Abstract
Background
Intradialytic hypotension and myocardial stunning are proposed as contributing to the pathogenesis of increased cardiovascular disease burden and death in patients receiving maintenance hemodialysis (HD). Noninvasive cardiac output measurements provide a dynamic, real-time assessment of hemodynamic parameters. We investigated intradialytic changes in hemodynamic parameters in pediatric outpatients receiving chronic HD and determined patient and treatment risk factors associated with such intradialytic changes.
Methods
Hemodialysis was performed using linear fluid removal over 4 h with polysulfone dialyzers. Continuous wave Doppler ultrasound was used to measure hemodynamic parameters prior, 2 h into, and after the mid-week HD treatment session. Pulse wave tonometry was performed at the same time. The percentage change in blood volume was measured by noninvasive hematocrit monitoring during HD.
Results
Twenty-two patients fit the inclusion criteria, of whom 16 (73 %) were male. The mean age of the patients was 17 ± 3.8 years, and the dialysis vintage was 47.8 ± 33.7 months. The cardiac index decreased significantly midway through the HD treatment session and remained low until the end of treatment. A significant decline in cardiac index without hypotension occurred in 12 (54 %) patients. Expected increase in systemic vascular resistance index to preserve the cardiac index was not observed. Weight, percentage fluid overload, dialysis vintage, and adequacy did not correlate with the observed decline in the cardiac index. The decrease in blood volume at the 2 h (R = 0.43, p = 0.045) and 4 h (R = 0.56, p = 0.007) time points was the only factor associated with cardiac index decline.
Conclusion
The cardiac index and stroke volume decreased significantly during the HD session. Patients with larger blood volume changes during the first 2 h of HD and at 4 h showed a significant decrease in cardiac index that did not recover at the completion of the HD treatment. Rate of fluid removal was the only significant risk factor for compromised cardiac index during HD. Conventional methods currently used for assisting fluid removal in HD are inadequate to assess hemodynamic changes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Young adults receiving maintenance dialysis exhibit 40- to 50-fold higher mortality rates than an age-matched general population, with cardiovascular (CV) disease being the most common cause of mortality [1]. This high CV disease-associated mortality is also seen in children receiving dialysis who have CV mortality rates that are almost 1000-fold higher than their age-matched healthy peers [2, 3]. Traditional risk factors seen in adult populations, such as dyslipidemia, smoking, and age-related atherosclerosis, do not account for the high prevalence of left ventricular disease in pediatric patients with end-stage renal disease (ESRD) [4]. Emerging data strongly support a role of interdialytic fluid overload and the subsequent intra-dialytic cardiac stress associated with removal of this fluid in the development of CV disease in this population [5, 6].
Myocardial stunning occurs when a non-lethal reduction in coronary arterial blood supply leads to the depression of myocardial function for a length of time ranging from hours to days [7, 8]. Traditional intermittent hemodialysis (HD) performed three times each week requires fluid removal over a period of only 3–4 h. Such rapid changes in circulating blood volume during HD have long been suspected of contributing to left ventricular dysfunction [9–11]. Burton et al. recently showed that myocardial stunning, defined as a reduction in regional wall motion in two or more segments from baseline and hyperkinesis in global parameters of cardiac contractility, occurs in up to two-thirds of adult patients during HD [12]. However, this phenomenon is less well studied in pediatric patients. Reliance on symptomatology only to guide safe rate of fluid removal might lead to missed subtle changes in the cardiac index with resultant subclinical myocardial stunning.
Noninvasive cardiac output measurements, validated in critically ill children, provide a dynamic, real-time assessment of hemodynamic parameters [13, 14]. The aim of this study was to investigate intradialytic changes in hemodynamic parameters in pediatric outpatients receiving chronic HD using a chair-side portable hemodynamic monitoring tool. We also sought to determine patient and treatment risk factors associated with such intradialytic changes.
Materials and methods
Patient selection
All patients who received chronic HD for more than 3 consecutive months at Texas Children’s Hospital (Houston, TX) were eligible for inclusion in this study. Patients who had not received HD for more than 3 consecutive months or who did not cooperate with having their hemodynamic parameters obtained were excluded.
Study protocol
Ultrasound (US) cardiac output monitors measure blood flow across the heart valves, either the aortic or pulmonary valve, using continuous wave Doppler US technology (Uscom Ltd., Sydney, Australia). The software uses algorithms based on the patient’s weight and height to determine the area of the valve. Stroke volume measurements are used in the formulas to calculate a beat-to-beat measurement of cardiac output and derive other parameters, such as systemic vascular resistance. US-based cardiac output measurements have been used to guide treatment in patients with shock by rapidly supplying information on the cardiac index, defined as the volume of blood ejected by the heart in 1 min indexed to the body surface area, stroke volume, and systemic vascular resistance, or the resistance to blood flow by the systemic vasculature, among other measured and derived parameters. This tool consists of a screen and a probe, about the size of a pen, which is placed in the suprasternal notch. It is portable, easy to use, and easy for the operator to become proficient.
HD was performed using linear fluid removal on a standard dialysate bath (sodium, 140 mEq/L; calcium, 2–2.5 mEq/L; potassium, 2 mEq/L; magnesium, 1 mEq/L) over 4 h with polysulfone dialyzers. Continuous wave Doppler US was used to measure the hemodynamic parameters at three time points, namely, prior to (pre-HD), 2 h into (2 h into HD), and following (post-HD) each mid-week HD treatment session. The percent change in blood volume was measured by noninvasive hematocrit monitoring. All patients had an annual echocardiogram as part of their standard care. Pulse wave tonometry to derive the augmentation index, central blood pressure, and pulse wave velocity (PWV) was done at the same time. US-based hemodynamic measurements were acquired by a single trained investigator. While on HD, the patient was required to lay flat while the dialysis chair was fully reclined in order to obtain accurate measurements.
Statistical analysis
Continuous variables were expressed either as the median and interquartile range (IQR) or mean ± standard deviation. The median values of the measured hemodynamic parameters pre-HD, 2 h into HD, and post-HD were analyzed using the Kruskal–Wallis test. The variables of interest between patients who had a decline in the cardiac index decline were analyzed using the Mann–Whitney U test. The relationship between cardiac index decline and residual renal function were analyzed by the Fisher exact test. A p value of <0.05 was considered to be significant. All statistical analyses were performed using Stata™ version 11 (StataCorp LP, College Station, TX).
Results
Twenty-four patients fit the inclusion criteria. Two patients were subsequently excluded due to a lack of hemodynamic measurements, and thus 22 patients completed the study. Of these 22 patients, 16 (73 %) were male. The mean age was 17 ± 3.8 years. Table 1 shows the demographics of the study population. Electronic supplementary material Table 1 shows individual patient information. No patient had congenital heart disease. The mean dialysis vintage was 47.8 ± 33.7 months. The single pool Kt/V (spKt/V) was 1.6 ± 0.17, and the mean hemoglobin level was 11.5 g/dL. Eight patients had left ventricular (LV) hypertrophy based on LV mass index (LVMI) criteria. No patient experienced intradialytic hypotension requiring intervention on the study day.
The cardiac index decreased significantly midway through the HD session and remained low until the end of treatment [Table 2: 3.38 (IQR 2.9–4.58) to 3.24 (IQR 2.5–3.82); p < 0.005). The stroke volume decreased throughout the treatment. The heart rate did increase during the treatment, but the increase was not sufficient to maintain the cardiac index. Two patients were on a low dose of angiotensin-converting-enzyme inhibitor and beta blocker for cardiac remodeling, but this did not affect the decline in the cardiac index. The cardiac index failed to return to pre-HD values at treatment completion. PWV did not change during HD (Table 2). Only one patient complained of dizziness and light headedness during the treatment; all other patients were asymptomatic despite a decline in cardiac index.
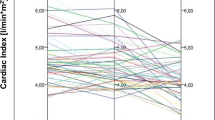
Of the 22 patients, 12 (54 %) had a significant decline in cardiac index by mid-treatment. When the patients were divided into two groups based on changes in cardiac index, there were no significant differences between weight, age, vintage, adequacy, LVMI, amount of ultrafiltration, and percentage fluid overload between the two groups (Table 3). The decrease in blood volume at 2 h into the HD session (R = 0.43, p = 0.045) and at the end of the HD session (4 h; R = 0.56, p = 0.007) was the only association with cardiac index decline (Fig. 1).
Discussion
We found that more than half of our patients had a significant decline in their cardiac index that failed to recover at the end of the dialysis treatment. Cardiac index and stroke volume decreased significantly during the HD session. To our knowledge this is the first study that has utilized a noninvasive bedside tool to demonstrate this phenomenon in pediatric and adolescent patients receiving maintenance HD. Healthy individuals who are fluid overloaded would be able to increase their cardiac contractility due to Starling forces when preload falls. However, most patients with ESRD have a stiffer left ventricle which likely blunts this response, causing a fall in cardiac output with preload reduction during dialysis [15]. With the blunted response, the only way compensation could occur is either by an increase in heart rate or by an increase in systemic vascular resistance. In our study, the heart rate did increase, but the increase was not enough to compensate for the fall in cardiac output for these patients at risk. The systemic vascular resistance did not increase during dialysis, as measured by the US cardiac output monitor and PWV. This phenomenon is well known in adults and thought to be related to autonomic insufficiency and diminished baroreceptor response [16–19]. Our results indicate that the normal physiological ventriculoarterial coupling response to declining preload and cardiac index appears to be disrupted even in children and young adults receiving chronic HD. In addition, our patients with these changes were asymptomatic, which is concerning. The rate of fluid removal was the only significant risk factor for a compromised cardiac index during HD. The total amount of fluid removed or the percentage fluid overload was not different between groups; however, this could have been due to a smaller sample size in our patient population.
Adverse cardiovascular effects of intradialytic hemodynamic changes have been shown eloquently by McIntyre and colleagues in adult patients. In one study, myocardial stunning occurred in up to two-thirds of adult patients during HD [20]. This group demonstrated that both intradialytic reductions in blood pressure and ultrafiltration volume independently determined the propensity for cardiac injury during dialysis [21]. In a follow-up study of 50 patients with myocardial stunning, 30 patients developed a fixed reduction in systolic function of >60 % in the stunned segments within 1 year [22]. Hothi et al. reported similar findings in pediatric patients and found that the number of stunned segments and the intensity of stunning within the segments on echocardiograms correlated with intradialytic blood pressure changes and ultrafiltration volume [23]. Utilizing detailed echocardiograms during HD sessions, while being the gold standard for detecting segmental wall motion abnormalities, is costly and may not be practical. As we have shown in our study, relying on symptomatology or traditional hemodynamic measurements, such as blood pressure and heart rate, to guide safe rate of fluid removal is a late measure, and subtle changes in cardiac index with resultant subclinical myocardial stunning may be missed.
Doppler US-driven hemodynamic measurements have been used to guide treatment in patients in shock by supplying information on the cardiac index, stroke volume, and systemic vascular resistance among other measured and derived parameters. Due to inter-observer variability, the trend, rather than the absolute measurements, can be considered to be more reliable. This tool is portable, easy to use, easy to gain expertise in without the requirement for prolonged training, and could offer a novel hemodynamic monitoring option for the outpatient HD unit.
Our study has a a few limitations. The findings are limited by the small number of patients, which could have impacted the contribution of other variables, such as ultrafiltrate volume. Repeated measurements of these variables in patients could increase the validity of the study.
In summary, we have shown that even in children and young adults receiving maintenance HD, the cardiac index falls in more than half the patients during dialysis and is associated with the rate of fluid removal. Conventional methods currently used for assisting fluid removal in HD are inadequate to assess hemodynamic changes. Prescriptions with individualized rate of fluid removal and intradialytic noninvasive CV monitoring are urgently needed to address pediatric patients with falling cardiac index during HD treatments.
References
U.S. Renal Data System Coordinating Center (2014) Annual data report: Atlas of end-stage renal disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda
Parekh RS, Carroll CE, Wolfe RA, Port FK (2002) Cardiovascular mortality in children and young adults with end-stage kidney disease. J Pediatr 141:191–197
Mitsnefes MM (2012) Cardiovascular disease in children with chronic kidney disease. J Am Soc Nephrol 23:578–585
Kalantar-Zadeh K, Block G, Humphreys MH, Kopple JD (2003) Reverse epidemiology of cardiovascular risk factors in maintenance dialysis patients. Kidney Int 63:793–808
McIntyre CW, Odudu A (2014) Hemodialysis-associated cardiomyopathy: a newly defined disease entity. Semin Dial 27:87–97
Selby NM, McIntyre CW (2007) The acute cardiac effects of dialysis. Semin Dial 20:220–228
Braunwald E, Kloner RA (1982) The stunned myocardium: prolonged, postischemic ventricular dysfunction. Circulation 66:1146–1149
Camici PG, Prasad SK, Rimoldi OE (2008) Stunning, hibernation, and assessment of myocardial viability. Circulation 117:103–114
McIntyre CW, Burton JO, Selby NM, Leccisotti L, Korsheed S, Baker CSR, Camici PG (2008) Hemodialysis-induced cardiac dysfunction is associated with an acute reduction in global and segmental myocardial blood flow. Clin J Am Soc Nephrol 3:19–26
Selby NM, Lambie SH, Camici PG, Baker CS, McIntyre CW (2006) Occurrence of regional left ventricular dysfunction in patients undergoing standard and biofeedback dialysis. Am J Kidney Dis 47:830–841
Selby NM, Burton JO, Chesterton LJ, McIntyre CW (2006) Dialysis-induced regional left ventricular dysfunction is ameliorated by cooling the dialysate. Clin J Am Soc Nephrol 1:1216–1225
Burton JO, Jefferies HJ, Selby NM, McIntyre CW (2009) Hemodialysis-induced cardiac injury: determinants and associated outcomes. Clin J Am Soc Nephrol 4:914–920
Stewart GM, Nguyen HB, Kim TY, Jauregui J, Hayes SR, Corbett S (2008) Inter-rater reliability for noninvasive measurement of cardiac function in children. Pediatr Emerg Care 24:433–437
Cattermole GN, Leung PY, Mak PS, Chan SS, Graham CA, Rainer TH (2010) The normal ranges of cardiovascular parameters in children measured using the Ultrasonic Cardiac Output Monitor. Crit Care Med 38:1875–1881
de Simone G (2003) Left ventricular geometry and hypotension in end-stage renal disease: a mechanical perspective. J Am Soc Nephrol 14:2421–2427
Chesterton LJ, Selby NM, Burton JO, McIntyre CW (2009) Cool dialysate reduces asymptomatic intradialytic hypotension and increases baroreflex variability. Hemodial Int 13:189–196
Pickering TG, Gribbin B, Oliver DO (1972) Baroreflex sensitivity in patients on long-term haemodialysis. Clin Sci 43:645–657
Chesterton LJ, Selby NM, Burton JO, Fialova J, Chan C, McIntyre CW (2010) Categorization of the hemodynamic response to hemodialysis: the importance of baroreflex sensitivity. Hemodial Int 14:18–28
Robinson TG, Carr SJ (2002) Cardiovascular autonomic dysfunction in uremia. Kidney Int 62:1921–1932
Burton JO, Korsheed S, Grundy BJ, McIntyre CW (2008) Hemodialysis-induced left ventricular dysfunction is associated with an increase in ventricular arrhythmias. Ren Fail 30:701–709
McIntyre CW (2009) Effects of hemodialysis on cardiac function. Kidney Int 76:371–375
Burton JO, Jefferies HJ, Selby NM, McIntyre CW (2009) Hemodialysis-induced repetitive myocardial injury results in global and segmental reduction in systolic cardiac function. Clin J Am Soc Nephrol 4:1925–1931
Hothi DK, Rees L, Marek J, Burton J, McIntyre CW (2009) Pediatric myocardial stunning underscores the cardiac toxicity of conventional hemodialysis treatments. Clin J Am Soc Nephrol 4:790–797
Acknowledgments
The authors gratefully acknowledge the support of the dedicated medical staff at Texas Children’s Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Baylor College of Medicine Institutional Review Board approved the study protocol prior to study initiation. Patients were included after written informed consent from their parents or guardians and child assent had been obtained.
Disclosures
Poyyapakkam Srivaths is supported by a Baxter Clinical grant and a Casey Lee Ball Foundation grant. Ayse Akcan Arikan has consulted for Baxter. The remaining authors have no disclosures.
Additional information
Parts of this manuscript were presented at the American Society of Nephrology–Kidney Week 2014 and the Annual Dialysis Conference 2014 where it won the “Best Pediatric Abstract Award”
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplemental Table 1
(DOCX 14 kb)
Rights and permissions
About this article
Cite this article
Geer, J.J., Shah, S., Williams, E. et al. Faster rate of blood volume change in pediatric hemodialysis patients impairs cardiac index. Pediatr Nephrol 32, 341–345 (2017). https://doi.org/10.1007/s00467-016-3486-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-016-3486-2