nearest neighbor hierarchical clustering (Nnh) is a method of spatial analysis that compares the distance between each incident case and then groups them with a minimum distance threshold criterion [17]. If an incident case is close enough to one or more others, a first-order cluster is detected. When all incident cases have been scanned, the same algorithm tries to detect second-order clusters. For this, a minimum of three points by group was set. In addition, because the population density is heterogeneous, a risk-adjusted Nnh [18] was preferred. The distance threshold is thus not a fixed distance but an adjusted distance according to population distribution (Student’s t test with a distance probability between pairs). Results are mapped as standard deviational (SD) ellipse [19], which approximates hot-spot localization with significant aggregation of cases. A Monte Carlo test was used to confirm that the distribution of clusters was not random.
Kernel-density mapping is another method of spatial analysis based on a point interpolation technique [20–22]. It applies, over the whole study area, a distance function inside a moving a circle, in this study with a 5-km radius. A density is calculated each time the window encounters one or several points. This value is weighted by a distance function inside the window and the point position on the study area. Results can be interpreted as a continuous density of population. A ratio of patient density and density of the child population was also calculated as a dual-kernel density in order to take the child population size into account.
All statistical analyses were performed with the R statistical program (v3.1.1). For all statistical tests, a p value <0.05 was considered to be significant. All maps were created with Arcmap 10.2 and Crimestat 3.3.
Results
Patient population
One hundred and eighty-eight children were newly diagnosed with INS between December 2007 and May 2010 in the study area. One hundred and sixty-five with a virological analysis were included from the NEPHROVIR study, including genoprevalence of Epstein-Barr virus (EBV) and other herpesviruses in INS patients at diagnosis [14]. Twenty-three additional patients were registered in a second recall. Reasons for noninclusion in the NEPHROVIR cohort were parents refusing the extra blood sample for the study (N = 3), language or social problems (N = 3), child’s vacation outside the Paris area at onset (N = 3), or any other reason not due to the patient (N = 14).
Demographic and clinical features are shown in Table 1. Briefly, median age at onset was 4.1 (mean 5.4) years, and 90 % of children were aged <10 years; male-to-female ratio was 1.8 over the whole population; 43 % of patients reported an infectious episode in the preceding month; steroid responsiveness was observed in 93 % of patients, including ten treated with methylprednisolone IV and whose median time to response was 8.5 (IQR 7–11) days; steroid dependency was observed in 48 % of the total series (52 % of steroid-sensitive patients).
All 14 steroid-resistant patients (histology showed focal and segmental glomerular sclerosis in 5 cases, minimal changes in 8, and was not determined in 1) were included in the analysis. Thirteen were sensitive to the association of prednisone/cyclosporine. The last steroid-resistant patient developed end-stage renal disease (ESRD) after 8 months of treatment and had an early recurrence on graft, confirming the diagnosis of INS.
Incidence of INS
The annual incidence of INS in the Paris area was 3.35 per 100,000 children aged between 6 months and 15 years. Monthly incidence ranged from two to 13 new cases a month (Fig. 1). Ten or more new cases occurred during 4 months of the observation period: December 2007, April 2008, December 2008, and March 2009. It is also noteworthy that eight new cases were registered in December 2009.
The Paris area is divided into eight administrative counties (Fig. 2), each county encompassing dozens of townships. Spatial analysis found disparities in incidence rates within those counties. In order to account for the demographic disparities within counties, SIRs in each county were assessed, showing a significantly higher incidence in the county of Seine-Saint-Denis (county 93) compared with the other areas [SIR 1.43, 95 % confidence interval (CI) 1.02–1.95; SRR 1.55, 95 % CI 1.09–2.19] (Table 2).
An area of overincidence was designed according to the results of a risk-adjusted Nnh clustering calculation (Fig. 3), as well as kernel-density mapping (Fig. 4). Figure 3 shows that seven first-order clusters were detected and one cluster of the second order. First-order clusters were strikingly all located close to a river. Figure 4a shows the density of the general child population and Fig. 4b the density of patients. It appears that distribution of children does not exactly overlap with patients: more patients live in the northeast and northwest of Paris city. A ratio of the two densities has been calculated as a dual-kernel density, confirming the difference in patient and child population distribution. This spatial cluster, designed regardless of administrative boundaries, appeared centered on the county of Seine-Saint-Denis, with limited extensions into neighboring counties. In order to further analyze incidences in and outside the area of clusters, we computed INS cases township by township, identifying an area of contiguous townships that finally displayed a very high incidence of cases (Fig. 3). This area of 467 km2 (the total surface of Paris area is 12,011 km2) included 89 of the 188 patients and displayed an annual incidence of 4.61 per 100,000 children (95 % CI 3.71–5.68) versus 2.66 (95 % CI 2.16–3.24) in the rest of the Paris area outside the cluster. SIR in the special area was 1.36 (95 % CI 1.09–.67), while SIR was at 0.81 in the rest of the Paris area (95 % CI 0.66–0.98). SRR over the study period in this area was 1.68 (95 % CI 1.26–2.24). General features of patients living in and outside the special area of higher incidence showed no differences in clinical outcome and viral status (Table 1). Conversely, the special area was characterized by a lesser proportion of patients from Caucasian extraction and a balanced sex ratio compared with the rest of the Paris area.
Cluster of cases: A risk-adjusted nearest-neighbor hierarchical (Nnh) clustering shows seven clusters of first order. A second-order clustering comprises four clusters in north of Paris, overlapping with the area of overincidence. Of note, all clusters of first order are in close vicinity to a river
Kernel-density mapping of children in the general population and patients, with a radius of 5 km2: a Population density aged 0–15 years in the Paris area. b Case density of idiopathic nephrotic syndrome (INS) in the Paris area. This representation of densities, regardless of administrative boundaries, shows that distributions of children and patients do not exactly overlap, with patients more frequently located in the northeast and northwest of Paris city
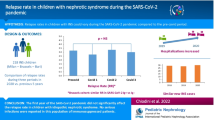
In addition, a temporal analysis was performed, which showed a circannual variation in SRR in this special area, with winter peaks (Fig. 5). Figure 5a shows that in the special area, SRR 95 % CI has its lower limit >1 in winter periods, whereas Fig. 5b, outside the special area, shows no significant variation in SRR over time.
Seasonal variation of sex- and age-controlled standardized risk ratio (SRR): a inside and b outside the overincidence area. The time-varying SRR inside the overincidence area (a) is expectedly higher than outside this area (b): SRR = 1.68 [95 % confidence interval (CI) 1.26–2.24] over the study period inside the area
Secondarily, we looked at a temporospatial pattern in the whole Paris area. Five centers of recruitment registered new cases in a very limited period of time (Fig. 6): Center 1 registered six patients in 12 weeks from December 2007 to March 2008 and a seventh in April 2010; center 2 registered four patients in 3 weeks from the 29 September to 22 October 2009, one patient in July 2008, one in March 2009, and one in April 2010; center 3 registered four patients in 3 months from the 22 December 2008 to 24 April 2009 and one in May 2010; center 4 registered three patients during the 30-month period between 9 March and 2 June 2009.
Longitudinal location of new cases over time supported a longitudinal progression of case occurrence. Each patient is located with its longitudinal positioning over the Paris area. Each quintile represents the longitudinal amplitude of 20 % of cases (Fig. 7). The median delay of case occurrence in each quintile, since the first case, which was located in Q4, progressively increased from Q4 to Q1 toward the west and from Q4 to Q5 toward the east, with a linear regression (p <0.0001) (Fig. 8). When keeping only quintiles 1–4, the linear correlation coefficient was 76, meaning that the mean delay when progressing from quintile to quintile from the east to the west increased by 76 days between Q4 and Q1. It is noteworthy that the first patient observed in Q1 was registered 28 days after the first patient in Q4 and the second patient in Q1 being further registered 143 days later. No other such gaps were observed in the other quintiles during the period of observation.
Map of the Paris area and patient localization: Each patient (N = 188) is represented by a spot according to postal address. Dotted lines represent limits of longitudinal case distribution into quintiles, from quintile 1 in the west toward quintile 5 in the east. Each quintile represents a set of 20 % of cases
Median delay of onset since the first case in quintile 4: Patients were divided into quintiles according to a longitudinal axis of geolocation, from west (Q1) to east (Q5). First case occurred in Q4. The median delay of cases in quintiles, according to the date of the first case, increasing from Q4 in the west toward Q1 (***p < 0.001) and to the east toward Q5 (*p < 0.05)
In addition, no other special progression was observed according to a north–south axis, to a given axis defined as a combination of the cardinal directions, or to a centrifuge model (location of new cases occurring further from a hypothetical center).
Discussion
To our knowledge, this is the first study providing data integrating time and space in an epidemiological analysis of INS. Here, we report a prospective population study, in a limited urban area, with a high density of general population, showing that INS may take the form of an epidemic disease.
INS is a rare condition. Epidemiological data are scarce and mostly based on retrospective and center- or region-based studies. Among the prospective studies, only those from The Netherlands provide spatial analysis, showing no significant difference in case distribution within the different provinces [6]. The annual incidence in the Paris area is higher than those previously published in the prospective studies. The high population density (991/km2) in the Paris area with 11.9 million inhabitants, including 2.3 million children aged up to 15 years, might influence the incidence. Interestingly, a study from Taiwan [23], where population density was 640/km2, showed an incidence of 3.36 new cases/year per 100,000 children aged 0–18 years—very similar to those of the Paris area at the same period. This is compared with The Netherlands, with a population density of 405/km2 and a lower incidence (1.52 new cases/year per 100,000 children aged 0–18 years).
Because one quarter of cases registered during the first month of this prospective survey were located in just one of the 39 centers involved in the study, we made the hypothesis that the disease may behave as an epidemic. The terms epidemic and endemic were first used by Hippocrates to distinguish diseases that were always present in a given area from those that only occurred during limited periods of time [24]. The term epidemic has been predominantly used to describe acute infectious diseases, but it also refers to any disease displaying an outbreak with a disproportionate number of cases at a given time in a given area. Endemic refers to a disease that is present in a population or a geographic region at a consistent level and period of time [25]. In addition, an epidemic course supposes a link in space and time between cases.
To test this hypothesis, the first step was to study the temporospatial pattern according to the distribution of cases along the standard geographical parameters of longitude and latitude. The five defined geographical areas encompassed a similar number of patients. This method revealed a correlation between the spread of cases through longitudinal quintiles of population within the time of observation. Our results suggest that a triggering event might have occurred first in quintile 4 and was responsible for the cluster observed by center 1, which progressed to the three quintiles to the west and to the final quintile to the east. It is noteworthy that because of the length of study preparation from grant acceptance, the onset of the survey coincided with the onset of winter, which is annually marked by the onset of viral outbreaks. Interestingly, the first manifestation of INS usually occurs in early childhood, which matches with the age of primary viral infections and the link between unspecific upper respiratory tract infections, and the first manifestation is ancient knowledge [1, 26]. Observing this temporospatial pattern raised questions about other environmental factors that may explain a longitudinal spread and that may also be involved in disease occurrence. Interestingly, dominant winds go from west to east due to the proximity to the Atlantic Ocean, while the main rivers (Seine and Marne) cross the region from east to west. Of note, the catchment area of those rivers is a wide area of intensive agricultural activity associated with the use of herbicides and pesticides [27]. Herbicides could also explain the seasonal variation, and they have been reported to contribute to targeting the immune system [28]. Atmospheric chemicals might also be an issue [29], whereas the emission of polycyclic aromatic hydrocarbons produced by domestic heating, car traffic, and industries are more significant in the winter period.
The next approach was to study the spatial clustering according to geographical positioning of patients. Because administrative boundaries create artificial, irregular, and heterogeneous structuring in space, we used a mapping approach with Nnh clustering. Interestingly, all seven hierarchical clusters of the first order were located in peripheral urban concentrations close to the rivers. In addition, the method allowed definition of a second-order cluster located between the River Seine and the River Marne. By contrast, other peripheral urban concentrations not located on those main rivers are not in clusters.
Kernel density is an additional method my which to study case density regardless of administrative boundaries. Consistently, the area with a significantly higher kernel density matches with the second-order cluster. According to these results, we designated an area with administrative boundaries in order to identify cases in the cluster. This was needed to study the incidence according to general population data as well as to locate the possible environmental factors involved in the concentration of cases. This designation was validated, as the incidence inside the area was effectively almost twice the incidence outside the area.
This overincidence area represents a population with a low socioeconomic level and mixed ethnic background. NS has previously been reported up to seven times more common among Asian than Caucasian children in the UK, with an incidence of 16 new cases per 100,000 children a year [8]. Ethnicity background and its wide heterogeneity in the Paris area may be a confounding factor. In France, no data are available regarding ethnicity in the general population, so we were unable to study INS incidence rate according to ethnicity or to compare ethnicities inside versus outside the area of higher incidence. Concerning the influence of socioeconomic level on INS incidence, in 1968, Schlesinger demonstrated a higher incidence of INS in the lowest socioeconomic level group compared with the middle or highest socioeconomic level [11]. In addition, after a similar analysis for other diseases—for example, cystic fibrosis, a genetic disease; and infectious encephalitis—it appeared that the distribution of INS according to socioeconomic level approximated more closely to a dominant infectious disease rather than a genetic disease. Seasonal variation with a winter peak within the overincidence area argues the hypothesis of an infectious or transmissible agent as a trigger of the disease.
Clearly, this study was not primarily designed to find specific environmental factors, which remain to be identified. The study provides a new approach to analyze the epidemiology of INS. However, both kernel-density mapping and Nnh clustering only identify spatial clusters and did not include time in the analysis. This leads to a focus on permanent environmental expositions within the identified areas. Other tools of space–time analysis, like emerging hot-spot analysis based on Mann—Kendall trend test and the Getis–Ord Gi, would be more relevant but require greater statistical power.
In conclusion, in this study, where demographic considerations enabled a high density of cases, we demonstrate that INS may have an epidemic course with a spatial synchrony and geographical clustering, suggesting that environmental factors play a central role in the physiopathology of the disease.
References
Yap HK, Han EJ, Heng CK, Gong WK (2001) Risk factors for steroid dependency in children with idiopathic nephrotic syndrome. Pediatr Nephrol 16:1049–1052
Toyabe S, Nakamizo M, Uchiyama M, Akazawa K (2005) Circannual variation in the onset and relapse of steroid-sensitive nephrotic syndrome. Pediatr Nephrol 20:470–473
Odaka J, Kanai T, Uehara R, Kusano E, Yamagata T (2015) Seasonal variation in first episode of childhood idiopathic steroid-sensitive nephrotic syndrome and adult minimal change nephrotic syndrome. Clin Exp Nephrol 19:146–147
Hodson E, Craig J, Willis N (2002) Congenital and idiopathic nephrotic syndrome. In: Ninth Annual Report Australian Paediatric Surveillance Unit. Eliott E, Australia, pp 6–8
Wong W (2007) Idiopathic nephrotic syndrome in New Zealand children, demographic, clinical features, initial management and outcome after twelve-month follow-up: results of a three-year national surveillance study. J Paediatr Child Health 43:337–341
El Bakkali L, Rodrigues Pereira R, Kuik DJ, Ket JC, van Wijk JA (2011) Nephrotic syndrome in The Netherlands: a population-based cohort study and a review of the literature. Pediatr Nephrol 26:1241–1246
Chuan PL, Leng SC, Sinniah R (1975) Five-year review of nephrotic syndrome in Singapore children. J Singapore Paediatr Soc 17:113–123
Sharples PM, Poulton J, White RH (1985) Steroid responsive nephrotic syndrome is more common in Asians. Arch Dis Child 60:1014–1017
McKinney PA, Feltbower RG, Brocklebank JT, Fitzpatrick MM (2001) Time trends and ethnic patterns of childhood nephrotic syndrome in Yorkshire, UK. Pediatr Nephrol 16:1040–1044
Feehally J, Kendell NP, Swift PG, Walls J (1985) High incidence of minimal change nephrotic syndrome in Asians. Arch Dis Child 60:1018–1020
Schlesinger ER, Sultz HA, Mosher WE, Feldman JG (1968) The nephrotic syndrome. its incidence and implications for the community. Am J Dis Child 116:623–632
French National Authority for Health (2008) Idiopathic nephrotic syndrome in children. French National Authority for Health: 1–22
Azib S, Macher MA, Kwon T, Dechartres A, Alberti C, Loirat C, Deschênes G, Baudouin V (2011) Cyclophosphamide in steroid-dependent nephrotic syndrome. Pediatr Nephrol 26:927–932
Dossier C, Sellier-Leclerc A-L, Rousseau A, Michel Y, Gautheret-Dejean A, Englender M, Madhi F, Charbit M, Ulinski T, Simon T, Jacqz-Aigrain E, Deschênes G (2014) Prevalence of herpesviruses at onset of idiopathic nephrotic syndrome. Pediatr Nephrol 29:2325–2331
Tripepi G, Jager KJ, Dekker FW, Zoccali C (2010) Stratification for confounding--part 2: direct and indirect standardization. Nephron Clin Pract 116:c322–c325
Breslow N, Day N (1993) Statistical methods in cancer research: the design and analysis of cohort studies. Int Agency Res Cancer: 406
Johnson SC (1967) Hierarchical clustering schemes. Psychometrika 32:241–254
Levine N (2013) CrimeStat IV: A spatial statistics program for the analysis of crime incident locations (version 4.0). Houston, TX, and the National Institute of Justice, Washington DC
Mitchell A (2005) The ESRI guide to GIS analysis. VOlume 2 : spatial measurements and statistics
Bithell JF (1990) An application of density estimation to geographical epidemiology. Stat Med 9:691–701
De Smith M, Goodchild M, Longley P (2007) Geospatial analysis : a comprehensive guide to principles, techniques and software tools. Troubadour Publishing Ltd
Larmarange J, Vallo R, Yaro S, Msellati P, Méda N (2011) Methods for mapping regional trends of HIV prevalence from demographic and health surveys (DHS). Cybergeo : Europ J Geography 2011:558
Chang J-W, Tsai H-L, Yang L-Y, Chen T-J (2012) Epidemiology and predictors of end-stage renal disease in Taiwanese children with idiopathic nephrotic syndrome. J Epidemiol 22:517–522
Swaroop S (1957) Index of endemicity. Bull World Health Organ 16:1083–1101
Kalra S, Kumar A, Jarhyan P, Unnikrishnan AG (2015) Endemic or epidemic? measuring the endemicity index of diabetes. Indian J Endocrinol Metab 19:5–7
MacDonald NE, Wolfish N, McLaine P, Phipps P, Rossier E (1986) Role of respiratory viruses in exacerbations of primary nephrotic syndrome. J Pediatr 108:378–382
Blanchoud H, Farrugia F, Mouchel JM (2004) Pesticide uses and transfers in urbanised catchments. Chemosphere 55:905–913
Colosio C, Corsini E, Barcellini W, Maroni M (1999) Immune parameters in biological monitoring of pesticide exposure: current knowledge and perspectives. Toxicol Lett 108:285–295
Vidotto JP, Pereira LA, Braga AL, Silva CA, Sallum AM, Campos LM, Martins LC, Farhat SC (2012) Atmospheric pollution: influence on hospital admissions in paediatric rheumatic diseases. Lupus 21:526–533
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Ethical statement
The study was reviewed and accepted by the local ethic committee. A written informed consent was systematically signed by the parents and, when possible, by the patient (age >10 years).
Rights and permissions
About this article
Cite this article
Dossier, C., Lapidus, N., Bayer, F. et al. Epidemiology of idiopathic nephrotic syndrome in children: endemic or epidemic?. Pediatr Nephrol 31, 2299–2308 (2016). https://doi.org/10.1007/s00467-016-3509-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-016-3509-z