Abstract
Background
The goal of this study was to examine national trends in hospitalization, emergency department (ED) utilization, secondary diagnoses, and charges associated with pediatric urolithiasis.
Methods
Data were evaluated from the Kids’ Inpatient Database of the Healthcare Costs and Utilization Project (HCUP) database from 1997 to 2012 and the HCUP National ED Sample from 2006 to 2011.
Results
Pediatric nephrolithiasis discharges increased by 18 %, while ureterolithiasis discharges decreased by 17 %. Hospital charges increased by 20 % when accounting for inflation, despite an overall decrease in discharges by 2.5 %. Female patients and those aged 15–17 years were more commonly affected. Pediatric ED visits increased by 9 %. The most common secondary diagnoses during 2003–2009 were urinary tract infections (UTI) (13 %), asthma (9 %), epilepsy (4 %), and paralysis (4 %).
Conclusions
Decreased hospitalizations and increased ED visits indicate a shift to outpatient care. Inpatient health care charges associated with pediatric urolithiasis continue to rise. Comorbidities include UTI, asthma, epilepsy, attention deficit hyperactivity disorder (ADHD), and mood disorders. Because of the significant health care burden and the increased risk to children of developing long-term sequelae there is a strong need for increased research into the mechanism of this systemic inflammatory disease and improved therapeutic targets.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urolithiasis has afflicted humans since early history as demonstrated by its presence in Egyptian mummies and mention in the Hippocratic Oath (http://www.nlm.nih.gov/hmd/greek/greek_oath.html). The ubiquitous presence of urolithiasis in human history can be easily understood when considering the difficulties of balancing calcium-based skeletal system turnover with the water conservation necessary for terrestrial life [1]. Urolithiasis burden in adults has been well established with an approximate lifetime risk of 10–15 % [1]. Traditionally, more frequent in male patients than in female patients, recent trends indicate a shift to a more balanced gender ratio [2, 3]. Currently, the health care burden of urolithiasis is substantial with 185,000 hospitalizations and 2 million outpatient visits annually. These account for over $2 billion spent on diagnosis and treatment [4].
Previously considered an uncommon cause of pediatric morbidity, mounting evidence indicates a progressive increase in urolithiasis frequency and cost. Some of the earliest data come from Sas et al., who reported an increased incidence in children in South Carolina from 7.9 per 100,000 children in 1996 to 18.5 per 100,000 children in 2007. During that time the amount of money spent on the care of pediatric urolithiasis increased by greater than four-fold [5]. These findings were echoed on a national level when Routh et al. looked at data from the Pediatric Health Information System (PHIS) database for 1999–2008. They showed an adjusted annual increase of 10.6 % in the number of pediatric urolithiasis patients [5]. This increase may in part be due to increased surveillance, but the etiology remains unelucidated and urolithiasis now accounts for 1 in 685 pediatric admissions [6].
The increase in pediatric urolithiasis is concerning given the economic burden associated with the treatment and morbidity associated with this condition. To further investigate the etiology and epidemiology of increasing pediatric urolithiasis we have examined data from the Kids’ Inpatient Database (KID) as well as the Healthcare Cost and Utilization Project (HCUP) National Emergency Room Sample for children.
Materials and methods
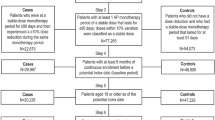
The KID is a component of the HCUP, which is sponsored by the Agency for Healthcare Research and Quality (AHRQ). It provides information on pediatric inpatient discharges by pulling raw data from a sample of American pediatric hospitals and converting it into weighted data to provide estimates of pediatric care on a national level. Participation has grown from 22 states in 1997 to 44 in 2012 and contains information from close to 4,000 hospitals; however, a minority of these represent children’s hospitals. The weighted data available from the KID are typical of a hospital discharge record, including demographics, diagnostic and procedural codes, payer and financial data, length of stay, and discharge disposition; data are available on patients regardless of payer, including persons covered by private insurance, Medicaid, Medicare, and the uninsured. No physiological or laboratory data are collected. We evaluated KID data from 1997, 2000, 2003, 2006, 2009, and 2012. The 1997 version contained just over 6 million total discharges whereas the 2012 version contains over 20 million.
The Nationwide Emergency Department Sample (NEDS) database gives national estimates of emergency department (ED) visits. We collected data from 2006 to 2011 to yield the total number of Pediatric Emergency Department (ED) visits associated with urolithiasis.
We identified patients using International Classification of Disease 9th Edition, Clinical Modification (ICD-9-CM) codes for nephrolithiasis (592.0) and ureterolithiasis (592.1). Data regarding secondary diagnoses were available on the basis of clinical classification software codes for nephrolithiasis from 2003 to 2009.
Results
Demographics
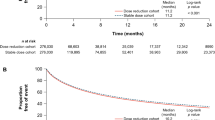
The average number of inpatient pediatric discharges with a primary diagnosis of nephrolithiasis (592.0) increased by 18 % over the study period. Interestingly, nephrolithiasis discharges in the KID peaked in 2006 at 1,651, representing a 35 % increase from 1,073 in 1997, but have since declined. Furthermore, pediatric inpatient discharges for ureterolithiasis (592.1) peaked in 2003 with 2,354, a 28 % increase. Between 2003 and 2012, the number of ureterolithiasis admissions sharply declined, reaching 1,423, which is actually 17 % less than in 1997 (Fig. 1a). The number of pediatric ED visits for nephrolithiasis and ureterolithiasis increased by 9 % from 17,118 in 2006 to 18,620 in 2011 (Fig. 1b). When considering hospital discharges, teenagers aged 15–17 years were the most frequently affected. However, this was more pronounced in the nephrolithiasis group with 15- to 17-year-olds accounting for an average of 62 % (SE 0.69) of patients vs 46 % (SE 1.1) in the ureterolithiasis group (Fig. 2a). Females are more commonly affected than males accounting for 60 % (SE 0.85) of the children affected for both groups from 1997 to 2012. Southern USA was the area with the greatest number of patients, averaging 42 % (SE 0.74) of the total over the 12 years of data collected. The West was the area least affected (Fig. 2b). Geographical data were not available for the ED data set.
Charges
Total aggregate charges for inpatient treatment have increased from US $8,323,479 in 1997 to $17,599,833 in 2012 (Fig. 3). This is a 53 % increase; however, if we account for inflation the charges in 1997 would be comparable to $14,715,817 in 2012 (http://www.halfhill.com/inflation.html). Thus, the actual charges are increased by 20 %, despite an overall decrease in discharges of 2.5 %. The average length of stay shortened for the nephrolithiasis group from 2.7 (SE 0.16) days in 1997 to 2.3 (SE 0.08) days in 2012. The average length of stay increased for the ureterolithiasis group from 1.8 (SE 0.061) days in 1997 to 2 (SE 0.05) days in 2012. Thus, daily inpatient charges for nephrolithiasis increased greatly from approximately $2,700 in 1997 to $10,800 in 2012, while the same charges for ureterolithiasis increased from $2,900 in 1997 to $9,800 in 2012. While children <5 years of age represented the smallest portion (9 %) of discharges, their hospital charges were highest among all the age groups, averaging $1,680/day higher than older patients in 2012.
Associated diagnoses
Common secondary diagnoses of children discharged with a primary diagnosis of nephrolithiasis were available for 2003–2009 data (Table 1). These associations are made available based upon clinical classification software (CCS) categories and the most commonly associated groups are generalized; for example, the top three include: other diseases of kidney and ureters; genitourinary symptoms and ill-defined conditions; and other nutritional, endocrine, and metabolic syndromes. Distinct diagnoses that were commonly associated included UTI, asthma, epilepsy, paralysis, and mood disorders. Unfortunately, data on the number of children discharged with secondary diagnoses vs those without are not available.
Discussion
Pediatric nephrolithiasis discharges peaked at a 35 % increase from 1997 in 2006 and have shown a steady decline in 2009 and 2012. Pediatric ureterolithiasis peaked at a 27 % increase from 1997 in 2003 and has now declined to 17 % lower discharge rates than in 1997. Matlaga et al., using HCUP data from 1997 to 2003, and Routh et al., using PHIS data from 1999 to 2008, both showed that overall pediatric urolithiasis was increasing [7, 8]. However, we have expanded on their previous work by considering nephrolithiasis and ureterolithiasis diagnosis codes separately, including the most recent data, and including emergency room visits. Along with decreasing discharge frequency the increasing pediatric ED visits give evidence for the thought that the frequency of urolithiasis has indeed increased since the late 1990s, but care is now shifting to the outpatient setting. This is further supported by the observation that the length of stay for nephrolithiasis has decreased; however, this is not true for ureterolithiasis. Perhaps the increased length of stay for ureterolithiasis is reflective of only more complex cases requiring admission. This shift is similar to the treatment pattern for adult nephrolithiasis found by the Urologic Diseases in America Project, which showed that care could be managed on an outpatient basis as medical management and minimally invasive surgical techniques were refined [9].
Collectively, these data indicate that pediatric urolithiasis is no longer an uncommon diagnosis, and rising ED visits attest to its growing role in overall pediatric morbidity. Despite the fact that the number of children discharged from the hospital for stone treatment decreased by 2 % from 1997, the mean hospital charges increased by 20 %, taking into account inflation, over our 12-year time frame. Bush et al. reported that an average hospital stay cost US$ 18,000 in 2007; we found an increased average cost of $ 22,000 per stay in 2012 [6]. Overall, the care of adult and pediatric stone disease cost $ 2.1 billion in 2000 [4]. Undoubtedly, pediatric urolithiasis is an area deserving of greater research as it causes significant pain for patients, correlates with poor cardiovascular health and chronic kidney disease (CKD) progression in adults, and is becoming a greater financial burden on the American health care system [10–13].
Our work confirms the female gender predilection for pediatric urolithiasis. Schaefer et al. showed that girls were more commonly diagnosed with urolithiasis than boys by 2:1 [14]. Novak et al. found that girls had a 1.5 times increased risk of urolithiasis compared with boys [15]. Interestingly, this is the reverse of the traditional male gender predilection in adults. However, there is growing evidence that adults may be moving toward gender parity [15]. Scales et al. showed that in 1997 adults had a 1.7:1 male to female ratio vs a 1.3:1 ratio in 2002 [3]. They postulated that while traditionally males had a greater prevalence of obesity, the increase seen across the American population at large was more rapid in the adult female population from 1960 to 2002, and this changing face of obesity mirrored the changing gender ratio of urolithiasis [3]. This association with obesity is lent credence by the lithogenic effects of obesity on urine that include a decrease in urine pH and an increase in the excretion of sodium, phosphorous, and oxalate [16]. The obesity epidemic has affected children in addition to adults. Flegal et al. found that while the prevalence of adult obesity doubled from 1980 to 2002, it tripled in the pediatric population [17]. However, the picture remains cloudy, as some reports suggest that the increasing incidence of obesity might be driving the increasing frequency of nephrolithiasis, while others do not show an association [14, 18, 19]. Another possibility for the female pediatric predominance and male adult predominance of kidney stones may be related to the hormonal changes experienced by both genders as they age. Adult urolithiasis is traditionally male dominated, but at around 60 years of age the male incidence falls, while female incidence increases [1]. The relationship between urolithiasis and hormonal changes is not clear and there are conflicting data concerning the protective effects of testosterone and estrogen. Heller et al. showed a protective effect of estrogen treatment in post-menopausal women. Women who were treated with hormone replacement therapy had decreased calcium excretion and calcium oxalate supersaturation of their urine. There is also evidence of an estrogen-driven increase in citrate secretion, but the mechanism is unknown [20]. Bergsland et al. studied the non-stone-forming relatives of calcium stone-forming patients. They found that the urine of non-stone-forming male relatives had a greater ability to inhibit crystallization than that of non-stone-forming female relatives [21]. Undoubtedly, there needs to be greater research in this area to delineate the true relationships.
Our data showed that the greatest increase in urolithiasis was in patients 15–17 years of age, as this group accounted for approximately 60 % of all discharges. This pattern has been found by others: Bush et al. queried the PHIS database from 2002 to 2004 and found that the odds ratio for hospitalization for urolithiasis was 8.1 if the patient was over 8 years of age [6], and Schaefer and Matlaga both found a 30-fold increased risk of urolithiasis when comparing their youngest patients with their oldest [8, 14]. It is unclear why such a strong relationship exists between age and stone formation. Again, one must wonder about the hormonal influence due to the association of puberty with our adolescent age group. Pietrow et al. found that half of their patients under 10 years of age had identifiable metabolic derangements (i.e., hypercalciuria) [22]. Thus, perhaps our increase in adolescents is more likely the result of external factors such as obesity, which is known to cause increased urine sodium, phosphorus, and oxalate [18]. Another possibility may be the increased freedom of adolescents to make dietary decisions vs younger children. Poor dietary choices, including high salt and low water intake may promote stone formation in this age group.
Others have used clinical experience with adult stone formers and their morbidities to evaluate pediatric stone formers for similar associations. We were interested in using stone formers themselves as a starting point to look for associations that might be unique to pediatric patients. We queried the HCUP database for the most common secondary diagnosis of children with a primary diagnosis of nephrolithiasis on discharge; these data were only available for nephrolithiasis patients from 2003 to 2009. We found that urinary tract infection (UTI), asthma, epilepsy, paralysis, and mood disorders were the most common secondary diagnosis, which specified a disease state via the CCS codes. The association of UTIs and kidney stones is not surprising as UTIs have been described as being both a cause and a consequence of kidney stones [23]. This overlap between kidney stones and UTIs is highlighted by the finding that more than 70 % of children hospitalized for nephrolithiasis received antibiotics [6]. The association with epilepsy is likely two-fold. First, the well-known association of stone formation with the ketogenic diet and second the long-standing history of anti-seizure medications causing stone formation. Topiramate has the best known association; its use can cause up to 10 % prevalence of symptomatic kidney stones secondary to a marked decrease in urine citrate excretion [24]. Further lithogenic effects of topiramate include increasing calcium excretion and elevation of urine pH [25]. Zonisamide, a newer generation antiepileptic drug, is also associated with urolithiasis [26]. Many studies have described the lithogenic effects of a ketogenic diet and stones occur in 1 in 20 children who follow the diet for improved seizure control [27]. This association is mainly due to increased urinary calcium excretion; however, some patients have also shown decreased urinary citrate [28]. What the HCUP coded as paralysis could also be described as immobilization. It has been well established that the lack of weight-bearing on bones often leads to resorptive hypercalciuria and these patients frequently have urolithiasis because of increased solute loads of calcium [29, 30]. Immobilized patients on lithogenic antiepileptic medicines may particularly be at risk. Asthma is a common inflammatory pediatric condition that was associated with 9 % of stone discharges, and is often treated with corticosteroids. There have been other systemic inflammatory conditions that are treated with steroids and associated with nephrolithiasis. One well-known example includes inflammatory bowel disease [31, 32]. However, stones have also been associated with inflammatory conditions that are not treated with steroids such as diabetes [33, 34]. Thus, one must wonder if it is the inflammation or the steroid use that predisposes these patients to stone formation [35, 36]. Of course, it may simply be coincidental, due to the commonality of asthma in the pediatric population. Another puzzling association is that of mood disorders and ADHD with nephrolithiasis; while topiramate is at times used for mood disorder treatment, it is not commonplace and is unlikely to account for the association. We speculate that changing dietary and fluid habits associated with stimulant medications could predispose children to stone formation. Perhaps as we move toward understanding nephrolithiasis as a complex systemic disease for both children and adults, the association between such varied medical conditions and nephrolithiasis will become clearer.
Historically, urolithiasis has afflicted patients more frequently in southern USA, giving it the distinction of being called the “stone belt” [9, 37, 38]. This geographic association is thought to be related to ambient temperatures and sunlight exposure. Our data have shown that pediatric urolithiasis patterns follow those of adults. Interestingly, Bush et al., using PHIS data from 2002 to 2004, showed that pediatric urolithiasis was more common in the north central region of the USA [6]. It is unclear why this discrepancy exists, although it is most likely the result of differing data collection practices between the PHIS and the HCUP.
This study has several limitations, many of which are the result of attempting to analyze pediatric urolithiasis on a national level. The HCUP database allows us to investigate trends in discharges and aggregate charges on a national level, rather than in individual institutions. However, HCUP data are derived from coding and may be unreliable. Coding practices vary between institutions and practitioners, and data may be affected by these practices rather than representing true patient variation. Furthermore, we are unable to differentiate multiple discharges for the same patient, and children with difficult-to-treat disease who require repetitive hospitalizations may artificially burgeon the numbers. In addition, granular patient data are lacking, including individual medication regimens and laboratory results that would allow us to make more meaningful conclusions. Also inherent in the use of coding data is the difficulty of differentiating nephrolithiasis and ureterolithiasis. However, we feel that both diagnosis codes should be used to give a more complete picture, despite the lack of validation concerning the correlation of code usage with actual stone location. Last, the HCUP only includes data from inpatient care and cannot make any direct conclusions regarding the efflux of pediatric nephrolithiasis patients to outpatient care. This lack of outpatient data also limits our ability to make comprehensive statements about the total cost of urolithiasis treatment, as we are unable to account for the likely substantial amount of care that goes on outside of the hospital. Additionally, aggregate charges are available, but not the amount of money that is actually recouped by the hospital, further complicating any true estimate of cost. However, we feel that the ability to use HCUP data as a hypothesis-generating tool still holds great merit. Hopefully, as the importance and impact of this disease grow, improved data sets may become available.
Other work has used the HCUP and PHIS databases to look at pediatric urolithiasis, but to our knowledge, none is as comprehensive longitudinally as this paper, which contains data from 1997 to 2012. We have shown that the frequency of children receiving medical care for kidney stones has increased. This care is shifting to the outpatient setting, as demonstrated by the increase in ED visits and decreasing hospitalizations. However, while the number of hospital discharges has decreased, charges associated with urolithiasis hospitalizations have increased. The association between pediatric nephrolithiasis and asthma, seizures, and immobilization may give further insight into the unelucidated mechanisms of this disease state. The growing number of pediatric patients with this disease is very troubling because of the growing body of data supporting the association with adult urolithiasis, with significant morbidities such as acute myocardial infarction, atherosclerosis, and chronic kidney disease [10, 11, 13]. One may postulate that children’s longer exposure period to this systemic inflammatory disorder will likely increase the risk for these sequelae. Thus, the growing morbidity, financial burden, and concern regarding the long-term sequelae make a poignant plea for further investigation and study into the pathogenesis of the disease, as well as improved therapeutic targets.
References
Moe OW (2006) Kidney stones: pathophysiology and medical management. Lancet 367:333–344
Coe FL, Parks JH, Asplin JR (1992) The pathogenesis and treatment of kidney stones. N Engl J Med 327:1141–1152
Scales CD Jr, Curtis LH, Norris RD, Springhart WP, Sur RL, Schulman KA, Preminger GM (2007) Changing gender prevalence of stone disease. J Urol 177:979–982
Lotan Y (2009) Economics and cost of care of stone disease. Adv Chronic Kidney Dis 16:5–10
Sas DJ, Hulsey TC, Shatat IF, Orak JK (2010) Increasing incidence of kidney stones in children evaluated in the emergency department. J Pediatr 157:132–137
Bush NC, Xu L, Brown BJ, Holzer MS, Gingrich A, Schuler B, Tong LY, Baker LA (2010) Hospitalizations for pediatric stone disease in United States, 2002–2007. J Urol 183:1151–1156
Routh JC, Graham DA, Nelson CP (2010) Epidemiological trends in pediatric urolithiasis at United States freestanding pediatric hospitals. J Urol 184:1100–1104
Matlaga BR, Schaeffer AJ, Novak TE, Trock BJ (2010) Epidemiologic insights into pediatric kidney stone disease. Urol Res 38:453–457
Pearle MS, Calhoun EA, Curhan GC (2005) Urologic diseases in America project: urolithiasis. J Urol 173:848–857
Gillen DL, Worcester EM, Coe FL (2005) Decreased renal function among adults with a history of nephrolithiasis: a study of NHANES III. Kidney Int 67:685–690
Liu Y, Li S, Zeng Z, Wang J, Xie L, Li T, He Y, Qin X, Zhao J (2014) Kidney stones and cardiovascular risk: a meta-analysis of cohort studies. Am J Kidney Dis 64:402–410
Rule AD, Bergstralh EJ, Melton LJ 3rd, Li X, Weaver AL, Lieske JC (2009) Kidney stones and the risk for chronic kidney disease. Clin J Am Soc Nephrol 4:804–811
Rule AD, Roger VL, Melton LJ 3rd, Bergstralh EJ, Li X, Peyser PA, Krambeck AE, Lieske JC (2010) Kidney stones associate with increased risk for myocardial infarction. J Am Soc Nephrol 21:1641–1644
Schaeffer AJ, Feng Z, Trock BJ, Mathews RI, Neu AM, Gearhart JP, Matlaga BR (2011) Medical comorbidities associated with pediatric kidney stone disease. Urology 77:195–199
Novak TE, Lakshmanan Y, Trock BJ, Gearhart JP, Matlaga BR (2009) Sex prevalence of pediatric kidney stone disease in the United States: an epidemiologic investigation. Urology 74:104–107
Obligado SH, Goldfarb DS (2008) The association of nephrolithiasis with hypertension and obesity: a review. Am J Hypertens 21:257–264
Flegal KM, Tabak CJ, Ogden CL (2006) Overweight in children: definitions and interpretation. Health Educ Res 21:755–760
Kokorowski PJ, Routh JC, Hubert KC, Graham DA, Nelson CP (2012) Association of urolithiasis with systemic conditions among pediatric patients at children’s hospitals. J Urol 188:1618–1622
Taylor EN, Stampfer MJ, Curhan GC (2005) Obesity, weight gain, and the risk of kidney stones. JAMA 293:455–462
Heller HJ, Sakhaee K, Moe OW, Pak CY (2002) Etiological role of estrogen status in renal stone formation. J Urol 168:1923–1927
Bergsland KJ, Kinder JM, Asplin JR, Coe BJ, Coe FL (2002) Influence of gender and age on calcium oxalate crystal growth inhibition by urine from relatives of stone forming patients. J Urol 167:2372–2376
Pietrow PK, Pope JCT, Adams MC, Shyr Y, Brock JW 3rd (2002) Clinical outcome of pediatric stone disease. J Urol 167:670–673
Borghi L, Nouvenne A, Meschi T (2012) Nephrolithiasis and urinary tract infections: ‘the chicken or the egg’ dilemma? Nephrol Dial Transplant 27:3982–3984
Welch BJ, Graybeal D, Moe OW, Maalouf NM, Sakhaee K (2006) Biochemical and stone-risk profiles with topiramate treatment. Am J Kidney Dis 48:555–563
Corbin Bush N, Twombley K, Ahn J, Oliveira C, Arnold S, Maalouf NM, Sakhaee K (2013) Prevalence and spot urine risk factors for renal stones in children taking topiramate. J Pediatr Urol 9:884–889
Israni RK, Kasbekar N, Haynes K, Berns JS (2006) Use of antiepileptic drugs in patients with kidney disease. Semin Dial 19:408–416
Sampath A, Kossoff EH, Furth SL, Pyzik PL, Vining EP (2007) Kidney stones and the ketogenic diet: risk factors and prevention. J Child Neurol 22:375–378
Furth SL, Casey JC, Pyzik PL, Neu AM, Docimo SG, Vining EP, Freeman JM, Fivush BA (2000) Risk factors for urolithiasis in children on the ketogenic diet. Pediatr Nephrol 15:125–128
Stewart AF, Adler M, Byers CM, Segre GV, Broadus AE (1982) Calcium homeostasis in immobilization: an example of resorptive hypercalciuria. N Engl J Med 306:1136–1140
Craven BL, Passman C, Assimos DG (2008) Hypercalcemic states associated with nephrolithiasis. Rev Urol 10:218–226
Cury DB, Moss AC, Schor N (2013) Nephrolithiasis in patients with inflammatory bowel disease in the community. Int J Nephrol Renovasc Dis 6:139–142
Clark JH, Fitzgerald JF, Bergstein JM (1985) Nephrolithiasis in childhood inflammatory bowel disease. J Pediatr Gastroenterol Nutr 4:829–834
Lieske JC, de la Vega LS, Gettman MT, Slezak JM, Bergstralh EJ, Melton LJ 3rd, Leibson CL (2006) Diabetes mellitus and the risk of urinary tract stones: a population-based case-control study. Am J Kidney Dis 48:897–904
Taylor EN, Stampfer MJ, Curhan GC (2005) Diabetes mellitus and the risk of nephrolithiasis. Kidney Int 68:1230–1235
Faggiano A, Pivonello R, Melis D, Filippella M, Di Somma C, Petretta M, Lombardi G, Colao A (2003) Nephrolithiasis in Cushing’s disease: prevalence, etiopathogenesis, and modification after disease cure. J Clin Endocrinol Metab 88:2076–2080
Danese S, Semeraro S, Papa A, Roberto I, Scaldaferri F, Fedeli G, Gasbarrini G, Gasbarrini A (2005) Extraintestinal manifestations in inflammatory bowel disease. World J Gastroenterol 11:7227–7236
Soucie JM, Coates RJ, McClellan W, Austin H, Thun M (1996) Relation between geographic variability in kidney stones prevalence and risk factors for stones. Am J Epidemiol 143:487–495
Brikowski TH, Lotan Y, Pearle MS (2008) Climate-related increase in the prevalence of urolithiasis in the United States. Proc Natl Acad Sci U S A 105:9841–9846
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kusumi, K., Becknell, B. & Schwaderer, A. Trends in pediatric urolithiasis: patient characteristics, associated diagnoses, and financial burden. Pediatr Nephrol 30, 805–810 (2015). https://doi.org/10.1007/s00467-014-3012-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-014-3012-3