Abstract
Background
The aim of this study was to evaluate the presence of subclinical cardiovascular disease (CVD) and its relation to risk factors in pediatric patients with steroid-resistant nephrotic syndrome (NS).
Methods
Thirty-seven patients with normal renal function were compared with 22 healthy controls regarding the presence of subclinical CVD. Measurements included aortic pulse wave velocity (PWV), carotid intima media thickness (IMT), and left ventricular mass (LVM). Patients were additionally assessed for blood pressure (BP) pattern and the presence of hypertension by 24-h ambulatory blood pressure monitoring.
Results
Compared with the controls, patients had significantly higher mean aortic PWV-standard deviation scores (SDS), mean carotid IMT-SDS, and LVM index (p < 0.001 for all). Increased aortic PWV was noted in 5 % of patients, increased carotid IMT in 22 %, and increased LVM index in 19 %. Five patients (14 %) were hypertensive, and mean BP indexes, SDS, and BP loads during nighttime were significantly higher than those during daytime (p < 0.001 for all). Multivariate analysis revealed a significant relationship between PWV-SDS and ferritin (R 2 = 0.269, p = 0.006) and between carotid IMT-SDS and proteinuria (R 2 = 0.141, p = 0.022). The LVM index was independently associated only with higher body mass index SDS (R 2 = 0.317, p < 0.001). In addition, six patients (16 %) had multiple abnormal subclinical CVD markers, and increased subclinical CVD risk was independently associated only with higher low-density lipoprotein cholesterol (R 2 = 0.292, p = 0.044).
Conclusions
Based on these results, steroid-resistant NS children generally are at high risk of cardiovascular complications, but the increased risk is likely to be multifactorial.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic nephrotic syndrome (NS) in the adult population is considered to be an important risk factor for accelerated atherosclerosis [1]. However the role of idiopathic NS in the development of atherosclerosis in childhood remains unclear [2, 3].
There is little or no risk of cardiovascular disease (CVD) in children with steroid-sensitive NS because of the transient nature of the metabolic abnormalities and steroid exposure [3, 4]. However, the duration of nephrotic dyslipidemia appears to be a critical factor for initiating vascular damage and, therefore, an increased risk of premature atherosclerosis exists in patients with unremitting NS [5, 6]. Moreover, these patients frequently have several additional risk factors, such as hypertension, obesity, insulin resistance, inflammation, long-term treatment with steroids and other immunosuppressive drugs, such as cyclosporine A, hypercoagulability, and oxidative stress. All of these risk factors may act in concert to produce atherosclerotic vascular lesions [6–8].
Given their lifelong exposure to atherogenic risk factors, children and adolescents with idiopathic steroid-resistant NS (SRNS) are at particularly high risk for developing premature atherosclerosis and are therefore ideal candidates for primary prevention. Several non-invasive methods are increasingly being used for the identification of structural and functional vascular abnormalities. The measurement of carotid intima-media thickness (IMT) is a reliable and widely used method to determine vascular disease, which is characterized by fibrosis of the intima and calcification of the media [8]. Pulse wave velocity (PWV) reflects arterial elasticity, which is used for the assessment of functional vascular changes, such as arterial stiffness [9].
To date, no systematic assessment of the cardiovascular status has been performed in pediatric patients with SRNS with respect to the assessment of arterial stiffness, carotid IMT, and left ventricular hypertrophy (LVH). The aim of the study reported here was to determine the presence of subclinical CVD and its association with risk factors in children with idiopathic SRNS. We examined both functional and structural abnormalities in the arteries and performed a cardiac assessment.
Materials and methods
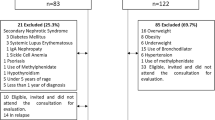
Study population
This cross-sectional observational study was conducted between February and May 2011. Thirty-seven patients aged between 7.9 and 18.8 years treated for SRNS with an estimated glomerular filtration rate (eGFR) of >90 ml/min/1.73 m2 [10] were recruited from the Pediatric Nephrology Divisions of Göztepe Research and Training Hospital and Cerrahpaşa Medical Faculty. SRNS was diagnosed according to the criteria recommended by the International Study for Kidney Disease in Children [11]. Based on renal biopsy results, the diagnoses of primary glomerular disease were as follows: focal segmental glomerulosclerosis (n = 30 patients), minimal change disease (n = 6), and diffuse mesangial proliferation (n = 1). The medical charts of each individual patient were reviewed for the following information: age, gender, age at diagnosis, disease duration, quantification of biochemical data, and the use of steroid, cyclosporine A, and other medications. The time-integrated mean values of serum concentrations of total protein, albumin, and lipids were calculated using the average of the values for the last 1 year. Hypoalbuminemia was defined by a serum albumin concentration of <2.5 g/dl. Nephrotic-range proteinuria was defined as >40 mg/m2 per hour of protein in a 24-h urine collection. All measurements of 24-h urinary protein excretions during relapses were documented and expressed as milligrams per square meter per day, and cumulative proteinuria was calculated as the area under the curve (AUC), which was computed by the trapezoidal rule using Microsoft Excel (Microsoft, Redwood, WA). All doses of prednisone and methylprednisolone were documented and converted to prednisolone equivalents. The mean daily doses of prednisolone and cyclosporine A (mg/kg per day) were calculated using the patient’s weight at the time of the use, and then their cumulative doses were also calculated as an AUC. Patients were not excluded if they were taking angiotensin-converting enzyme inhibitors (ACEIs), angiotensin receptor blockers (ARBs), or statins, since these treatments constitute best clinical practice.
Twenty-two healthy volunteers served as the control group. Control data were used to compare the results of cardiovascular measurements (aortic PWV, carotid IMT and LVH) and metabolic parameters. The study protocol was approved by the local Ethics Committee. An informed consent to participate in the study according to the recommendations of the Declaration of Helsinki on Biomedical Research Involving Human Studies was obtained from all children and/or their parents.
Anthropometric measurements
Weight (kg) and height (cm) of the subjects were measured by the same two nurses. For the assessment of growth in terms of weight and height, standard deviation scores (SDS) of weight and height of an individual measurement were computed for each sex using the least mean squares (LMS) method from growth references for Turkish children [12]. The body mass index (BMI) was calculated as weight/height2 (kg/m2); the SDS of BMI was also computed using the LMS method from BMI references for Turkish children [13]. The weight status of the patients was categorized according to the Turkish BMI-for age/gender-centile curves.
Laboratory measurements
Blood samples were drawn in the morning after an overnight fast (at least 8 h) and used in laboratory tests to determine serum levels of ferritin, fibrinogen, C-reactive protein (CRP), glucose, insulin, and other routine biochemical parameters, including urea, creatinine, albumin, triglycerides, total cholesterol, low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C). Biochemical parameters were measured by routine laboratory methods. Serum insulin levels were analyzed by the chemiluminescence immunoassay method. The homeostasis model assessment of insulin resistance (HOMA-IR) was calculated as an estimate of insulin resistance using fasting levels of plasma glucose and insulin [HOMA-IR = fasting plasma glucose (mg/dl) × fasting plasma insulin (μU/ml)/405] [14]. Insulin resistance was defined as a HOMA-IR of >95th percentile according to sex and pubertal stages, as calculated in Italian children and adolescents by D’Annunzio et al. [15].
Ambulatory blood pressure monitoring
Hypertension was assessed by measuring the ambulatory blood pressure (BP) using a SpaceLabs 91207 oscillometric device (SpaceLabs Healthcare, Snoqualmie, WA). Measurements were obtained every 30 min during daytime and every 60 min during sleep over a 22–h period. The mean systolic blood pressure (SBP) and diastolic blood pressure (DBP) during both daytime and nighttime and also during a 24-h period were calculated. Indexed SBP, DBP, and mean arterial BP (MAP) were calculated by dividing the observed BP by gender and the height-specific 95th percentile of BP [16]. The height-specific SDS was also calculated for each patient’s mean BP according to the methods of Wühl et al. [17]. BP load was defined as the percentage of BP measurements above the 95th percentile for gender and height [16]. Dipping was calculated as the difference between daytime and nighttime BP. Nocturnal dipping was defined as a ≥10 % decline in mean systolic and diastolic ambulatory BP levels from day to night. Ambulatory hypertension was defined as 24-h MAP above the 95th percentile and/or a SBP or DBP load of ≥25 %.
Vascular assessments
Pulse wave velocity
Aortic (carotid–femoral) PWV for assessing central arterial stiffness was performed using the Vicorder system (Skidmore Medical, Bristol, UK) that measures pressure waveforms with a volume displacement technique. After the patient had rested for 15 min in a supine position, the brachial BP and heart rate were measured using an oscillometric device (PRO 1000; DinaMAP, Freiberg, Germany). BP cuffs for the PWV were then placed around both the neck at the level of the carotid artery and the right upper thigh to measure the femoral pulse in the supine position, as described previously [18]. The cuffs were each inflated to 60 mmHg and both carotid and femoral waveforms simultaneously recorded. The aortic PWV was then measured. Three measurements were obtained for each patient, and these were used to obtain an average aortic PWV for that patient. The SDS for the aortic PWV were computed by height-specific normative values using obtained applanation tonometry [19], due to the best agreement between the two methods [18]. An increased aortic PWV was defined as an SDS of the aortic PWV of >2.
Carotid artery IMT
Carotid IMT was measured in the common carotid artery on longitudinal B-mode images obtained with a high-resolution ultrasound instrument (Acuson P50 portable ultrasound system; Siemens, Munich, Germany) equipped with a 5- to 7.5-MHz linear array transducer. Three to five measurements were manually obtained on both carotid arteries at a distance 1–2 cm proximal of the bifurcation; these were averaged for each patient according to international radiologic consensus recommendations [20]. The SDS for the carotid IMT was computed by the LMS method using height-specific normative values [21]. An increased carotid IMT was defined as an SDS of the carotid IMT of >2.
Echocardiography
Transthoracic echocardiography was performed on all patients by the same cardiologist to diagnose LVH, using a Siemens Acuson CV70 instrument equipped with 2.5-MHz transducers. M-mode measurements of the left ventricular end diastolic dimension, interventricular septal thickness (IVST), and posterior wall thickness (PWT) were taken at the left ventricular minor axis, as recommended by the American Society of Echocardiography [22]. The left ventricular mass (LVM) was calculated with the following equation: LVM = 0.8 {1.04 [left ventricular internal dimension (LVID) + PWT + IVST]3 − (LVID)3} + 0.6 g [23]. The LVM was indexed to body size by dividing it by patient height2.7 to become the LVM index, [24]. LVH was defined as an LVM index greater than the age-specific 95th percentile for the indexed LVM index in children and adolescents [25]
Statistical analysis
Statistical analysis was performed with the SPSS ver. 15.0 package program for Windows (SPSS, Chicago, IL). Descriptive statistics were used for the characteristics of the study population. Normally distributed continuous data are expressed as the mean ± standard deviation, and non-normally distributed variables are expressed as the median and interquartile range (25–75th percentile). Urinary protein excretion, the dose of prednisolone and cyclosporine A, serum albumin, triglycerides, cholesterol, ferritin, and CRP values were log transformed to obtain normal distributions. The Mann–Whitney U test was used to compare continuous data between the two groups. Categorical variables were presented as a number (percentages) and compared by using the chi-square test and the Fisher’s exact test. The Wilcoxon two-sample test was performed to compare the BP between daytime and nighttime. The Spearman’s rank and Pearson correlation analyses were used to examine the associations of cardiovascular markers (aortic PWV, carotid IMT, and LVM index) with potential risk factors. The variables that showed a p value of ≤0.05 in the univariate analysis were tested in a stepwise model of multivariate linear regression analysis for each cardiovascular marker. The statistical significance was defined as a two-tailed p value of ≤ 0.05.
Results
Clinical and laboratory findings
Thirty-seven consecutive patients (18 males, 19 females) with idiopathic SRNS and 22 healthy children were enrolled in the study. Clinical characteristics of the patients and the controls are summarized in Table 1. There were no differences in age, male to female ratio, or BMI-SDS between the patient and control groups. Seven of the patients were obese and only one was overweight. None of the patients were underweight.
The mean duration the disease was followed for was 94.5 ± 59.4 (median 80.6, from 52.4 to 127.9) months. Of the 37 patients, 13 had nephrotic-range proteinuria, of whom five were also hypoalbuminemic at the time of study. The mean urinary protein excretions were 84.2 ± 29.1 and 4.6 ± 2.2 mg/m2 per day in children with and without nephrotic-range proteinuria, respectively. Seventeen patients were receiving prolonged therapy with prednisone at a low dose of 0.25–0.50 mg/kg body mass on alternate days, and two patients were still on pulse methylprednisolone and oral prednisolone at high doses at enrollment. Cyclosporine A treatment was given to 15 patients at a dose of 3–5 mg/kg per day. The mean cumulative doses of prednisolone and cyclosporine A were 1,450 ± 853 and 3,448 ± 2,344 mg/kg, respectively. None of the patients were treated with monoclonal antibodies. Twenty-six of the patients were on an ACEI, and 12 of these were on both ACEIs and ARBs.
The mean levels of serum glucose, serum insulin, and HOMA-IR did not differ between the patients and the controls (Table 1). None of the patients were insulin resistant as assessed by HOMA-IR. Twenty of the patients (54 %) had a total cholesterol of >200 mg/dl. Serum concentrations of HDL-C were <35 mg/dl in four patients (11 %), and LDL-C levels were >130 mg/dl in 16 patients (43 %). Statins were prescribed to 15 patients.
Ambulatory blood pressure monitoring findings
All patients were subjected to ambulatory blood pressure monitoring (ABPM), and the results, including mean BP, BP indexes, SDS, and loads, are shown in Table 2. The mean indexes and SDS of 24-h MAP were 0.92 ± 0.07 and 0.42 ± 1.15, respectively; five patients showed a 24-h MAP that was >95th percentile for both sex and height.
As shown in Table 2, the mean BP indexes, SDS, and BP loads during nighttime were significantly higher than those during daytime (p < 0.001 for all). The nocturnal decline in SBP and DBP was 7.3 ± 5.3 and 11.6 ± 7.2 %, respectively. Nocturnal dipping was absent in 25 of 37 patients (68 %), of whom 14 were nondippers for both SBP and BP, and the remaining patients were nondippers only for SBP.
Subclinical CVD
The aortic PWV, carotid artery IMT, and LVM index were evaluated in all patients and compared to the healthy controls. As shown in Table 3, patients had a significantly higher mean aortic PWV (5.35 ± 0.65 vs. 4.81 ± 0.44 m/s; p = 0.001) and aortic PWV-SDS (0.64 ± 0.88 vs. −0.35 ± 0.51; p < 0.001) than controls. Of the 37 patients, two (5 %) had an increased aortic PWV-SDS. The mean carotid IMT was higher in patients (0.44 ± 0.02 mm) than in controls (0.39 ± 0.03 mm; p < 0.001), as was the mean carotid IMT-SDS (1.44 ± 0.67 vs. 0.45 ± 0.53, respectively; p < 0.001). Eight patients (22 %) had an increased carotid IMT-SDS. No plaque was detected in the carotid arteries. The mean LVM index was 35.3 ± 12.7 in patients and 26.3 ± 5.32 in controls (p < 0.001). LVH was present in seven patients (19 %) according to the age-specific 95th percentile for indexed LVM index in children and adolescents [25].
Risk factors for CVD
All clinical, laboratory and ABPM findings were analyzed to determine the factors influencing cardiovascular markers (aortic PWV-SDS, carotid IMT-SDS, and LVM index) and the potential predictors of subclinical CVD disease. None of these cardiovascular markers differed between male and female patients or between the patients receiving and not receiving ACEI/ARB or statins.
The mean PWV-SDS was found to be positively correlated with the 24-h SBP-SDS (r = 0.393, p = 0.016) and serum ferritin (r = 0.491, p = 0.009) and triglyceride levels (r = 0.357, p = 0.030), and inversely correlated with eGFR (r = -0.372, p = 0.023). Increased PWV was independently associated only with high serum ferritin level in a stepwise model of the multivariate linear regression analysis adjusted by SBP-SDS, triglyceride levels, and eGFR (R 2 = 0.269, β = 0.518, p = 0.006).
The mean carotid IMT-SDS was positively correlated with mean urinary protein excretion (r = 0.375, p = 0.022) and cumulative glucocorticoid exposure (r = 0.334, p = 0.043), and inversely correlated with serum albumin levels (r = −0.333, p = 0.044). Increased carotid IMT was independently associated only with high urinary protein excretion in a stepwise model multivariate regression analysis (R 2 = 0.141, β = 0.375, p = 0.022).
Univariate analysis also showed that there was a significant correlation between the LVM index and BMI-SDS (r = 0.486, p = 0.002) and 24-h SBP-SDS (r = 0.391, p = 0.017), but not with any laboratory variables. In a stepwise model multivariate regression analysis, the LVM index was found to be independently associated only with high BMI-SDS (R 2 = 0.317, β = 0.563, p < 0.001).
Multiple subclinical CVD
The patient with multiple subclinical CVD markers was defined as having at least two abnormal surrogate subclinical cardiovascular markers (an increased PWV-SDS, carotid IMT-SDS, LVM index, and/or 24-h MAP-SDS). Six patients (16 %) had multiple abnormal cardiovascular markers, including four patients with an increased carotid IMT and LVM index, one patient with an increased carotid IMT and 24-h MAP-SDS, and one patient with an increased aortic PWV-SDS and 24-h MAP-SDS.
To compare risk factors for multiple subclinical CVD, all of the clinical and laboratory parameters were separately evaluated (Table 4). The use of statins, but not ACEIs/ARBs, was significantly more prevalent in patients with multiple subclinical CVD as compared to their counterparts. The patients with multiple subclinical CVD had significantly higher cumulative urinary protein excretion and LDL-C than those without (Table 4). A logistic regression analysis revealed that the presence of multiple subclinical CVD was independently associated only with higher LDL-C (R 2 = 0.292, β = 1.019, p = 0.044).
Discussion
The results of this study provide evidence for the presence of early vascular and cardiac changes in children with SRNS. Our findings also reveal the presence of both functional and structural abnormalities of the arteries in these children, including increased arterial stiffness and increased carotid IMT.
It has been widely recognized that aortic PWV is a sensitive marker of arterial stiffness and, consequently, of cardiovascular outcome [26]. Although previous studies have demonstrated impaired endothelial function in adult [27] and pediatric [28] nephrotic patients, aortic stiffness has not been sufficiently examined in these patients. Our study demonstrates, for the first time, that children with SRNS have increased arterial stiffness. It is also important to note that our results show a significant association between increased arterial stiffness and serum ferritin level in SRNS. In proteinuric states, we suggest that there is the probability that the ability of ferritin to act as an inflammatory and/or oxidative factor could lead to vessel wall changes by favoring the formation of pro-atherogenic oxidized LDL [29]. Previous studies have demonstrated oxidative stress and inflammation in children with idiopathic nephrotic syndrome [30–32], and also that these changes are more marked in patients with SRNS than in those with steroid-sensitive NS [32–34].
Earlier studies have identified the various metabolic risk factors that contribute to atherosclerosis in NS [35, 36]. In our patient cohort, LDL-C appears to be a potential risk factor for subclinical CVD. Nephrotic children may have prolonged periods of hyperlipidemia even after clinical remission and, therefore, some of these children with dyslipidemia may be at increased risk of developing premature atherosclerosis [4, 37]. Persistent proteinuria has also been described as an additional risk factor for CVD [38], and an association between carotid IMT and the number of recurrences has previously been reported in young patients formerly treated for idiopathic NS [4]. Our findings demonstrate that children with SRNS have significantly higher carotid IMT as predicted by high amounts of urinary protein excretion. Since limited data on increased carotid IMT are available for children currently being treated for steroid-resistant and -dependent NS [39], our results may indicate an increased risk of vascular disease and may point out its association with urinary protein excretion in children with SRNS. Our findings therefore support the hypothesis that the increasing severity of atherosclerosis is not only related to the presence or extent of metabolic cardiovascular risk factors but also to the persistence of risk factors over time.
Systolic hypertension is considered to be a definite risk factor for kidney injury and CVD. Therefore, evaluation of BP status and its association with CVD was another important focus of this study. The most obvious ABPM finding was that our patients had a predominantly higher nocturnal BP with a high prevalence of the nondipping pattern. Blunted nocturnal dipping is a prognostic risk factor for unfavorable cardiovascular outcome in the general population [40], and there is also a link between the loss of reduction in nighttime BP and excessive target organ damage [41]. An abnormal BP pattern has previously been described in children with chronic kidney disease [42]. In addition, in our patient cohort, higher 24-h SBP-SDS was significantly, but not independently associated with an increased PWV-SDS and LVM index. However, at enrollment, the majority of our patients were receiving ACEIs and/or ARBs, and statins. Due to the use of these medications in our patients, which are especially widely used in children with nephrotic-range proteinuria and hypoalbuminemia, it is not possible to rule out their possible effects on the cardiovascular parameters. Furthermore, it can be speculated that the use of ACEIs/ARBs and statins might have a potentially protective effect on the development of atherosclerosis, possibly due to their renoprotective and pleiotrophic effects in our study population.
In our study cohort, patients had higher LVM index values than the controls, and seven patients had LVH. Our results suggest that BMI-SDS was the only independent risk factor for LVH. It is well known that high-dose and long-term glucocorticoid exposure induce increases in BMI z-scores, hypertension, and dyslipidemia, all of which are acknowledged risk factors for CVD [43, 44]. However, our study failed to demonstrate a correlation between glucocorticoid exposure and both BMI and hypertension. Indeed, a child with a high total lifetime glucocorticoid exposure may have lost weight while being maintained on small doses of glucocorticoids for several years [45]. The BMI of our patients were in the range of 21.9 ± 5.5, and 17 of 19 patients were on low-dose glucocorticoid treatment at enrollment. Also, genetic factors and familial environment may predispose children to weight gain during glucocorticoid exposure [45, 46]. Furthermore, LVH may be prevalent even at the time of diagnosis among children with SRNS as a result of mutations in podocin [47].
Several limitations of this study must be taken into consideration when interpreting the data. Firstly, our study had a cross-sectional design and was limited by the small sample size, which may affect the validity of the multivariate analyses. In addition, the use of immunosuppressive and antihypertensive drugs could result in major confounding effects on the surrogate vascular endpoints. Therefore, the study did not allow us to determine causality. Secondly, although many potential confounding factors have been assessed, the existence of unexamined variables, such as oxidative stress [31], genetics [47], and dietary habits [48], should be noted.
In conclusion, SRNS children generally have a high risk of cardiovascular complications. However, SRNS is most probably associated with complex pathophysiological changes for CVD, and the process of CVD development is likely to be multifactorial, and not solely related to augmented traditional risk factors. Therefore, prospective longitudinal studies in larger cohorts are required to further identify the impact of each risk factor on CVD.
References
Ordonez JD, Hiatt RA, Killebrew EJ, Fireman BH (1992) The increased risk of coronary heart disease associated with the nephrotic syndrome. Kidney Int 44:638–642
Adedoyin O, Frank R, Vento S, Vergara M, Gauthier B, Trachtman H (2004) Cardiac disease in children with primary glomerular disorders role of focal segmental glomerulosclerosis. Pediatr Nephrol 19:408–412
Lechner BL, Bockenhauer D, Iragorri S, Kennedy TL, Siegel NJ (2004) The risk of cardiovascular disease in adults who have had childhood nephrotic syndrome. Pediatr Nephrol 19:744–748
Kniażewska MH, Obuchowicz AK, Wielkoszyński T, Żmudzińska-Kitczak J, Urban K, Marek M, Witanowska J, Sieroń-Stołtny K (2009) Atherosclerosis risk factors in young patients formerly treated for idiopathic nephrotic syndrome. Pediatr Nephrol 24:549–554
Eddy AA, Symons JM (2003) Nephrotic syndrome in childhood. Lancet 362:629–639
Querfeld U (1999) Should hyperlipidemia in children with nephrotic syndrome be treated? Pediatr Nephrol 13:77–84
Chan DT, Irish AB, Dogra GK, Watts GF (2008) Dyslipidaemia and cardiorenal disease: mechanisms, therapeutic opportunities and clinical trials. Atherosclerosis 196:823–834
Litwin M, Niemirska A (2009) Intima-media thickness measurements in children with cardiovascular risk factors. Pediatr Nephrol 24:707–719
Tomiyama H, Yamashina A (2010) Non-invasive vascular function tests: their pathophysiological background and clinical application. Circ J 74:24–33
Schwartz GJ, Gauthier B (1985) A simple estimate of glomerular filtration rate in adolescent boys. J Pediatr 106:522–526
International Study of Kidney Disease in Children (1981) The primary nephrotic syndrome in children. Identification of patients with minimal change nephrotic syndrome for initial response to prednisone. J Pediatr 98:561–564
Neyzi O, Furman A, Bundak R, Gunoz H, Darendeliler F, Bas F (2006) Growth references for Turkish children aged 6 to 18 years. Acta Pediatr 95:1635–1641
Bundak R, Furman A, Gunoz H, Darendeliler F, Bas F, Neyzi O (2006) Body mass index references for Turkish children. Acta Pediatr 95:194–198
Matsumoto K, Miyake S, Yano M, Ueki Y, Yamaguchi Y, Akazawa S, Tominaga Y (1997) Glucose tolerance, insulin secretion, and insulin sensitivity in nonobese and obese Japanese subjects. Diabetes Care 20:1562–1568
D’Annunzio G, Vanelli M, Pistorio A, Minuto N, Bergamino L, Iafusco D, Lorini R, the Diabetes Study Group of the Italian Society for Pediatric Endocrinology and Diabetes (ISPED) (2009) Insulin resistance and secretion indexes in healthy Italian children and adolescents: a multicenter study. Acta Biomed 80:21–28
Soergel M, Kirschstein M, Busch C, Danne T, Gellermann JJ, Holl R, Krull F, Reichert H, Reusz GS, Rascher W (1997) Oscillometric twenty-four-hour ambulatory blood pressure values in healthy children and adolescents: a multicenter trial including 1141 subjects. J Pediatr 130:178–184
Wuhl E, Witte K, Soergel M, Mehls O, Schaefer F, Germany Working Group on Pediatric Hypertension (2002) Distribution of 24-h ambulatory blood pressure in children: normalized reference values and role of body dimensions. J Hypertens 20:1995–2007
Kracht D, Shroff R, Baig S, Doyon A, Jacobi C, Zeller R, Querfeld U, Schaefer F, Wühl E, Schmidt BM, Melk A, 4C Study Consortium (2011) Validating a new oscillometric device for aortic pulse wave velocity measurements in children and adolescents. Am J Hypertens 24:1294–1299
Reusz GS, Cseprekal O, Temmar M, Kis E, Cherif AB, Thaleb A, Fekete A, Szabó AJ, Benetos A, Salvi P (2010) Reference values of pulse wave velocity in healthy children and teenagers. Hypertension 56:217–224
Stein JH, Korcarz CE, Hurst RT, Lonn E, Kendall CB, Mohler ER, Najjar SS, Rembold CM, Post WS, American Society of Echocardiography Carotid Intima-Media Thickness Task Force (2008) Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American Society of Echocardiography Carotid Intima-Media Thickness Task Force. Endorsed by the Society for Vascular Medicine. J Am Soc Echocardiogr 21:93–111
Jourdan C, Wühl E, Litwin M, Fahr K, Trelewicz J, Jobs K, Schenk JP, Grenda R, Mehls O, Tröger J, Schaefer F (2005) Normative values for intima-media thickness and distensibility of large arteries in healthy adolescents. J Hypertens 23:1707–1715
Sahn DJ, De Maria A, Kisslo J, Weyman A (1978) Recommendations regarding quantification in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation 58:1072–1083
Devereux RB, Reichek N (1977) Echocardiographic determination of left ventricular mass in man: anatomic validation of the method. Circulation 55:613–618
De Simone G, Daniels SR, Devereux RB, Meyer RA, Roman MJ, de Diviitis O, Alderman MH (1992) Left ventricular mass and body size in normotensive children and adults: assessment of allometric relations and impact of overweight. J Am Coll Cardiol 20:1251–1260
Khoury PR, Mitsnefes M, Daniels SR, Kimball TR (2009) Age specific reference intervals for indexed left ventricular mass in children. J Am Soc Echocardiogr 22:709–714
Khosdel AR, Carney SL, Nair BR, Gillies A (2007) Better management of cardiovascular diseases by pulse wave velocity: combining clinical practice with clinical research using evidenced based medicine. Clin Med Res 5:45–52
Dogra GK, Watts GF, Herrmann S, Thomas MAB, Irish AB (2002) Statin therapy improves brachial artery endothelial function in nephrotic syndrome. Kidney Int 62:550–557
Tkaczyk M, Czupryniak A, Owczarek D, Lukamowicz J, Nowicki M (2008) Markers of endothelial dysfunction in children with idiopathic nephrotic syndrome. Am J Nephrol 28:197–202
Agarwal R (2008) Iron, oxidative stress, and clinical outcomes. Pediatr Nephrol 23:1195–1199
Kamireddy R, Kavuri S, Devi S, Vemula H, Chandana D, Harinarayanan S, James R, Rao A (2002) Oxidative stress in pediatric nephrotic syndrome. Clin Chim Acta 325:147–150
Mishra OP, Gupta AK, Prasad R, Ali Z, Upadhyay RS, Mishra SP, Tiwary NK, Schaefer FS (2011) Antioxidant status of children with idiopathic nephrotic syndrome. Pediatr Nephrol 26:251–256
Wasilewska A, Zoch-Zwierz W, Tobolczyk J, Tenderenda E (2007) High-sensitivity C-reactive protein (hs-CRP) level in children with nephrotic syndrome. Pediatr Nephrol 22:403–408
Kuo HT, Kuo MC, Chiu YW, Chang YW, Guh JY, Chen HC (2005) Increased glomerular and extracellular malondialdehyde levels in patients and rats with focal segmental glomerulosclerosis. Eur J Clin Invest 35:245–250
Bakr A, Hassan SA, Shoker M, Zaki M, Hassan R (2009) Oxidant stress in primary nephrotic syndrome: does it modulate the response to corticosteroids? Pediatr Nephrol 24:2375–2380
Jin J, Jin B, Huang S, Yuan Y, Ding D, Bao H, Chen Y, Han Y, Zhao F, Zhang A (2012) Insulin resistance in children with primary nephrotic syndrome and normal renal function. Pediatr Nephrol 27:1901–1909
Dogra GK, Herrmann S, Irish AB, Thomas MAB, Watts GF (2002) Insulin resistance, dyslipidaemia, inflammation and endothelial function in nephrotic syndrome. Nephrol Dial Transplant 17:2220–2225
Zilleruelo G, Hsia SL, Freundlich M, Gorman HM, Strauss J (1984) Persistence of serum lipid abnormalities in children with idiopathic nephrotic syndrome. J Pediatr 104:61–64
Grimm RH, Svendsen KH, Kasiske B, Keane WF, Wahi MM (1997) Proteinuria is a risk factor for mortality over 10 years of follow-up: MRFIT Research Group, Multiple Risk Factor Intervention Trial. Kidney Int 63:S10–S14
Książek J, Niemirska A, Lipka M, Grenda R (2006) Evaluation of arterial intima-media thickness (IMT) in children with idiopathic nephrotic syndrome—preliminary report. Przegl Lek 63[Suppl 3]:205–207
Ohkubo T, HozawaA YJ, Kikuya M, Ohmori K, Michimata M, Matsubara M, Hashimoto J, Hoshi H, Araki T, Tsuji I, Satoh H, Hisamichi S, Imai Y (2002) Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama study. J Hypertens 20:2183–2189
Routledge FS, McFetridge-Durdle JA, Dean CR, Canadian Hypertension Society (2007) Night-time blood pressure patterns and target organ damage: a review. Can J Cardiol 23:132–138
Mitsnefes M, Flynn J, Cohn S, Samuels J, Blydt-Hansen T, Saland J, Kimball T, Furth S, Warady B, CiKD Study Group (2010) Masked hypertension associates with left ventricular hypertrophy in children with CKD. J Am Soc Nephrol 21:137–144
Nakamura A, Niimi R, Kurosaki K, Yanagawa Y (2010) Factors influencing cardiovascular risk following termination of glucocorticoid therapy for nephrotic syndrome. Clin Exp Nephrol 14:457–462
Fardet L (2013) Metabolic and cardiovascular adverse events of systemic glucocorticoid therapy. Rev Med Interne 34:303–309
Foster BJ, Shults J, Zemel BS, Leonard MB (2006) Risk factors for glucocorticoid-induced obesity in children with steroid-sensitive nephrotic syndrome. Pediatr Nephrol 21:973–980
Wisniewski AB, Chernausek SD (2009) Gender in childhood obesity: family environment, hormones, and genes. Gend Med 6[Suppl 1]:76–85
Frishberg Y, Feinstein S, Rinat C, Becker-Cohen R, Lerer I, Raas-Rothschild A, Ferber B, Nir A (2006) The heart of children with steroid-resistant nephrotic syndrome: is it all podocin? J Am Soc Nephrol 17:227–231
Koeth RA, Wang Z, Levison BS, Buffa JA, Org E, Sheehy BT, Britt EB, Fu X, Wu Y, Li L, Smith JD, Didonato JA, Chen J, Li H, Wu GD, Lewis JD, Warrier M, Brown JM, Krauss RM, Tang WH, Bushman FD, Lusis AJ, Hazen SL (2013) Intestinal microbiota metabolism of l-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat Med 19:576–585
Disclosure
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Candan, C., Canpolat, N., Gökalp, S. et al. Subclinical cardiovascular disease and its association with risk factors in children with steroid-resistant nephrotic syndrome. Pediatr Nephrol 29, 95–102 (2014). https://doi.org/10.1007/s00467-013-2608-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-013-2608-3