Abstract
Background
It has been suggested that C1q and immunoglobulin M (IgM) nephropathy are variants of minimal change nephrotic syndrome (MCNS). Many researchers believe that these two conditions signify a worse prognosis for children with MCNS in comparison with immunofluorescence (IF)-negative MCNS. The aim of our study was to determine the prognostic significance of C1q nephropathy and IgM nephropathy in children with MCNS.
Methods
Fifty-five children with MCNS who had been biopsied over the course of 24 years at our institution were retrospectively categorized into three groups on the basis of IF microscopy findings: IF-negative MCNS (29/55 patients), MCNS with IgM nephropathy (19/55 patients), and MCNS with C1q nephropathy (7/55 patients). Clinical characteristics at disease presentation, clinical course, and renal outcome were compared between groups during the median follow-up period of 16.9 years (minimum 1.0, maximum 31.1 years).
Results
No statistically significant differences in clinical characteristics at disease presentation, clinical course, and renal outcome were found. Children with IgM nephropathy, C1q nephropathy, and IF-negative MCNS were clinically indistinguishable.
Conclusions
We concluded that C1q or IgM nephropathy variants do not seem to signify a worse prognosis in children with MCNS in comparison with IF-negative MCNS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nephrotic syndrome (NS) is a constellation of clinical and laboratory findings that result from renal protein loss. It is classically defined by nephrotic range proteinuria, hypoalbuminemia, edema, and hyperlipidemia, where the first two criteria are generally used for clinical diagnosis. NS is thus not a disease in itself, but rather a manifestation of many different glomerular diseases that bear in common an increased permeability of the glomerular filtration barrier.
The most common form of NS in children is primary NS, where kidney involvement is the main sign of the disease. Primary NS accounts for approximately 90 % of NS in children, while secondary NS, where kidney involvement is only a part of the systemic disease, accounts for the remaining 10 % [1]. Renal biopsy is required to elucidate the exact glomerular disease that causes the NS. Glomerulopathy with minimal changes is the commonest cause of primary NS in children, occurring in about 75 % of patients [2], and is referred to as minimal change nephrotic syndrome (MCNS). In comparison, the frequency of other pathohistological forms of primary NS in children, such as focal segmental glomerulosclerosis (FSGS) and membranous glomerulopathy is much lower [3].
In MCNS, the immunofluorescence (IF) analysis may be negative or it may reveal the characteristic features of immunoglobulin M (IgM) or C1q nephropathy. IgM nephropathy was described in 1978 as a glomerulopathy with diffuse IgM glomerular mesangial immune deposits showing a variable degree of mesangial hypercellularity [4, 5]. C1q nephropathy, on the other hand, was described in 1985 by Jennette and Hipp as a glomerulopathy with prominent C1q glomerular immune deposits with no evidence of systemic lupus erythematosus (SLE) and no histological criteria for type I membranoproliferative glomerulonephritis [6, 7]. More recently, modified criteria have been proposed for a diagnosis of C1q nephropathy in patients without evidence of SLE; these include a grade of ≥2+ (on a scale of 0–4+) immunostaining for C1q with a predominantly mesangial distribution, frequently accompanied by IgG and IgM, which may be less intense, equally intense or more intense [8, 9].
There is profound variability in histology and clinical presentation in both C1q nephropathy and IgM nephropathy. Both disorders are often associated with MCNS, FSGS, and NS, and are, accordingly, suggested as being variants of MCNS [10]. C1q nephropathy and IgM nephropathy can also present as isolated hematuria, non-nephrotic proteinuria, nephritic syndrome and asymptomatic urinary abnormalities, and have even been found in a few healthy individuals [9, 11–14].
A review of literature revealed that studies comparing patients with C1q or IgM nephropathy to patients with IF-negative MCNS are scarce [15–19]. In most studies dealing with C1q nephropathy and IgM nephropathy in children, the number of participating patients was relatively small, and the follow-up period was relatively short [11, 18–22]. These studies included children with various histological variants of C1q nephropathy, and IgM nephropathy, and the results showed that they were often associated with frequently relapsing, steroid-dependent and steroid-resistant NS and therefore might carry the risk of an unfavorable long-term prognosis [11, 18–22]. Nevertheless, the evidence for this is not unequivocal, as some researchers have reported obtaining the opposite results [16, 17, 23]. The limited indications for renal biopsy and the relatively low incidence of C1q and IgM nephropathy in children with NS make it difficult for researchers in this field to come to meaningful conclusions in terms of the prognostic significance of these two conditions. The questions which remain to be answered are whether C1q or IgM nephropathy in children with MCNS are truly the markers of disease severity, the markers that will guide the clinician to a more aggressive therapeutic approach, and the markers which will facilitate prognosis.
The aim of our study was to determine the prognostic significance of C1q and IgM nephropathy in childhood MCNS. To this end, we compared three groups of children with MCNS, namely, those with no deposits, those with IgM nephropathy, and those with C1q nephropathy, for clinical characteristics at disease presentation, clinical course, and outcome of MCNS.
Methods
Renal biopsies and patient selection
This was a retrospective study in which the results of 6,240 renal biopsies analyzed at the Institute of Pathology, Faculty of Medicine, University of Ljubljana, Slovenia in the period 1984–2008 were reviewed.
There is as yet no universal consensus on the indications for renal biopsy in children with NS although these have become more specific in recent years. Nowadays, most physicians would agree on the following criteria: age of <1 year or >10 years, arterial hypertension and/or hematuria and/or decreased glomerular filtration rate (GFR) and/or extra-renal manifestations that could indicate a systemic disease, and frequently relapsing, steroid-dependent or steroid-resistant NS. Our patients satisfied these criteria, with two exceptions (non-concordance of clinical picture with supposedly mild, non-nephrotic proteinuria in one child, and age of 8 years at the time of biopsy in another).
The indications for follow-up biopsy in children with NS are even less well-defined, but most physicians would agree on the following, which were also used in our patients: change in response to steroid therapy, drug nephrotoxicity during follow-up, appearance of arterial hypertension and/or hematuria and/or decreased GFR and/or extra-renal manifestations that could indicate a systemic disease.
In accordance with the definitions described in detail in Appendix 1, 59 children treated at the University Children’s Hospital of the University Medical Centre Ljubljana, Slovenia from 1 January 1984 to 1 April 2012 (28 years) were identified as having MCNS at the time of their initial renal biopsy. Of these 59 patients, four were excluded from further analysis (no glomeruli for IF analysis in 2 patients; full medical records were unavailable for 2 patients).
The renal tissue obtained by initial percutaneous needle biopsy was divided into three portions. All biopsies (n = 55 patients) were processed for study by light and IF microscopy, and 30 biopsies were processed for viewing under the electron microscope according to standard techniques. For light microscopy, the renal tissue samples were fixed in buffered 4 % formaldehyde, embedded in Paraplast, and stained with hematoxylin and eosin, Masson trichrome, periodic acid–Schiff, periodic acid silver methenamine/Azan, and van Gieson–Weigert’s stains. For IF microscopy, the kidney samples were frozen in liquid nitrogen, and cryostat sections were stained with fluorescein isothyocianate-labeled antisera to human IgA, IgG, IgM, kappa and lambda light chains, C3, C1q, C4, fibrin/fibrinogen, and albumin (Dakopatts, Copenhagen, Denmark). The tissue for electron microscopy was fixed in buffered 1 % osmium tetroxide and embedded in Epon. Ultrathin sections were contrasted with uranyl acetate and lead citrate prior to analysis.
C1q nephropathy was defined as grade ≥2+ (on a scale of 0–4+) immunostaining for C1q with a predominantly mesangial distribution, frequently accompanied by IgG and IgM, which may be less intense, equally intense, or more intense, in patients without evidence of SLE. IgM nephropathy was defined as grade ≥2+ (on a scale of 0–4+), indicating dominant immunostaining for IgM predominantly in the mesangium. The exceptions were patients who had in addition to IgM, C1q staining grade ≥2+; these patients were included in the C1q nephropathy group. Accordingly, patients were categorized into three groups: IF-negative MCNS patients, IgM nephropathy MCNS patients, and C1q nephropathy MCNS patients.
Biopsy follow-up was available for 15 patients, who underwent 21 repeat renal biopsies.
Patients’ charts were reviewed retrospectively for presentation of the disease, histopathology findings, clinical course, methods of treatment, and outcome. Due to the retrospective nature of our study, the data on some of the analyzed parameters were not available for all patients.
The definitions used for disease presentation, clinical course, response to treatment, and renal outcome are described in detail in Appendices 2–4, respectively.
Collection and review of patient data were approved by the National Medical Ethics Committee of the Republic of Slovenia.
Statistical analysis
As patient age revealed a bimodal distribution and other numerical variables showed an asymmetrical distribution, we generally present the data as the median, with data variability presented as the first and third quartile. Categorical data are expressed as proportions. The differences in medians between patient groups were assessed using the Kruskal–Wallis test and the Mann–Whitney test. For post-hoc paired comparisons, a correction of type I error was made using the Keppel modification of Bonferroni correction. The differences between observed and expected frequencies were tested using Pearson’s chi-square test or the Fisher exact test, as appropriate. A p value of <0.05 was considered to be statistically significant. Statistical analysis was performed with the R language for statistical computing [24].
Results
Renal biopsies and patients
Among the 55 children with MCNS, 31 were boys and 24 were girls, and all were Caucasian. At the time of disease presentation, they ranged in age from 1.3 to 17.8 (median 4.8) years. Initial renal biopsies were performed 0.02–13.74 years after the onset of the disease.
Based on IF microscopy findings, the patients were categorized into three groups: IF-negative MCNS (29/55; 53 %), MCNS with IgM nephropathy (19/55; 34 %), and MCNS with C1q nephropathy (7/55; 13 %). The finding of diffuse mesangial hypercellularity did not differ significantly among the three groups and was found in three (3/29; 10 %) of the patients with IF-negative MCNS, two (2/19; 11 %) of the patients with MCNS with IgM nephropathy, and one (1/7; 14 %) patient with MCNS with C1q nephropathy (p = 1).
In patients with C1q nephropathy, electron-dense deposits were seen in six of the six electron microscopy examinations available for study; in patients with IgM nephropathy these deposits were seen in five of the 13 electron microscopy examinations available for study. In all cases, the deposits were mesangial in distribution, and in one patient with C1q nephropathy they were also subendothelial. Podocyte foot process effacement was present in 27 of the 30 cases: in 11 patients with IgM nephropathy, six patients with C1q nephropathy, and ten patients with IF-negative MCNS. Podocyte foot process effacement was segmental (<50 %) in nine cases and diffuse (≥50 %) in 18 cases.
Demographic data and clinical presentation
Demographic data and clinical presentations did not differ significantly between the groups (Table 1).
Clinical course of the disease and response to treatment
The characteristics of the clinical course of the disease are presented in Table 2. It should be noted that conclusions are based on relatively low statistical power, which is presented in brackets for each parameter. No statistical significance was shown between the three groups as regards the proportion of patients who were infrequently relapsing, frequently relapsing, steroid dependent or steroid resistant (p = 0.98; power 0.32).
Of the 55 patients, nine (16 %) were initially steroid resistant, of whom one (1/7; 14 %) had C1q nephropathy, three (3/19; 16 %) had IgM nephropathy, and five (5/29; 17 %) had IF-negative MCNS. Of the 55 patients, 46 (84 %) were initially steroid sensitive, among whom no statistically significant difference as regards time to achieve first remission was found (p = 0.55; power 0.42). Relapses occurred in 41 of the 46 (89 %) initial responders. There were no significant differences between groups in terms of relapse rate per year of follow-up, hematuria, hypertension, and angiotensin converting enzyme (ACE) inhibition later in the course of the disease (p = 0.72, p = 0.83, p = 1, p = 1, respectively; power 0.11, 0.33, 0.05, 0.06, respectively).
The proportion of patients who received adjuvant immunosuppressive therapy did not differ statistically between the groups (p = 0.75; power 0.06), but was highest in the C1q nephropathy group (86 % in C1q nephropathy group, 68 % in IgM nephropathy group, 76 % in IF-negative group). The median of relapse-free survival time after initiation of the first-choice immunosuppressive agent was longest in the C1q nephropathy group and shortest in the IgM nephropathy group, but the differences between groups for this parameter were not statistically significant (p = 0.785; power 0.41).
There was no significant difference in the number of different adjuvant therapies used per patient during follow-up between the groups (p = 0.848; power 0.05).
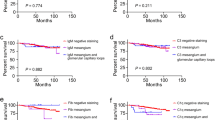
Outcome of the disease
The outcome parameters were evaluated during the last follow-up visit and are presented in Table 3. No statistically significant differences in renal outcome were found between the IgM nephropathy, C1q nephropathy and IF-negative MCNS groups (p = 0.674). It should be noted that this conclusion is based on a relatively low statistical power of 0.29.
The patients were followed for a median of 16.9 years (minimum 1.0, maximum 31.1 years). Follow-up was the shortest in C1q nephropathy patients (median 5.9 years) due to the emigration of two patients shortly (12 months) after renal biopsy and the death of one patient 2 years after disease presentation. Consequently, C1q nephropathy patients were also the youngest at the end of follow-up (median 9.6 years).
Twenty-one follow-up renal biopsies were performed in 15 patients 0.2–13.5 years after the initial biopsy. Morphological transition to FSGS was observed in a similar proportion in all three groups of patients, being present in one of four (25 %) patients in the C1q nephropathy group, one of three (33 %) in the IgM nephropathy group, and in three of eight patients (38 %) in the IF-negative group.
In the 46 patients who were steroid sensitive, all but one were in complete remission at last follow-up. The one exception had IF-negative MCNS and was initially steroid dependent, but progressed to end-stage renal disease (ESRD) at the age of 10.6 years. The reason for such an outcome was believed to be non-compliance with therapy.
In the nine patients who were steroid resistant, three were in complete remission, two in partial remission, one had no remission but stable renal function, one had no remission and progression of renal disease, and two had progressed to ESRD at last follow-up. In both patients who progressed to ESRD, a follow-up renal biopsy revealed FSGS; the initial biopsy had revealed MCNS with C1q nephropathy in one patient and IF-negative MCNS in the second patient. The first patient was resistant to all therapy and died 2 years after disease presentation due to ESRD complications. The second patient progressed to ESRD 4.5 years after the initial diagnosis despite various second-line immunosuppressive therapies and has since received a transplant.
Discussion
The standard practice in children with NS is that only those with an unfavorable clinical course comprising steroid dependency, frequently relapsing disease, or steroid resistance are biopsied [25–27]. Accordingly, it is impossible to estimate the real prevalence of C1q and IgM nephropathy in children with NS and, consequently, research in this field is difficult and subject to selection bias.
On the basis of our clinical impressions and data retrieved from the literature, it would appear that C1q and IgM nephropathy variants of MCNS are more often associated with frequently relapsing, steroid-dependent, or steroid-resistant NS, and as such might bear the risk of a more unfavorable clinical course and long-term prognosis when compared to the IF-negative variant of MCNS. However, the evidence for this in the literature is equivocal [11, 15–23] and we therefore conducted a retrospective study comparing the presentation, clinical course, and outcome of IF-negative MCNS patients to patients with C1q/IgM nephropathy variants of MCNS. Since we followed many children into adulthood, the follow-up period in our study is the longest to be published to date for children with IgM nephropathy and one of the longest for children with C1q nephropathy.
Our comparison of 55 children with MCNS who had been biopsied over a period of 24 years at our institution revealed no statistically significant differences in the features of clinical characteristics at disease presentation, clinical course, and renal outcome between the groups (IgM, C1q, and IF-negative MCNS). It should be noted, however, that the number of patients included in our study, as well as in other studies, was far lower than that needed to reach statistically significant and sufficiently powerful conclusions; consequently, the lack of any difference between the groups may simply be caused by the small number of patients in each group. IgM nephropathy and C1q nephropathy were clinically indistinguishable in our children with MCNS. As regards the finding of diffuse mesangial hypercellularity, which according to some authors might predict a worse clinical course and outcome [26, 28, 29], no differences were found between the groups in our cohort. The findings of our study imply that the presence of C1q or IgM nephropathy, regardless of mesangial hypercellularity, does not signify a poorer prognosis in children with MCNS as compared to children with IF-negative MCNS. Silverstein et al. [30] have even suggested that mesangial hypercellularity predicts a more favorable prognosis.
Few studies have compared the clinical course and renal outcome in children with the IgM nephropathy variant of MCNS to IF-negative MCNS [16–19], and only one previous study has compared the clinical course and renal outcome in children with the C1q nephropathy variant of MCNS to IF-negative MCNS [15]. In this latter study, Wong et al. compared nine children with C1q nephropathy MCNS and 16 children with IF-negative MCNS and found no significant differences in the features of clinical characteristics at disease presentation, clinical course (relapse frequency during follow-up, time to first remission, and time to first relapse), and renal outcome between the two groups [15]; these results are in agreement with our results. The proportion of patients who received adjuvant immunosuppressive therapy in our study did not differ statistically between the groups, but was the highest in the C1q nephropathy group (86 %). Wong et al. [15] reported a similar finding, with all children with C1q nephropathy needing chronic immunosuppression with calcineurin inhibitors and/or mycophenolate mofetil to maintain remission, whereas IF-negative MCNS patients did not. In contrast to Wong et al.’s [15] cohort, all but one child in our cohort were in complete remission without chronic immunosuppressive therapy at the end of the follow-up period. This discrepancy between our cohort and Wong’s cohort could be attributed to the use of different immunosuppressive agents, as the majority of our patients received cyclophosphamide, whereas Wong et al.’s [15] patients received calcineurin inhibitors and/or mycophenolate mofetil. In addition, Wong’s patients were mostly Hispanic or African American, while ours were all Caucasian, and it is possible that demographic parameters (ethnicity) may also account for these differences. The relevance of such comparisons is, however, limited, since both C1q nephropathy cohorts comprised a small number of patients.
The studies that compared children with IgM nephropathy to IF-negative MCNS have provided conflicting results. Pardo et al. [16] and Al-Eisa et al. [17] reported findings which are in agreement with our results and concluded that these two conditions are clinically indistinguishable, while Zeis et al. [18], similar to Swartz et al. [20] showed a worse response to therapy and a worse outcome in patients with IgM nephropathy. In a recent study by Kanemoto et al., the outcome in children with IgM nephropathy was not statistically different from that of children with IF-negative NS, but a higher percentage of IgM nephropathy NS patients needed immunosuppressive agents at last follow-up visit [19]. Zeis et al. [18], like Swartz et al. [20] and Kanemoto et al. [19], included only patients with NS who were steroid dependent and steroid resistant, while Pardo et al. [16] and Al-Eisa et al. [17], like us, included patients with much broader clinical presentations of NS (infrequent relapsers, frequent relapsers, steroid-dependent and steroid-resistant patients), and their results are in line with those of our study. Zeis et al. [18] showed a higher frequency of morphological transitions to FSGS among children with IgM nephropathy MCNS as compared to children with IF-negative MCNS, whereas in our study the transition to FSGS was not significantly different between the groups.
The relationship between MCNS and FSGS remains controversial. Some researchers believe that MCNS may progress to FSGS with time, while others are of the opinion that these two conditions are two separate disorders and that the characteristic histopathological features of FSGS are missed in the initial biopsies of MCNS patients due to sampling error [31, 32]. Still others have proposed that C1q and IgM nephropathies are a transitional state between MCNS and FSGS [10, 33], a hypothesis which was not supported by the results of our study, where follow-up biopsies showed a similar proportion of transition to FSGS in IF-negative and IF-positive patients.
Progression to ESRD was a rare event in our patients with C1q or IgM nephropathy, which was not the case in Swartz et al.’s patient cohort [20]. These authors analyzed a group of 55 children with steroid-dependent and steroid-resistant NS and IgM nephropathy. Of these 55 patients, 23 had minimal change disease, with four of these 23 (17 %) ultimately progressing to chronic kidney disease and three (13 %) to ESRD. No comparison to IF-negative MCNS patients was made in this study, yet the outcome of IgM nephropathy MCNS patients was much worse than that in our cohort. The differences between our results and those reported by Swartz et al., Zeis et al., and Kanemoto et al. [18–20] might have been due to the different inclusion criteria used in each case.
In conclusion, the findings of our study suggest that C1q nephropathy and IgM nephropathy variants of MCNS, regardless of the presence or absence of mesangial hypercellularity, do not predict the disease course, are not more often associated with frequently relapsing, steroid-dependent, or steroid-resistant NS and therefore do not bear the risk of unfavorable clinical course and long-term prognosis in children with MCNS as compared to children with the IF-negative variant of MCNS. It should, however, be noted that these conclusions are based on relatively low statistical power. The number of patients included in our study, as well as in other studies, were far from that needed to reach statistically powerful enough conclusions; consequently, the lack of any difference between the groups may simply have been caused by the small number of patients in each group. Given the numerous drawbacks and limitations of our study and of previous retrospective studies, a prospective multi-center, randomized trial is needed to further clarify the prognostic significance of IgM nephropathy and C1q nephropathy variants in children with MCNS.
References
Churg J, Habib R, White RH (1970) Pathology of the nephrotic syndrome in children: a report for the International Study of Kidney Disease in Children. Lancet 760:1299–1302
[No authors listed] (1978) Nephrotic syndrome in children: prediction of histopathology from clinical and laboratory characteristics at time of diagnosis. A Report of the International Study of Kidney Disease in Children. Kidney Int 13:159–165
Eddy AA, Symons JM (2003) Nephrotic syndrome in childhood. Lancet 362:629–639
Bhasin HK, Abeulo JG, Nayak R, Esparza AR (1978) Mesangial proliferative glomerulonephritis. Lab Invest 39:21–29
Cohen AH, Border WA, Glassock RJ (1978) Nephrotic syndrome with glomerular mesangial IgM deposits. Lab Invest 38:610–619
Jennette JC, Hipp CG (1985) C1q nephropathy: a distinct pathologic entity usually causing nephrotic syndrome. Am J Kidney Dis 6:103–110
Jennette JC, Hipp CG (1985) Immunohistopathologic evaluation of C1q in 800 renal biopsy specimens. Am J Clin Pathol 83:415–420
Jennette JC, Falk RJ (2000) C1q nephropathy. In: Massry SG, Glassock R (eds) Textbook of nephrology, 4th edn. Lippincott-Williams & Wilkins, Philadelphia, pp 730–733
Vizjak A, Ferluga D, Rožič M, Hvala A, Lindič J, Levart TK, Jurčić V, Jennette JC (2008) Pathology, clinical presentations, and outcomes of C1q nephropathy. J Am Soc Nephrol 19:2237–2244
Fogo AB (2001) Minimal change disease and focal segmental glomerulosclerosis. Nephrol Dial Transplant 16[Suppl 6]:74–76
Kersnik Levart T, Kenda RB, Avgustin Čavić M, Ferluga D, Hvala A, Vizjak A (2005) C1Q nephropathy in children. Pediatr Nephrol 20:1756–1761
Wenderfer SE, Swinford RD, Braun MC (2010) C1q nephropathy in the pediatric population: pathology and pathogenesis. Pediatr Nephrol 25:1385–1396
Myllymäki J, Saha H, Mustonen J, Helin H, Pasternack A (2003) IgM nephropathy: clinical picture and long-term prognosis. Am J Kidney Dis 41:343–350
Bloom PM, Filo RS, Smith EJ (1976) Immunofluorescent deposits in normal kidneys (Abstract). Kidney Int 10:539
Wong CS, Fink CA, Baechle J, Harris AA, Staples AO, Brandt JR (2009) C1q nephropathy and minimal change nephrotic syndrome. Pediatr Nephrol 24:761–767
Pardo V, Riesgo I, Zilleruelo G, Strauss J (1984) The clinical significance of mesangial IgM deposits and mesangial hypercellularity in minimal change nephrotic syndrome. Am J Kidney Dis 3:264–269
Al-Eisa A, Carter JE, Lirenman DS, Magil AB (1996) Childhood IgM nephropathy: comparison with minimal change disease. Nephron 72:37–43
Zeis PM, Kavazarakis E, Nakopoulou L, Moustaki M, Messaritaki A, Zeis MP, Nicolaidou P (2001) Glomerulopathy with mesangial IgM deposits: long-term follow up of 64 children. Pediatr Int 43:287–292
Kanemoto K, Ito H, Anzai M, Matsumura C, Kurayama H (2013) Clinical significance of IgM and C1q deposition in the mesangium in pediatric idiopathic nephrotic syndrome. J Nephrol 26:306–314
Swartz SJ, Eldin KW, Hicks MJ, Feig DI (2009) Minimal change disease with IgM + immunofluorescence: a subtype of nephrotic syndrome. Pediatr Nephrol 24:1187–1192
Lau KK, Gaber LW, Delos Santos NM, Wyatt RJ (2005) C1qnephropathy: features at presentation and outcome. Pediatr Nephrol 20:744–749
Iskandar SS, Browning MC, Lorentz WB (1991) C1q nephropathy: a pediatric clinicopathologic study. Am J Kidney Dis 18:459–465
Fukuma Y, Hisano S, Segawa Y, Niimi K, Tsuru N, Kaku Y, Hatae K, Kiyoshi Y, Mitsudome A, Iwasaki H (2006) Clinicopathologic correlation of C1q nephropathy in children. Am J Kidney Dis 47:412–418
Development Core Team (2008) Available at: http://www.R-project.org
[No authors listed] (1981) The primary nephrotic syndrome in children. Identification of patients with minimal change nephrotic syndrome from initial response to prednisone. A Report of the International Study of Kidney Disease in Children. J Pediatr 98:561–564
[No authors listed] (1981) Primary nephrotic syndrome in children: clinical significance of histopathologic variants of minimal change and of diffuse mesangial hypercellularity. A Report of the International Study of Kidney Disease in Children. Kidney Int 20:765–771
Schulman SL, Kaiser BA, Polinsky MS, Srinivasan R, Baluarte HJ (1988) Predicting the response to cytotoxic therapy for childhood nephrotic syndrome: superiority of response to corticosteroid therapy over histopathologic patterns. J Pediatr 113:996–1001
Border WA (1988) Distinguishing minimal-change disease from mesangial disorders. Kidney Int 34:419–434
Cho MH, Hong EH, Lee TH, Ko CW (2007) Pathophysiology of minimal change nephrotic syndrome and focal segmental glomerulosclerosis. Nephrology (Carlton) 12[Suppl 3]:S11–S14
Silverstein DM, Craver RD (2008) Mesangial hypercellularity in children: presenting features and outcomes. Pediatr Nephrol 23:921–928
Couser WG (2012) Basic and translational concepts of immune-mediated glomerular diseases. J Am Soc Nephrol 23:381–399
Barisoni L, Schnaper HW, Kopp JB (2007) A proposed taxonomy for the podocytopathies: a reassessment of the primary nephrotic diseases. Clin J Am Soc Nephrol 2:529–542
Markowitz GS, Schwimmer JA, Stokes MB, Nasr S, Seigle RL, Valeri AM, D’Agati VD (2003) C1q nephropathy: a variant of focal segmental glomerulosclerosis. Kidney Int 64:1232–1240
Acknowledgments
We are grateful to Prof. Jadranka Buturović-Ponikvar and Assist. Prof. Andreja Marn Pernat for their assistance in providing patient records for clinical course in adulthood. Our sincere thanks also go to Anastazija Hvala for cooperating in the electron microscopy examinations of renal biopsies. Many thanks also to Mojca Čižek Sajko, Prof. Janez Stare and Rok Blagus for assisting in the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendices
Appendix 1. Definitions used to include patients in the study
-
MCNS: Clinical constellation of nephrotic range proteinuria, hypoalbuminemia, edema, hyperlipidemia, and pathohistological findings of minimal change disease on light microscopy with or without mesangial proliferation, C1q and/or IgM mesengial deposition on IF microscopy, and with or without foot process effacement on electron microscopy.
-
IgM nephropathy: ≥2+ (on a scale of 0–4+) dominant immunostaining for IgM, with a predominantly mesangial distribution. Exceptions were patients who had in addition to IgM, C1q staining grade of ≥2+. Those patients were included in the C1q nephropathy group.
-
MCNS with IgM nephropathy: MCNS with pathohistological characteristics of IgM nephropathy.
-
C1q nephropathy: ≥2+ (on a scale of 0–4+) immunostaining for C1q with a predominantly mesangial distribution, frequently accompanied by IgG and IgM, which may be less intense, equally intense, or more intense, in patients without evidence of SLE.
-
MCNS with C1q nephropathy: MCNS with pathohistological characteristics of C1q nephropathy.
-
Children: individuals aged 1–18 years.
Appendix 2. Definitions used for presentation of the disease
-
Nephrotic syndrome: Nephrotic range proteinuria, hypoalbuminemia, edema, and hyperlipidemia.
-
Nephrotic range proteinuria: Proteinuria exceeding 40 mg/m2/h.
-
Hypoalbuminemia: Serum albumin concentration below 30 g/l.
-
Edema: An abnormal accumulation of fluid beneath the skin or in one or more cavities of the body that produces swelling.
-
Hyperlipidemia: Elevation of lipids above the 95th percentile for patient age and gender.
-
Normal renal function: Normal values of calculated creatinine clearance for patient age and gender.
-
Decline in renal function: Values of calculated creatinine clearance below normal for patient age and gender.
-
Hypertension: Systolic and/or diastolic blood pressure above the 95th percentile based on a child’s gender, age, and height percentile.
-
Hematuria: An abnormal quantity of red blood cells in urine (more than 5 red blood cells per high-power field of spun urinary sediment), being either microscopic or macroscopic.
Appendix 3. Definitions used for clinical course and response to treatment
-
Remission: Proteinuria below 4 mg/m2/h or zero to trace albuminuria on dipstick on three consecutive days.
-
Relapse: Reappearance of nephrotic range proteinuria in a patient who was previously in remission.
-
Steroid-sensitive NS patients: Patients in whom proteinuria resolved within ≤6 weeks after initiation of steroid therapy. These were further subdivided into three groups:
-
Infrequently relapsing NS patients - patients who had no or less relapses than defined for the frequently relapsing NS patients during the first year of treatment.
-
Frequently relapsing NS patients - patients who had at least two relapses in a 6-month or at least 4 relapses in a 12-month period during the first year of treatment.
-
Steroid-dependent NS patients - patients who relapsed during steroid treatment or within 2 weeks after its cessation during the first year of treatment.
-
-
Steroid-resistant NS patients - patients in whom proteinuria did not resolve within ≥ 6 weeks after initiation of steroid therapy.
Appendix 4. Definitions used for the renal outcome
-
Complete remission: Proteinuria below 4 mg/m2/h and normal renal function at last follow-up.
-
Partial remission: Reduction in proteinuria of at least 50 % and stable renal function at last follow-up.
-
No remission, stable renal function: Continuous nephrotic range proteinuria and stable renal function at last follow-up.
-
No remission, progression of renal disease: Continuous nephrotic range proteinuria and decline in renal function at last follow-up.
-
End-stage renal disease: Need for chronic replacement therapy at last follow-up.
Rights and permissions
About this article
Cite this article
Vintar Spreitzer, M., Vizjak, A., Ferluga, D. et al. Do C1q or IgM nephropathies predict disease severity in children with minimal change nephrotic syndrome?. Pediatr Nephrol 29, 67–74 (2014). https://doi.org/10.1007/s00467-013-2551-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-013-2551-3